Spina Bifida
Spina bifida is an NTD characterized by herniation of meninges and spinal cord (Fig. 6, panel a: myelomeningocele) or meninges only (Fig. 6, panel b: meningocele). Lesion can be open or closed. Hydrocephalus is a common complication, especially among children with open myelomeningocele. Figs. 7–10 show the different spina bifida lesion levels.
Fig. 6. Spina bifida
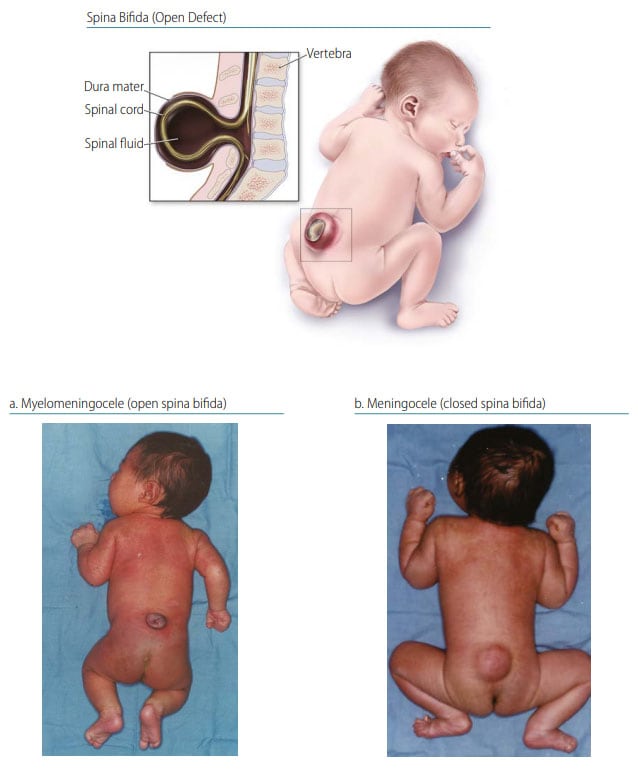
Photograph source: CDC–Beijing Medical University collaborative project.
Fig. 7. Cervical spina bifida

Photograph source: CDC–Beijing Medical University collaborative project.
Fig. 8. Thoracic spina bifida

Photograph source: CDC–Beijing Medical University collaborative project.
Fig. 9. Lumbar spina bifida
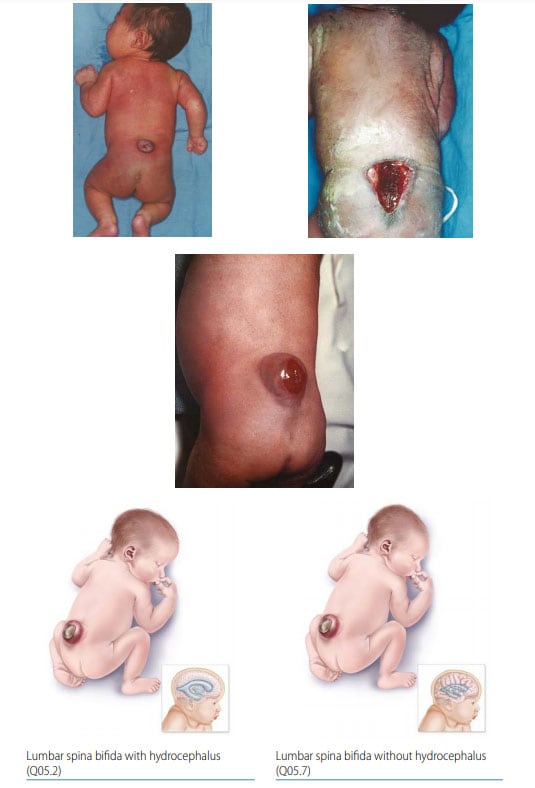
Photograph sources: CDC–Beijing Medical University collaborative project; Idalina Montes, MD, and Rafael Longo, MD, FACS, Puerto Rico.
