4.2d Encephalocele (Q01.0–Q01.83, Q01.9)
Encephalocele is a NTD characterized by a pedunculated or sessile cystic, skin-covered lesion protruding through a defect in the cranium (skull bone). Encephaloceles can contain herniated meninges and brain tissue (encephalocele or meningoencephalocele) or only meninges (cranial meningocele), and can vary in location and size (see Fig. 4.6). The most common type of encephalocele is occipital (approximately 74%), followed by parietal (13%) encephalocele.
Encephalocele is more likely to occur with other unrelated structural anomalies or syndromes than either anencephaly or spina bifida.
Fig. 4.6. Encephalocele
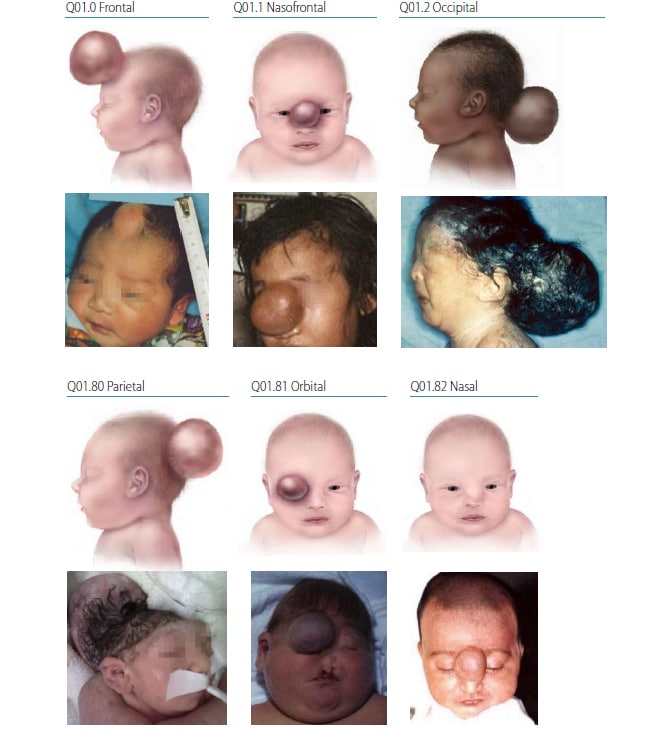
Photograph sources: CDC–Beijing Medical University collaborative project; Dr Jaime Frias.
Relevant ICD-10 codes
Q01.0 Frontal encephalocele
Q01.1 Nasofrontal encephalocele
Q01.2 Occipital encephalocele
Q01.80 Parietal encephalocele
Q01.81 Orbital encephalocele
Q01.82 Nasal encephalocele
Q01.9 Encephalocele, unspecified
Diagnosis
Prenatal. Encephalocele can be diagnosed prenatally using ultrasound, and might co-occur with a number of brain abnormalities such as Dandy Walker malformation or a Chiari malformation. Encephaloceles might be confused with the amniotic band spectrum of anomalies. For this reason, a prenatal diagnosis of encephalocele should always be confirmed postnatally. When this is not possible (e.g. termination of pregnancy or unexamined fetal death), the programme should have criteria in place to determine whether to accept or not accept a case based solely on prenatal data.
Postnatal. The newborn examination, x-ray and computed tomography (CT) or magnetic resonance imaging (MRI) confirm the diagnosis and distinguish it from the other anomalies that might involve the brain and cranium.
Clinical and epidemiologic notes
Distinguishing encephalocele from the other abnormalities of the brain and cranium is important because this condition has different causes and associated anomalies. The diagnosis of an encephalocele requires a careful examination with radiographs (to evaluate the intracranial connection) and imaging (MRI, CT scan to determine the content of the cephalocele).
Approximately 20% of infants diagnosed with an encephalocele will have at least one additional unrelated major birth defect. Encephaloceles are also known to occur in over 30 syndromes, which include both single-gene disorders (e.g. Meckel–Gruber syndrome) and chromosomal anomalies (e.g. trisomies 13 and 18). For this reason, it is crucial to report all findings and obtain good clinical photographs for the expert reviewer.
In the amniotic band spectrum, the skull and brain might resemble an “encephalocele”. However, the occurrence of other findings (facial schisis, limb and ventral wall anomalies, strands of amniotic sac tissue) points towards the diagnosis of an amniotic band disruption and allows the differentiation from encephalocele.
As with other NTDs, non-genetic risk factors might include pregestational diabetes, obesity, and hyperthermia (e.g. fever) in early pregnancy, and folic acid insufficiency/deficiency. Adequate preconceptional use of folic acid (as a supplement or through fortification) might prevent some cases of encephalocele.
The reported birth prevalence of encephalocele varies widely worldwide, with a range between 0.1 to 26.5 per 10 000 births. The location of the encephalocele also varies geographically. Most frequently, encephaloceles are located in the occipital area, except in South-East Asia, where anterior location (frontal or nasofrontal) is most common.
Inclusions
Q01.0 Frontal encephalocele
Q01.1 Nasofrontal encephalocele
Q01.2 Occipital encephalocele
Q01.80 Parietal encephalocele
Q01.81 Orbital encephalocele
Q01.82 Nasal encephalocele
Q01.83 Nasopharyngeal encephalocele
Q01.9 Encephalocele, unspecified
Exclusions
Q79.8 Amniotic band syndrome
Checklist for high-quality reporting
| Encephalocele – Documentation Checklist |
Describe in detail:
Report whether autopsy (pathology) findings are available and if so, report the results. |
Suggested data quality indicators
| Category | Suggested Practices and Quality Indicators |
| Description and documentation |
|
| Coding |
|
| Clinical classification |
|
| Prevalence |
|