Longitudinal Axial Defects – Split Hand and Foot
A longitudinal deficiency of the central digits/toes often involving the associated carpal/tarsal bones leads to a split-hand or splitfoot appearance (see Fig. 44). Radiographs are strongly recommended to confirm and further characterize the condition.
Fig. 44. Longitudinal axial defects (split hand and foot)

Photograph source: CDC–Beijing Medical University collaborative project.
Diagnosis
Prenatal. Split hand/foot can be suspected prenatally but can easily be missed or misdiagnosed. Cases identified or suspected prenatally should be confirmed postnatally before inclusion in a surveillance programme.
Postnatal. The newborn examination confirms the diagnosis of split hand and foot and distinguishes it from other limb reduction defects (e.g. transverse terminal defects with amputation of digits or toes). It is important to underline the need for a proper examination of cases, in order to confirm the absence of the axial segment of the hand or foot. For these purposes, a radiological examination is essential.
Clinical and epidemiologic notes
The terms “ectrodactyly” and “lobster claw hands” are imprecise and pejorative and should not be used. The anatomic distribution can be hands only, feet only, or affected hands and feet. The hands are affected much more frequently than the feet. In many cases of split hand/foot, there is syndactyly and hypoplasia of some of the remaining digits. The most severe form of split hand/foot is monodactyly, where the hand or foot has but a single digit.
- Split hand/foot may be isolated, or there may be deficiency of the adjacent long bones of the limbs.
- Split hand/foot is part of a large group of syndromes, some with overlapping features. The most common of these is EEC syndrome (ectrodactyly, ectodermal dysplasia and cleft lip/palate). Another syndrome with split hand/foot is limb-mammary syndrome (split hand/foot, absence of breast tissue, cleft palate).
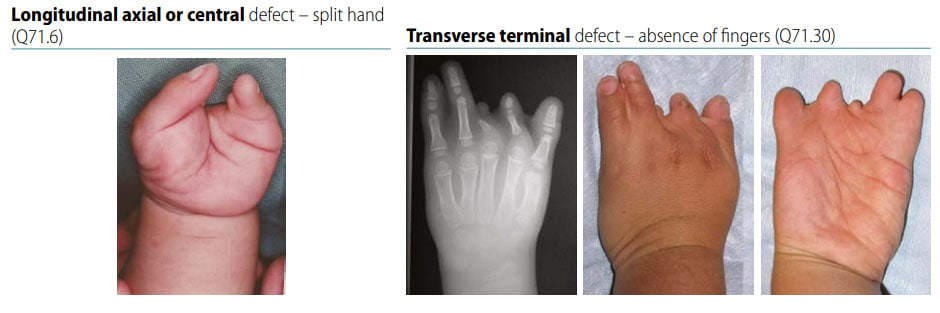
- Make sure that the central segment of the hand or foot is affected – third digit/toe, with or without involvement of second and fourth digit/toe. Carefully distinguish from transverse terminal defects affecting the same digits/toes (see Fig. 45).
- Radiographs are useful to confirm and describe which specific bones are involved in the defect.
- Consider additional procedures to assess syndromes (e.g. skin examination, oral clefts), which are not uncommon in longitudinal axial defects.
Checklist for high-quality reporting
| Split Hand and Foot – Documentation Checklist |
Describe in detail, including:
|
Fig. 45. Distinguishing longitudinal axial defects from transverse terminal defects of hand (side-by-side comparison)
Photograph source: CDC–Beijing Medical University collaborative project.