TB NOTES

TB Notes 3, 2020
Notes from the Director

Dear Colleague,
The COVID-19 pandemic continues to impact public health services, including tuberculosis (TB) control services, as described in a publication in CDC’s Morbidity and Mortality Weekly Report. The Division of TB Elimination (DTBE) staff continue to deploy to CDC’s response to the COVID-19 pandemic. Also, we are aware of the shifting staff roles and responsibilities as well as resources in public health departments and healthcare facilities across the United States to address the ongoing needs of the COVID-19 response.
As of October 30, 102 DTBE staff members (64% of DTBE staff) have participated in 196 deployments supporting CDC’s COVID-19 response efforts. Over 600 staff from the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention have been deployed to work on COVID-19 response activities. DTBE’s embedded field-based staff have also participated in the response efforts of their assigned local jurisdictions. Thank you to everyone who has responded to the COVID-19 pandemic.
Even with the challenges we face due to COVID-19, this issue of TB Notes demonstrates that the critical work towards achieving TB elimination continues.
Recently, results from two important studies were presented at the 51st Union World Conference:
- CDC’s Tuberculosis Trials Consortium (TBTC) and the National Institute of Health’s Adult AIDS Clinical Trials Group (ACTG) announced findings from Study 31/A5349. Study 31/A5349 is the first clinical trial to identify a shorter 4-month daily treatment regimen for drug-susceptible TB disease that is as effective as (non-inferior to) the existing 6-month daily regimen in curing TB disease. This is the first new treatment regimen for drug-susceptible TB disease in almost 40 years. I am grateful to the researchers, clinical staff, and most of all, study participants, for their important contributions to this study.
- A two-year study conducted by New York City Department of Health and Mental Hygiene, CDC, and Columbia University, showed that electronic directly observed therapy (eDOT) was at least as effective as traditional in-person DOT for ensuring high adherence to treatment while enabling patient-centered care for TB disease.
CDC also released the 2019 edition of Reported Tuberculosis in the United States. Once again, the United States reported the lowest number of TB cases (8,916) and the lowest incidence rate on record (2.7 cases per 100,000 persons). The United States has achieved substantial progress in reducing TB; however, the rate of decrease remains low. This report compiles TB surveillance data collected for U.S. TB cases counted in 2019, before the COVID-19 pandemic directly affected the United States. Effects of reduced public health capacity for TB prevention and control will become clearer after provisional surveillance data, including number of U.S. TB cases reported during 2020, are published in early 2021. DTBE will continue to work closely with state and local TB control programs, as well as our partners at the National TB Controllers Association to monitor and document the effect of COVID-19 on 2020 TB reporting activities.
This is the second year the report is published exclusively online, as part of CDC’s Digital First Initiative to help audiences discover, view, and share content more easily. I want to especially thank all the state and local health departments throughout the United States whose staff collected and reported the data used in this publication.
Finally, CDC continues to monitor issues related to nitrosamine impurities identified in rifampin and rifapentine. On August 26, U.S. Food and Drug Administration (FDA) issued a statement related to mitigating shortages of rifampin and rifapentine and its interim guidance to continue using these drugs in the treatment of TB after nitrosamine-class impurities were detected through recently adopted regulatory standards to assay all medications for nitrosamines. Read CDC’s Dear Colleague Letter to learn more about what this means for the prevention of TB disease and treatment of latent TB infection. CDC will work with our partners at FDA, the National Tuberculosis Controllers Association (NTCA), state and local health departments, and the TB Centers of Excellence for Training, Education, and Medical Consultation to ensure TB patients continue to receive safe and effective treatment.
Thank you for your continued dedication to TB prevention and control.
Philip LoBue, MD, FACP, FCCP
Director
Division of Tuberculosis Elimination
National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention
Electronic Directly Observed Therapy (eDOT) is as Effective as Traditional DOT for the Treatment of TB Disease
Directly observed therapy (DOT) is the most effective strategy for ensuring that TB patients adhere to treatment. DOT means that a health care worker or other designated person watches the TB patient swallow each dose of the prescribed drugs. However, because in-person DOT can be time- and resource-intensive for patients and DOT workers, some TB programs have elected to use alternative DOT methods for treatment of TB disease. Electronic DOT (eDOT) is one alternative to in-person DOT where a patient is remotely observed (e.g., over a smartphone) taking their TB medication.
In a two and a half-year study conducted by New York City Department of Health and Mental Hygiene Bureau of Tuberculosis Control, CDC, and Columbia University, data showed that electronic directly observed therapy (eDOT) was at least as effective as traditional in-person DOT for ensuring high adherence to treatment while enabling patient-centered care for TB disease. Supported by CDC’s DTBE, with funding from the Antibiotic Resistance Solutions Initiative, the randomized two-period cross-over non-inferiority trial was conducted in the Morrisania, Fort Green, Washington Heights, and Corona TB Chest Clinics.
The study observed patients from July 2017 through January 2020. Additional analyses reveal the types and severity of adverse events were similar between both DOT methods. Also, after undergoing eDOT and in-person DOT, more study participants reported overall satisfaction with electronic DOT that with in-person DOT.
Results from this study were presented at the 51st Union Conference on Lung Health on October 23, 2020. CDC will use the results of this study in considering whether new guidelines or recommendations are needed. CDC previously published Implementing an Electronic Directly Observed Therapy (eDOT) Program: A Toolkit for Tuberculosis (TB) Programs to assist TB programs in developing and implementing a TB eDOT program.
This work was a collaboration of colleagues in the Division’s Data Management, Statistics and Evaluation Branch, the Clinical Research Branch, the Field Services Branch and the DTBE Office of the Director; as well as expert consultation provided by colleagues at the University of California San Francisco and University of California San Diego.
The Latent Tuberculosis Infection: A Guide for Primary Health Care Providers Gets a New Look!
In July, DTBE announced the release of the updated Latent Tuberculosis Infection: A Guide for Primary Health Care Providers. The guide is intended for primary care providers who care for individuals and populations who may be at risk for infection with M. tuberculosis. The content includes latent TB infection diagnosis and treatment information, sample documentation forms, and additional resources.
The product is currently available online and can be downloaded from the CDC DTBE website. Free print copies are available for order from CDC-Info On Demand – Publications. For information on how to order print copies of the guide, please see the publication ordering instructions.
Submitted by Nick DeLuca, PhD, CEBSB Branch Chief
Reported Tuberculosis in the United States, 2019 Now Available
Earlier this year, on March 19, 2020 CDC released provisional 2019 surveillance data on reported TB cases in the United States. The full report, Reported Tuberculosis in the United States, is now available online.
This report compiles TB surveillance data collected for U.S. TB cases counted in 2019, before the COVID-19 pandemic directly affected the United States. The COVID-19 pandemic has strained public health services, including TB control services, across sectors of public health. We will continue to work closely with state and local TB control programs, as well as our partners at the National TB Controllers Association to monitor and document the effect of COVID-19 on 2020 TB reporting activities.
Key findings:
- In 2019, 8,916 TB cases were reported in the United States, a 1.2% decrease from 2018.
- TB cases were not evenly distributed across the U.S.
- Four jurisdictions account for over half (51%) of all reported U.S. TB cases: California, Florida, New York City, and Texas.
- The national TB incidence rate decreased to 7 cases per 100,000 persons.
- Nine states and the District of Columbia reported TB rates above the national average.
- Among U.S.-born people, TB disease disproportionately occurs among non-White persons.
- Nationally, only one in eight (12.5%)S. TB cases with available genotype data are considered the result of TB transmission that occurred in the local area in the preceding 2 years (i.e., recent transmission).
- A disproportionate number of U.S. TB cases occur among people born outside of the United States, largely because of progression of longstanding latent TB infection likely acquired before arriving in the United States.
- TB cases were not evenly distributed across the U.S.
CDC has created a slide set, fact sheet, and social media graphics with highlights from the surveillance report to support TB education and outreach to clinicians, health care agencies, and community organizations.
The United States continues to have one of the lowest TB case rates in the world, and the 2019 case count represents the lowest number of TB cases on record. Still, too many people suffer from TB disease and our progress is too slow to eliminate TB in this century. Ending TB will require a dual approach of maintaining and strengthening current TB control priorities, while increasing efforts to identify and treat latent TB infection in populations at risk for TB disease.
Read more in a recent Dear Colleague Letter.
Julie Self, PhD, MPH Selected as Surveillance Team Lead

