Congenital Anomalies of the Nervous System: Microcephaly
Microcephaly is a cranial vault that is smaller than normal for the baby’s sex and gestational age at birth (Fig. 11). The size of the cranial vault is an indicator of the size of the underlying brain.
Fig. 11. Newborn with a normal head size, microcephaly, and severe microcephaly
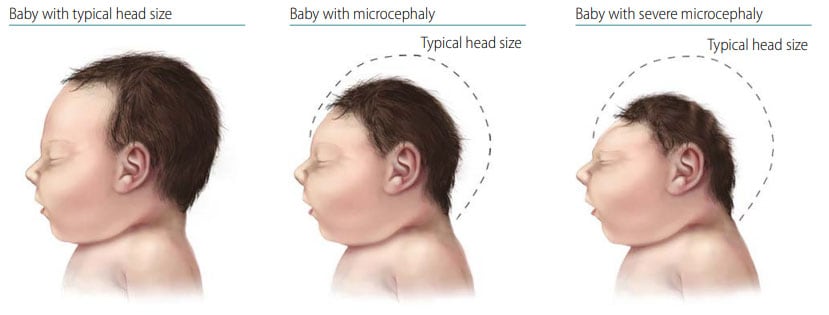
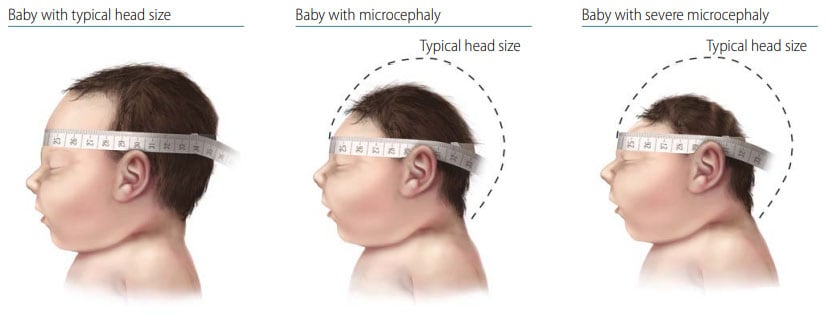
Fig. 12. Measurement of head size
Diagnosis
Prenatal. Transabdominal ultrasound between 18 and 37 weeks’ gestation might identify a small head size and with serial ultrasounds, showing poor growth over time.
Postnatal. At delivery, a measurement of the occipito-frontal circumference (OFC) or head circumference (HC) that is three standard deviations (SD) below the mean for the age- and sex appropriate distribution curves is diagnostic of severe microcephaly. Report if using a different definition or cut-off point to define microcephaly (e.g. two SD below the mean). Detailed imaging and expert consultations (e.g. paediatric geneticist, paediatric neurologist) can confirm the diagnosis of an underlying brain abnormality and might help identify the underlying cause of microcephaly.
Clinical and epidemiologic notes
- Use a tape measure that cannot be stretched.
- Place the tape around the widest part of the head, above the eyebrows and ears, on the forehead and most prominent part of the occiput. See Fig. 12.
- Record the measurement to the nearest 0.1 cm.
- Ideally, the measurement should be taken three times (use largest).
- Although head moulding and/or swelling can occur during the birthing process, HC measurements should be obtained within the first 24 hours of life. Standards for HC were developed on early measurements (i.e. INTERGROWTH-21st measurements were obtained before 12 hours of life and WHO measurements were obtained before 24 hours of life). Therefore, postponing HC measurements until after 24 hours of life to allow for birth process changes to subside results in not having appropriate comparison standards.
The INTERGROWTH-21st online tool (http://intergrowth21.ndog.ox.ac.ukexternal icon) can be used to enter data to calculate the percentile of the HC or compare to standards based on the infant’s sex and prematurity.
- Many genetic syndromes are associated with microcephaly: Autosomal recessive microcephaly; trisomy 18; inborn errors of metabolism; Rett syndrome, etc.
- Teratogenic conditions with microcephaly include congenital rubella, CMV, congenital Zika infection and congenital toxoplasmosis.
- Always calculate the percentile of HC considering sex and gestational age.
- There is no single definition of microcephaly that is universally used. Report which charts (e.g. INTERGROWTH-21st) and cut-off points you are using to define microcephaly.
- Microcephaly can occasionally be a normal trait in a family (though less likely if severe or symptomatic); therefore, measuring parents’ OFC if possible is reasonable.
- Obtain a thorough pregnancy history, looking in particular for infections and other exposures.
Depending on capacity and clinical findings, consider imaging to document intracranial anatomy and selected laboratories (genetic studies, viral studies, etc.).
Checklist for high-quality reporting
| Microcephaly – Documentation Checklist |
Describe in detail:
Take and report photographs: Show full face and body photographs, if allowed; can be crucial for review Describe evaluations to find or rule out related and associated anomalies:
Report whether autopsy (pathology) findings are available and if so, report the results. |