Fig. 10. Sacral spina bifida
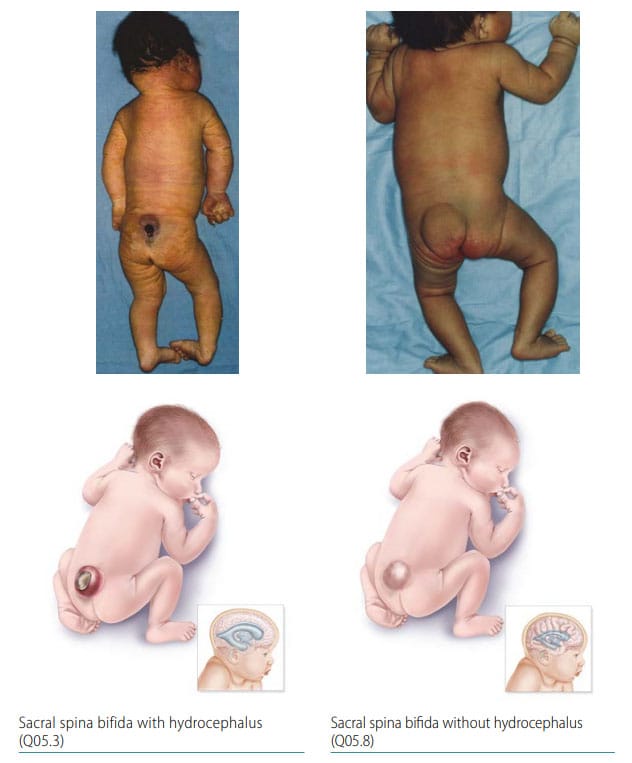
Photograph source: CDC–Beijing Medical University collaborative project.
- Location – level of the lesion; that is, lumbar spine (the most common location), followed by sacral, thoracic and cervical.
- Covering – open, non-skin covered (myelomeningocele) represents 90% of spina bifida; 10% have a closed lesion (meningocele – containing only meninges and cerebral spinal fluid).
- Size – can vary from single vertebral to multiple levels (thoracic-lumbar).
Diagnosis
Prenatal. Spina bifida might be diagnosed prenatally using ultrasound, but distinguishing if the lesion is open or closed can be challenging. Maternal serum screening might help to determine an open versus a closed lesion. Use programme rules (SOPs) to decide whether to accept prenatal diagnoses without postnatal confirmation (e.g. in cases of termination of pregnancy or unexamined fetal death).
Postnatal. The newborn examination usually confirms the diagnosis. Imaging (when available) can provide additional information to characterize the location, extent and content of the lesion, as well as the presence or absence of frequently co-occurring brain findings (e.g. hydrocephalus, Chiari II malformation).
Clinical and epidemiologic notes
- Chiari II malformation and hydrocephalus.
- Hip dislocation, talipes, lower limb paralysis.
- Loss of sphincter control, including neurogenic bladder.
- Always look for additional anomalies and syndromes (trisomy 18).
- Occurs in OEIS complex (omphalocele–exstrophy of the bladder–imperforate anus–spinal defects).
- Review examinations, procedures and imaging – rare conditions misdiagnosed as spina bifida include spina bifida occulta, sacrococcygeal teratoma, isolated scoliosis/kyphosis, and amniotic band syndrome.
- Lipomeningo(myelo)cele is a rare type of spina bifida with an overlying lipoma; many programmes do not include lipomeningo(myelo)celes as an NTD.
Checklist for high-quality reporting
| Spina Bifida – Documentation Checklist |
Describe defect in detail:
Take and report photographs: Show clearly the level of spina bifida (back and side if possible); can be crucial for review. Describe evaluations to find or rule out related and associated anomalies:
Report whether autopsy (pathology) findings are available and if so, report the results. |