7.9 Simple Tools to Improve Data Quality
Simple tools to improve data quality
Two simple tools that can benefit birth defects surveillance programmes are checklists and data quality indicators.
Using checklists
Checklists have been used in high-reliability, high-complexity organizations and settings – for example, by pilots and surgeons. Checklists help users focus on key tasks, even simple tasks (for example, hand washing in surgery). Checklists help avoid errors, improve data quality, and increase efficiency, especially in busy or charged environments where pressure and distractions can be significant.
In birth defects surveillance, checklists can be developed at various steps of the processes – ascertainment, clinical case review, analysis, and so on. A particularly important step is the collection of primary data on birth defects at the point of care. None of the other steps in surveillance can obviate the lack of high-quality primary data – especially a detailed description and appropriate documentation of the birth defect.
Training front-line staff and abstractors to use (and if necessary, tailor) a simple but complete checklist is an inexpensive and highly valuable tool for enhancing quality. It also speaks to the main theme of quality improvement, which is to embed quality in each step of the surveillance system and not wait until the end of the process.
A checklist should be simple and practical. An example of a checklist for gastroschisis is shown below that includes a few clearly stated items. Using checklists requires training to ensure that all terms and items are understood.
| Gastroschisis – Documentation Checklist |
|
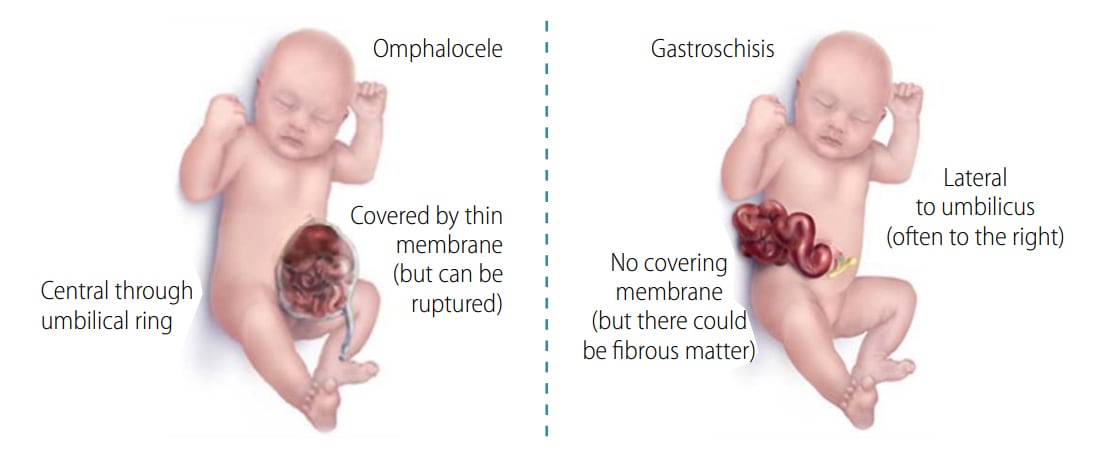
Such a checklist can be improved by integrating visual aids, which can be especially useful for differentiating complex or potentially confusing defects. For instance, the following visual aid can help distinguish gastroschisis from omphalocele (see Fig. 7.9).
Fig. 7.9. Visual aid for differentiating omphalocele and gastroschisis
The checklists developed for high-quality description and documentation of selected birth defects are available in Chapter 4, where the conditions are fully described.
Using data quality indicators (DQI)
A second set of tools for data quality is data quality indicators (DQI), which can be used to assess the quality of the “end product” of surveillance – the data. DQI can: (1) assist programmes to focus on areas needing improvement; (2) support data users in interpretation of findings; and (3) provide help in detection of variations (positive or negative) over time and among different sources or sites.
DQI for birth defects surveillance have been proposed by birth defects networks such as the European Network of Population-Based Registries for the Epidemiological Surveillance of Congenital Anomalies (EUROCAT) and the NBDPN. These are useful but tend to be more helpful for surveillance systems in high-resource areas or for specific uses within those networks. Because of the wider focus of the ICBDSR, which includes programmes operating in low-resource settings, a team of ICBDSR members developed a DQI tool that can be used more broadly.
These DQI include four domains that can be mapped to the main processes of a surveillance system: (1) description/documentation, (2) coding, (3) clinical classification and (4) analysis of prevalence (which reflects ascertainment). An example of DQI for gastroschisis is shown below.
| Category | Quality Indicators for Gastroschisis |
| Description and documentation | Review sample for documentation of key descriptors:
|
| Coding |
|
| Clinical classification |
|
| Prevalence |
|
Whereas these DQI can be assessed at the central or programme coordination level, some can be embedded within each step so that potential lapse in quality can be promptly detected and corrected.
DQI for selected birth defects, corresponding to the checklists described above, are also included in Chapter 4. Such sets of DQI can be embedded in easy-to-use tools. An example of an Excel-based tool is freely available for download at http://www.icbdsr.org/data-quality-indicators-tool/ external iconand is further explained in Appendix K. Using this tool, a surveillance programme can input its own data and systematically apply the DQI on specific birth defects. Surveillance programmes can also incorporate these DQI into their data management system to facilitate routine checks.