Longitudinal Postaxial (Fibula, Ulna, Fifth Ray)
Longitudinal postaxial defects include absence or hypoplasia of the fifth toe/finger (sometimes including the fourth toe/finger), and absence/hypoplasia of the fibula or ulna (see Fig. 46). Radiographs are strongly recommended to confirm and further characterize the condition.
Fig. 46. Longitudinal postaxial

Photograph source: ECLAMC.
Diagnosis
Prenatal. Longitudinal postaxial defects can be suspected prenatally but can easily be missed or misdiagnosed. Cases identified or suspected prenatally should be confirmed postnatally before inclusion in a surveillance programme.
Postnatal. The newborn examination confirms the diagnosis of longitudinal postaxial limb deficiencies and distinguishes it from other limb reduction defects (e.g. longitudinal preaxial defects). It is important to underline the need for a proper examination of cases, in order to confirm the absence of the postaxial segment of the upper or lower limb. For these purposes, a radiological examination is essential.
Clinical and epidemiologic notes
Absence or hypoplasia of the ulna is much more likely to be a partial deficiency affecting only one arm. With complete absence of the ulna there is often a marked flexion deformity of the elbow. The hand can be straight or angulated to the ulnar side of the wrist. Ulnar deficiency is less common than radial deficiency.
- Ulnar hypoplasia is often associated with radioulnar synostosis (fusion of the radius and ulna), absence of the postaxial digits(fourth and fifth fingers) and fibular deficiency.
- Two associations with postaxial defects have been identified:
- The unilateral absence or hypoplasia of the ulna, femur and fibula (femur-fibula-ulna complex).
- The ulnar-mammary syndrome, in which there are deficiencies of the ulna, fibula and postaxial digits; hypogenitalism; and absence of one or both breasts.
- Postaxial limb defects of the hand occur in Miller syndrome.
- Make sure that the postaxial side of the limb is affected: absent fifth finger with or without fourth finger, ulna (upper limb); absent fifth with or without fourth toe, fibula (lower limb). Carefully distinguish from preaxial defects (see Fig. 47).
- Radiographs are useful to confirm and describe which specific bones are involved in the defect.
- Look for femoral deficiency, a feature of the femur-fibula-ulna complex.
Checklist for high-quality reporting
| Longitudinal Postaxial Defects – Documentation Checklist |
Describe in detail, including:
|
Fig. 47. Distinguishing longitudinal postaxial defects from longitudinal preaxial defects (side-by-side comparison)
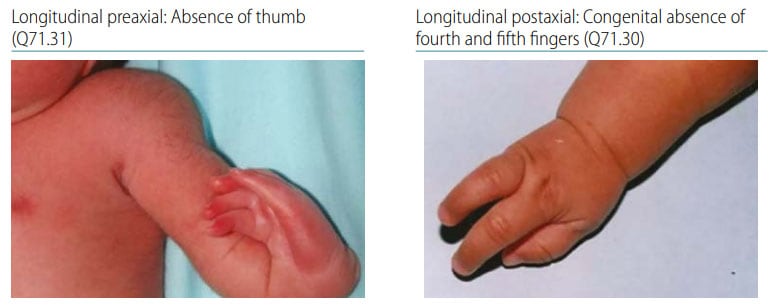
Photograph source: ECLAMC