Transverse Intercalary
Transverse intercalary limb deficiencies are characterized by the absence of proximal or middle segments of a limb with all or part of the distal segment present (see Fig. 40). Radiographs are strongly recommended to confirm the condition and characterize the bony anatomy.
Fig. 40. Transverse intercalary

Diagnosis
Prenatal. Transverse intercalary limb deficiency can be suspected prenatally but can easily be missed or misdiagnosed. Cases identified or suspected prenatally should be confirmed postnatally before inclusion in a surveillance programme.
Postnatal. The newborn examination confirms the diagnosis of intercalary limb deficiencies and distinguishes it from other limb reduction defects. A careful clinical examination and documentation, aided by imaging (photos and radiographs), are essential for an accurate and complete diagnosis.
Clinical and epidemiologic notes
Note that the term “phocomelia”, associated in the past with these conditions, is now considered pejorative and should not be used (the word alludes to the shape of the limb resembling a flipper on a seal).
Typical intercalary deficiencies present with absence of all limb bones proximal to a normal or malformed hand or foot that attaches directly to the trunk. Atypical intercalary deficiencies present with absence of a humerus or femur, or both radius-ulna (tibia-fibula) with a normal or malformed hand or foot.
- About half of cases are isolated. Most of the remaining cases have multiple congenital anomalies. A small proportion of cases are syndromic.
- Syndromes with intercalary limb deficiencies include Roberts syndrome, and in its most severe form, thrombocytopenia absent radius (TAR) can have intercalary limb deficiencies.
- A teratogen that can cause intercalary limb deficiencies is thalidomide.
- Femoral hypoplasia-unusual facies syndrome (now more commonly called femoral-facial syndrome or FFS) is characterized by unilateral or bilateral deficiency of femurs, with variable deficiencies of other long bones. It has been reported in association with pregestational diabetes.
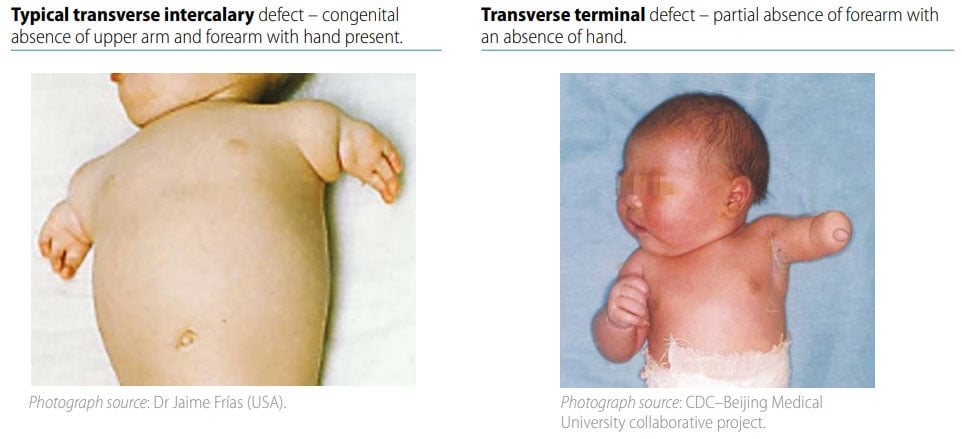
- Make sure that the distal part of the limbs (hand and foot) is intact. Only the proximal or middle segments of the limbs are affected in terminal intercalary defects. Carefully distinguish from terminal transverse defects, which look like an amputation (see Fig. 41).
- Take photographs and attach radiographs – the combined information is extremely helpful to confirm the diagnosis, characterize accurately the specific bones involved, and distinguish typical from atypical intercalary deficiencies.
Checklist for high-quality reporting
| Intercalary Defects – Documentation Checklist |
Describe in detail, including:
|
Fig. 41. Distinguishing intercalary defects from transverse terminal defects (side-by-side comparison)