Gastroschisis
Gastroschisis is an abdominal defect, with herniation of gut and possibly liver and other organs.
Fig. 50. Gastroschisis
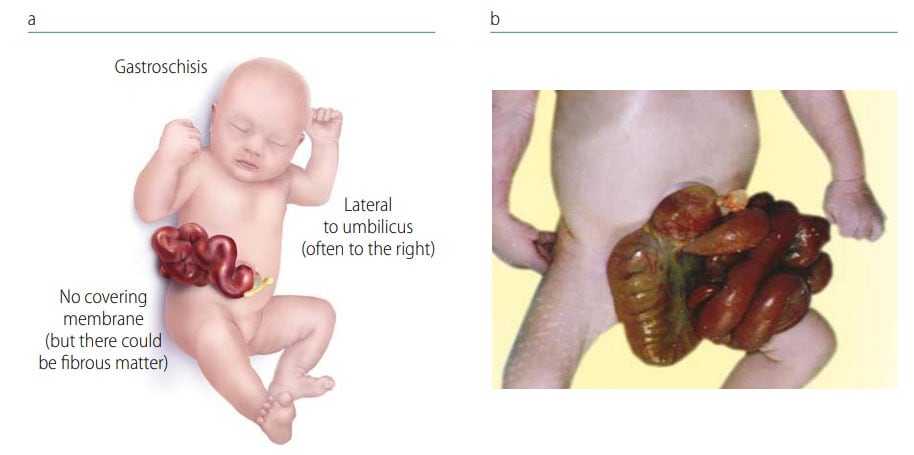
Photograph source: CDC–Beijing Medical University collaborative project.
Key findings in gastroschisis (see Fig. 50):
- Location – the defect is just to the side of (lateral to) the inserted umbilical cord (and generally to the right).
- Covering – there is no covering membrane, and the organs are exposed (at times these can covered by fibrous material due to in utero exposure to fluids).
Note: Be sure not to confuse this condition with omphalocele. In omphalocele, the organs (a) herniate centrally through a widened umbilical ring and (b) are covered by a thin, typically translucent membrane (not skin) that may, however, be ruptured (see Fig. 51 and Table 3).
Diagnosis
Prenatal. Always confirm the diagnosis postnatally – prenatal diagnosis is possible but is tricky, and misdiagnoses are not uncommon. Use programme rules (SOPs) to decide whether to accept prenatal diagnoses without postnatal confirmation (e.g. in cases of termination of pregnancy or unexamined fetal death).
Postnatal. A careful examination should be able to confirm or exclude the diagnosis. Differentiate from omphalocele. Some other conditions can be confused with gastroschisis but are much rarer and more complex (e.g. limb-body wall spectrum).
Clinical and epidemiologic notes
Gastroschisis is most often an isolated, non-syndromic anomaly. There can be other anomalies of the gut (which are not considered associated but related), but usually not of other organs. Arthrogryposis (multiple contractures) can occur in a small fraction of babies with gastroschisis. Diagnostic confusion can arise with omphalocele, which has a much higher proportion of associated anomalies and syndromes.
- If the child has a syndrome (e.g. trisomy 21 or 18), very probably it is not gastroschisis – review and document.
- If the child has gastroschisis, look for related anomalies, especially of the gut – intestinal malrotation, small intestinal atresia, microcolon. Assess for pulmonary hypoplasia. These related anomalies can affect survival and long-term function.
Checklist for high-quality reporting
| Gastroschisis – Documentation Checklist |
Describe in detail. Avoid using only the term “gastroschisis”; specify the following details:
|
Fig. 51. Distinguishing omphalocele from gastroschisis
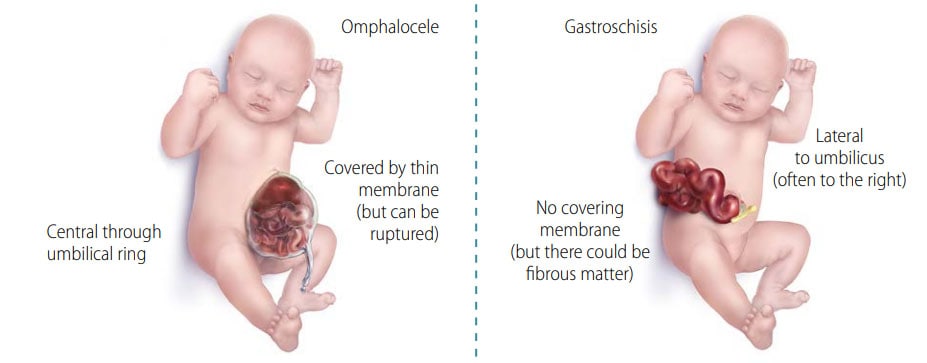
| Omphalocele | Gastroschisis | |
| Location | Within umbilical cord (central) | Lateral (R>>L) to intact umbilical cord |
| Covered by membrane | Yes (but can be ruptured) | Never (but surface can be matted) |
| Extruded viscera | Gut, +/– stomach, liver, etc. | Gut, occasionally other organs |
| Associated anomalies | Common (including syndromes) | Rare (syndromes very rare) |
 Photograph source: ECLAMC. |
 Photograph source: ECLAMC |