3.2 Population Coverage
On this Page
Expected time: 2 hours
This section focuses on why birth prevalence and not incidence is the recommended form of reporting the frequency of congenital anomalies. First, let’s distinguish between incidence, prevalence and birth prevalence of congenital anomalies.
Incidence
Incidence refers to all new cases of congenital anomalies within a time period and within a given population. Incidence is not usually used to describe the occurrence of congenital anomalies. It is not possible to capture a true incidence, since not all conceptuses (products of conception at any time between fertilization and birth) can be ascertained – for example, because of early spontaneous abortions.
Prevalence
Prevalence is a measure of the total number of existing cases of a disease or condition for a given point in or period of time, and in a given population, regardless of whether or not they are new cases.
The following expression is used to calculate the birth prevalence of congenital anomalies, with the assumption that both live births and late fetal deaths are being captured:
Birth prevalence = a/b × 10 000
- a = Number of live births and late fetal deaths (stillbirths) with a specific congenital anomaly (e.g. spina bifida) counted among the source population in a given year
- b = Number of live births and late fetal deaths (stillbirths) during the same year
In order to calculate total prevalence in a population-based congenital anomalies surveillance system, the numerator includes cases among live births, known fetal deaths and pregnancy terminations (if possible). The denominator comprises the total number of subjects evaluated, including those cases in the numerator. However, if the total number of fetal death subjects or elective terminations of pregnancy for fetal anomaly (ETOPFA) is unknown, the total number of live births (and stillbirths if available) can be used. This is because the numerator of ETOPFA (and/or stillbirths) is relatively small, compared with the number of live births, and its exclusion from the denominator has little effect on the prevalence estimate. Spontaneous abortions (also called miscarriages) are not included in either the numerator or the denominator because it is practically impossible to assess the total number of spontaneous abortions.
Birth prevalence includes a specific timeframe; the estimate is for babies being born during a defined period of time.
Ask participants to provide responses aloud.
Types of Surveillance Programmes
There are two main types of surveillance programmes that may be used for congenital anomalies surveillance: population-based and hospital-based programmes.
Population-based programmes collect data from the entire population (all mothers giving birth either within or outside of a maternity facility, in a defined geographic area). The denominator would be the total number of births (live births and stillbirths).
- Inclusion is typically defined by the maternal residence.
- For example, a woman giving birth in the catchment area but residing elsewhere would not be considered a resident. Therefore, the fetus or neonate would not be included for surveillance or in the total number of births.
- Alternatively, a woman who gives birth outside the catchment area, but who maintains a permanent residence in the catchment area, would be considered a resident mother. Therefore, the fetus or neonate would be included for surveillance and in the total number of births.
- It is important to note that the surveillance system would need a mechanism to identify and exclude records of non-eligible mothers/births.
- Also, the surveillance system would need a mechanism to capture births to residents identified with congenital anomalies outside of the catchment area, such as in treatment centres, paediatric wards, rehabilitation centres or any other health facility. Therefore, more resources are needed to ascertain all fetuses or neonates with congenital anomalies. Programmes will need to have a mechanism in place to ensure that fetuses/neonates identified with a congenital anomaly and reported from more than one source are not counted twice (e.g. having a report from the delivery hospital and a report from a treatment centre).
Hospital-based programmes collect data from births that occur in pre-selected hospitals within a well-defined geographic area.
- Fetuses and neonates delivered at home would not be included, even if identified later in life in participating hospitals.
- Hospital-based programmes may be vulnerable to referral bias, since some hospitals may have particular characteristics.
- Hospital births may only be common among families with higher socioeconomic status.
- Hospital births may be more common among women who have been identified as being at high risk for a complicated birth.
- Prevalence estimates may not be accurate if they rely solely on hospital-based programmes.
- In countries where nearly all births take place in the hospital and all hospitals participate, those hospital-based programmes can closely approximate true prevalence.
A country’s selection between population-based and hospital-based surveillance programmes will depend on available resources and capacity. Both populationbased and hospital-based programmes may have a short period of time to diagnose a condition in a neonate, since neonates are discharged within hours or days following birth. Congenital anomalies that are commonly identified after the neonatal period, such as congenital heart defects, are often not diagnosed in a hospital setting, unless the programmes have resources to conduct follow-up with children after discharge from the birth hospital.
If a hospital-based programme is being implemented, selection of hospitals may include:
- Hospitals with a willingness to participate
- History of reporting other conditions to the ministry of health
- Hospitals that have a log book in place with an indicator of the presence or absence of a congenital anomaly in the delivery ward and other sources (such as paediatric wards and neonatal wards), as appropriate
- Hospitals with a high number of births
Note:It will be important to closely monitor the quality of reporting of participating hospitals.
