Congenital Cytomegalovirus
Background
Cytomegalovirus (CMV) is a very common herpesviridae virus. Most people will be infected at some point during their lifetime. CMV is transmitted through close person-to-person contact with infected secretions, including urine, saliva, blood transfusions, semen, cervical secretion and breast milk. Congenital cytomegalovirus infection (cCMV) occurs when the CMV crosses the placenta during pregnancy and infects the fetus. The highest risk of fetal infection is among mothers experiencing a primary infection during the first or second trimester of pregnancy. Women who are immunocompromised – for example, with HIV infection – have higher rates of fetal transmission.
Main clinical manifestations in the mother
CMV infection is very common and in most healthy people presents with mild flu-like symptoms or is asymptomatic (subclinical infection).
Main clinical manifestations in the infant
Most infants with cCMV will not have signs or symptoms of cCMV disease at birth and will remain well. Infants born with symptoms – which might include growth restriction, ascites/hydrops, hepatosplenomegaly, jaundice, petechiae, hepatitis (raised transaminases or bilirubin), thrombocytopenia, anaemia, microcephaly, seizures, chorioretinitis and sensorineural hearing loss – are at the highest risk of poor neurodevelopmental outcomes. Rarely, infants with cCMV have severe microcephaly that is characterized by marked reduction in cranial vault height with overlapping sutures and redundant scalp with rugae or folds. This presentation is indistinguishable from CZS by physical examination alone.
Long-term sequelae: While the majority of infants born with cCMV will not have any long-term sequelae, 10–20% will go on to have neurodevelopmental disabilities, including sensorineural hearing loss, epilepsy, cerebral palsy, visual impairment and learning difficulties. CMV is the most common infectious cause of sensorineural hearing loss and neurodevelopmental abnormalities in high-income settings, and is likely more common, but under-identified, in low-resource settings. cCMV is a known cause of stillbirth and neonatal death.
Relevant ICD-10 codes
P35.1 Congenital cytomegalovirus infection (CMV)
Fig. 55. Clinical findings in the infant

Petechial rash (blueberry muffin rash) and jaundice in infant with cCMV.
Photograph source: Jacob Johan.

Infant born with cCMV. Note severe microcephaly and lower limb spasticity similar to features of severe congenital Zika infection.
Photograph source: CDC Public Health Image Library.
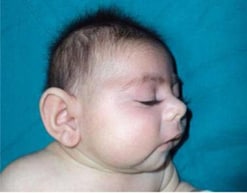
Microcephaly in an infant with cCMV.
Photograph source: Işikay S, Yilmaz K. Congenital cytomegalovirus infection and finger anomaly. Case Reports. 2013;2013:bcr2013009486.
Checklist
| Checklist |
|