7.8 Quality and “Waste” in Surveillance
It is well recognized that health care, in its current state, has a quality problem – and specifically, large amounts of “waste”. Waste here is a technical term that addresses a significant problem in the production of a service through a series of linked processes. Waste is an activity that does not add value to the final product.
The key insight here is that a crucial way to improve quality is to reduce waste. Waste is everywhere in health care – preventable errors are made every day, causing harm, and creating complications leading to hospitalizations and illnesses. In surveillance, waste is likely everywhere – data are stalled in one or more processes and delay timeliness, cases are missed because of inadequate physical examination or lack of good data sources (e.g. for stillbirths), cases are miscoded and misclassified leading to inaccurate reports and interpretation.
A programme team that wishes to improve quality should investigate such sources of waste and find ways to intervene. The first steps have already been made, leading to a clear visual map of the processes. The elements of data quality can then be tracked across some or all processes using measurable indicators for completeness, accuracy and timeliness.
The search for “waste” needs to start with an understanding of the common types that occur in health care and surveillance. The two most common types are quality waste and inefficiency waste.
Quality waste includes anything in the process that produces a flawed product, or any step in the process that does not add value to the final product. Another type of waste is inefficiency waste, which looks at two processes that generate the same product at different costs; the process that has the higher cost is comparatively inefficient. A major emphasis in industry and health care in recent decades has been not so much to decrease costs but to increase quality at a reasonable cost.
For a surveillance programme, the system is structured as a series of linked processes, aimed at producing a specific product. The product is a specific kind of information, but a product nonetheless. Like any other system, these processes have issues of efficiency, quality and potentially wasted resources. As shown in Fig. 7.8, cases in a birth defects surveillance programme might be missed, miscoded or misclassified.
Fig. 7.8. Quality waste in surveillance
Quality waste in surveillance: solution is to find and fix
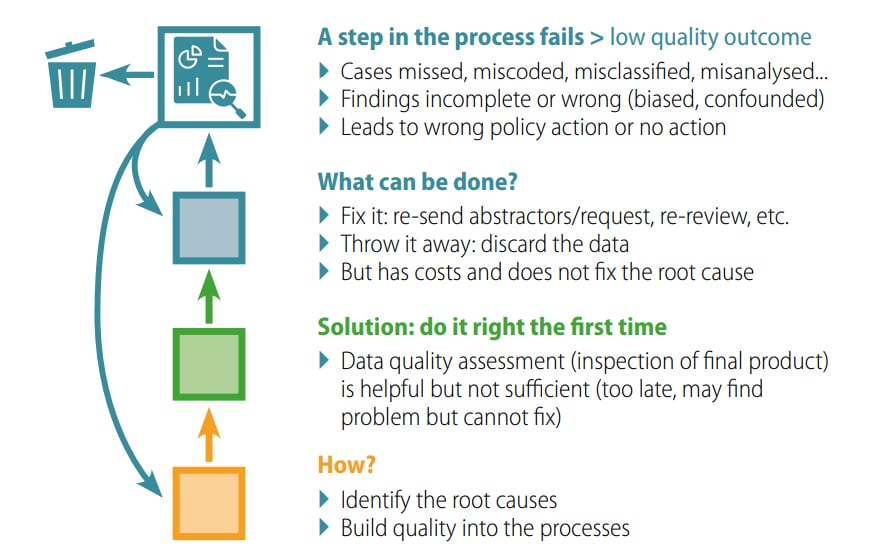
Fixing the errors can be time and resource intensive, which might require the front-line staff to go back and re-abstract information, clinicians to re-review sets of cases with updated information, and so on. At times the errors might not be fixable; for example, if the primary records are flawed and there is no longer access to the infant, the case data might need to be discarded.
Some lessons can be gleaned so far:
- Quality assessment is critical but not sufficient. Quality assessment relies on an inspection of the final product, and if a programme waits until the final product, it might be too late to fix the issues.
- Quality assessment might identify the problem, but cannot solve it. In fact, in most cases, finding a flawed product does not even reveal the origin of the problem.
So, if quality assessment does not directly translate to better quality, what is the solution? The solution lies in first diagnosing the root causes of the quality problem and then treating it. To do so effectively requires a deep understanding of the processes in the production system. Such understanding comes from a careful and detailed process mapping developed by a team that involves all key staff, including the front-line staff and other personnel who have a fundamental knowledge of the system.
These strategies aim at finding the root causes of quality issues, which in turn helps to identify leverage points for improvement, where small changes can lead to significant increases in quality. For example, if the primary data on birth defects from the physical examination are inaccurate or incomplete, focused training of front-line staff together with systematic use of checklists can lead to large improvements in data quality.
To summarize, quality must not only be checked at the end, it must be built into – embedded into – each step of the process. There is ample justification for intentional and sustained efforts at assessing and improving data quality in public health surveillance. Surveillance generates data for action, and if the data are inaccurate, incomplete or untimely, the benefits of surveillance for public health are curtailed and limited resources are wasted. This primer briefly presents a broad overview of selected issues, such as defining data collected based on programme goals; developing SMART goals that provide meaningful operational guidance to the system; focusing on data quality attributes of completeness, accuracy and timeliness; and finally, mapping the key processes of the surveillance system. Programmes are encouraged to seek out available training and resources for quality improvements.