Activity 3.1
Ask participants to refer to Activity 3.1 worksheet in the Participant Workbook pdf icon[457 KB, 21 Pages, Print Only].
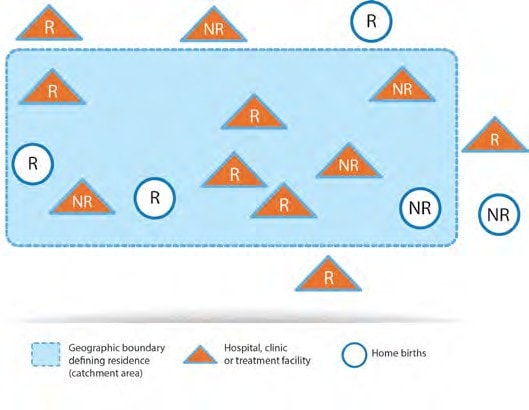
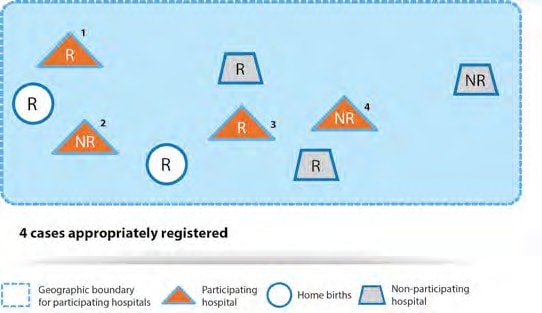
Illustration A
R = fetus or neonate with congenital anomaly whose mother is a resident.
NR = fetus or neonate with congenital anomaly whose mother is a non-resident.
The figure represents a population-based programme.
Yes it is; all neonates with congenital anomalies should be included if the mother is a resident.
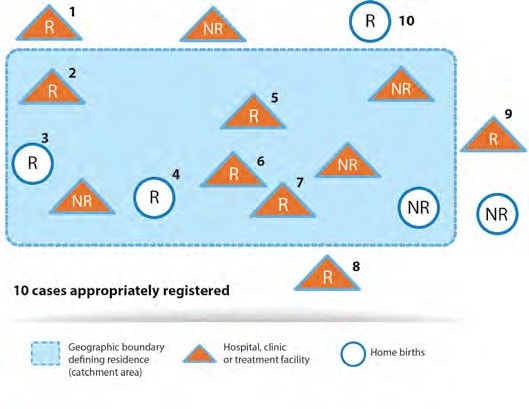
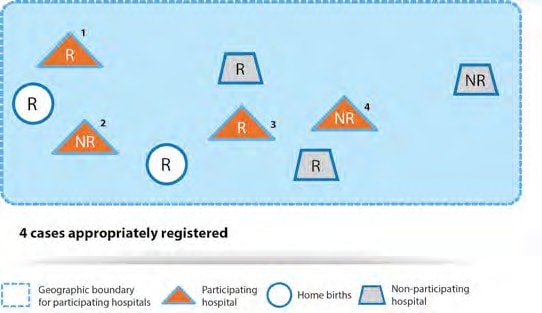
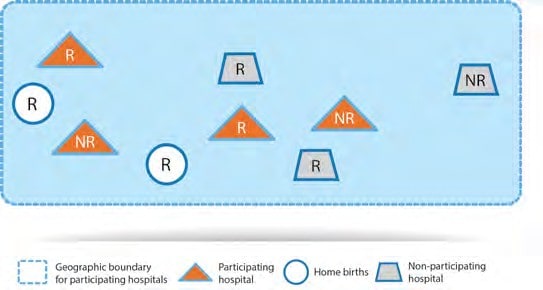
Illustration B
R = fetus or neonate with a congenital anomaly whose mother is a resident; included if the fetus or neonate is identified at a participating hospital.
NR = fetus or neonate with a congenital anomaly whose mother is a non-resident; included if the fetus or neonate is identified at a participating hospital.
The figure represents a hospital-based programme.
4; births that occur in the four participating hospitals shown in the figure.
No, it is not; neonates with congenital anomalies at participating hospitals should be included regardless of the mother’s residency.
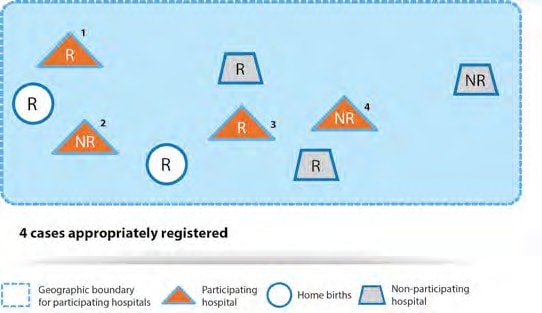
No, they are not included; only births that occur in participating hospitals should be included.