Abdominal Wall Defects: Omphalocele
Omphalocele is a birth defect of the anterior abdominal wall, characterized by a centrally located and membrane-covered herniation of gut and possibly other organs (liver, spleen, stomach).
Fig. 48. Omphalocele

Photograph source: CDC–Beijing Medical University collaborative project.
Key findings in omphalocele (see Fig. 48):
- Location – the defect is central (not lateral) and the organs herniate through a dilated umbilical ring.
- Covering – organs are covered or contained by a membrane (not skin) and the umbilical cord inserts into the distal part of the sac. The membrane can be thin and translucent (panel a) or more opaque and nearly fibrous (panel b) due to in utero exposure to amniotic fluid. Note also that the membrane may be ruptured in utero or during birth (panel c).
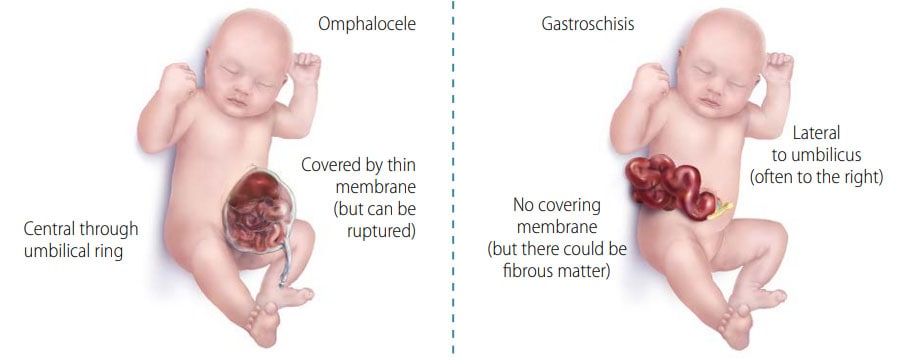
Note: Be sure not to confuse this condition with gastroschisis. In gastroschisis the abdominal defect is lateral to the umbilical cord and herniated organs are never covered by membrane (see Fig. 49).
Diagnosis
Prenatal. Always confirm the diagnosis postnatally – prenatal diagnosis is possible but is tricky, and misdiagnoses are not uncommon. Use programme rules (SOPs) to decide whether to accept prenatal diagnoses without postnatal confirmation (e.g. in cases of termination of pregnancy or unexamined fetal death).
Postnatal. A careful examination should be able to confirm or exclude the diagnosis. Differentiate from gastroschisis. Some other conditions can be confused with omphalocele but are much rarer and more complex (e.g. limb-body wall spectrum).
Clinical and epidemiologic notes
- With other unrelated birth defects, particularly cardiac, urogenital, brain, spina bifida.
- With certain complex anomaly patterns (OEIS [omphalocele, cloacal exstrophy, imperforate anus, spinal defects]).
- With some genetic syndromes, including trisomies 13 and 18, and Beckwith-Wiedemann syndrome.
- Always look for additional internal anomalies and syndromes.
- Note the size of the omphalocele – the bigger the size, the more likely the presence of anomalies and syndromes, the presence of liver in the sac, the complexity of treatment/surgery, and the risk for morbidity, mortality, disability.
Checklist for high-quality reporting
| Omphalocele – Documentation Checklist |
Describe in detail: Avoid just using the term “omphalocele” but add further details:
|
Fig. 49. Distinguishing omphalocele from gastroschisis