4.2a Anencephaly (Q00.0)
Anencephaly is a condition characterized by a total (holo) or partial (mero) absence of the brain with absence of the cranial vault (calvarium) and covering skin. Anencephaly is a NTD that results from a failure of the anterior (rostral) portion of the embryonic neural tube (anterior neuropore) to close properly. Many affected fetuses are either stillborn or die shortly after birth. In locations where prenatal diagnosis is prevalent and termination of pregnancy is permitted, fetuses with anencephaly might be missed if surveillance does not include this outcome. The calvarial defect extends through the foramen magnum in infants with holoanencephaly (Fig. 4.2, panel a – total absence), which is more common than meroanencephaly (Fig. 4.2, panel b – partial absence) in which the foramen magnum is not involved.
Relevant ICD-10 codes
Q00.0 Anencephaly
Diagnosis
Prenatal. Anencephaly is readily diagnosed. However, anencephaly could be confused with craniorachischisis, acrania or amniotic band syndrome. For this reason, a prenatal diagnosis of anencephaly should always be confirmed postnatally. When this is not possible (e.g. termination of pregnancy or unexamined fetal death), the programme should have criteria in place to determine whether to accept or not accept a case based solely on prenatal data.
Postnatal. The newborn examination confirms the diagnosis and will distinguish anencephaly from the other rare anomalies that might involve the brain and cranium. In anencephaly, the eyes are normally formed but tend to bulge as a result of the absent frontal portion of the cranial vault. The cerebellum, brain stem and spinal cord are intact.
Clinical and epidemiologic notes
Distinguishing anencephaly from the other abnormalities of the brain and spinal cord is important because these conditions have different causes and associated anomalies. With careful examination, the diagnosis of anencephaly is straightforward. Rare conditions that might be misdiagnosed as anencephaly include acrania, acephaly, and atypical “anencephaly” in amniotic band spectrum.
Acrania is a term that refers to acalvaria, or absence of the neurocranium (calvarial bones, dura mater and associated muscles), and is thought to be unrelated to NTDs. However, in some countries, the term acrania is used synonymously with the term anencephaly, so it is important to review clinical findings to ensure appropriate classification. Acephaly – absence of the head – is part of a pattern seen in acardiac twins. In the amniotic band spectrum and limb-body wall spectrum, the skull and brain might be affected in a way that resembles an unusual form of “anencephaly”. However, there are often other findings (facial schisis, limb and ventral wall anomalies, bands) that make the diagnosis straightforward and allow the differentiation from typical anencephaly.
Anencephaly is a fatal condition with rare survival past the first few days of birth and is often an isolated (approximately 70–80%), non-syndromic anomaly. For this reason, it is crucial to report all findings and obtain good clinical photographs for the expert reviewer. Anencephaly is reported to occur more commonly in females.
Non-genetic risk factors include pregestational diabetes, folate insufficiency/deficiency, obesity, and hyperthermia (e.g. fever) in early pregnancy. Adequate periconceptional use of folic acid (as a supplement or through fortification) can prevent most cases of anencephaly.
The birth prevalence of anencephaly varies widely, between 0.8 to 16 per 10 000 births. Median prevalence, when stratified by country income level, decreases with increasing income categories. Prevalence is also higher among areas without mandated folic acid fortification of foods.
Inclusions
Q00.0 Anencephaly
Note that holoanencephaly and meroanencephaly are coded the same and are counted together.
Exclusions
Acrania, acephaly: These have the same code as anencephaly (Q00.0) but must be excluded from prevalence counts of anencephaly.
Q00.1 Craniorachischisis
Q00.2 Iniencephaly
Q00.20 Iniencephaly, open
Q00.21 Iniencephaly, closed
Fig. 4.2.Types of anencephaly
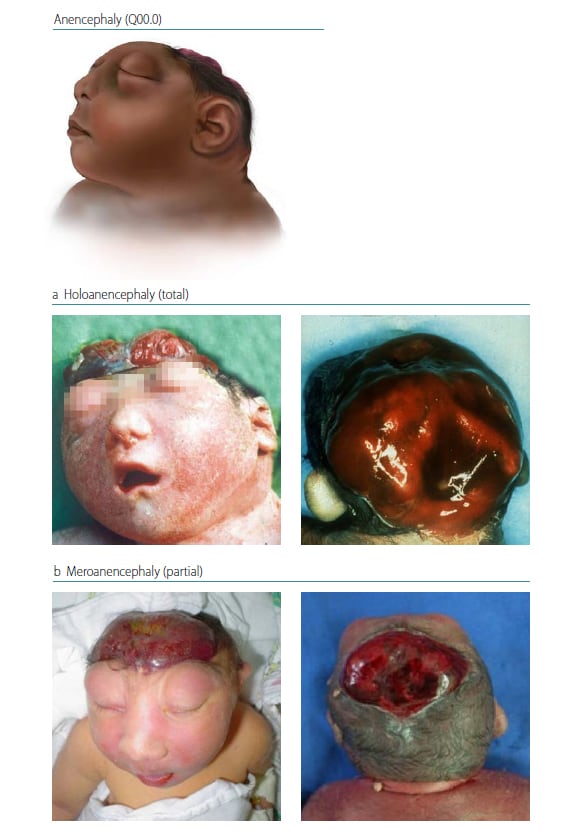
Source: CDC
Checklist for high-quality reporting
| Anencephaly – Documentation Checklist |
Describe defect in detail:
Report whether autopsy (pathology) findings are available and if so, report the results. |
Suggested data quality indicators
| Category | Suggested Practices and Quality Indicators |
| Description and documentation |
|
| Coding |
|
| Clinical classification |
|
| Prevalence |
|