In August, DTBE announced the selection of Julie Self, PhD, MPH as the Surveillance, Epidemiology, and Outbreak Investigations Branch (SEOIB) Surveillance Team Lead. Dr. Self joined DTBE in 2017 as an epidemiologist with the SEOIB Molecular Epidemiology Activity. As part of the SEOIB Molecular Epidemiology Activity, she supported state and local TB programs to apply molecular data to enhance the epidemiologic understanding of TB, assisted with enhancements to the TB genotyping database, and conducted analyses to improve understanding of TB among people experiencing homelessness. She coauthored the molecular epidemiology sections for the 2017, 2018, and 2019 annual TB surveillance reports. She has been the lead CDC investigator on an important collaboration with academic partners to estimate the serial interval and reproductive number of TB. Most recently, Dr. Self has served in a 120-day detail position as the acting Surveillance Team Lead, during which she has led substantial progress on the team’s key priorities despite challenges due to the COVID-19 pandemic.
Before joining DTBE, Dr. Self served as an Epidemic Intelligence Service (EIS) Officer assigned to the Enteric Diseases Epidemiology Branch in CDC’s National Center for Emerging and Zoonotic Infectious Diseases. Prior to joining CDC as an EIS officer, she earned her MPH and PhD at Emory University. Outside of work, she enjoys spending time outside with her family, including her husband and three daughters.
Submitted by Adam Langer, DVM, MPH, DACVPM, SEOIB Branch Chief
Available Now: Training Video on the Methods for Performing Whole-Genome Single Nucleotide Polymorphism (SNP) Comparison
DTBE published a training video called “A look at the methods behind whole-genome single nucleotide polymorphism (SNP) comparison and phylogenetic analysis for TB.” The purpose of the video is to provide state and local TB control program staff with information on the methods for performing whole-genome single nucleotide polymorphism (SNP) comparison.
Whole-genome SNP comparison is a laboratory-based approach used to analyze the genetic material (e.g. DNA) of Mycobacterium tuberculosis, the bacterium that causes TB disease. This training video explains how to interpret the analysis results of the SNP comparison to help state and local TB control program staff better understand the TB cases in their specific area. For example, the phylogenetic trees created during SNP comparison can help state and local TB control program staff know if the TB cases in a specific area are due to new cases of TB or are latent TB infection that has recently developed into TB disease.
The learning objectives of “A look at the methods behind whole-genome single nucleotide polymorphism (SNP) comparison and phylogenetic analysis for TB” are to describe:
- The analytic steps involved in whole-genome SNP comparison;
- How a phylogenetic tree is built using the results of whole-genome SNP comparison;
- How the placement of the most recent common ancestor (MRCA) is determined; and
- How adding or removing isolates from the comparison can affect results.
Submitted by Sarah Talarico, PhD, Senior Epidemiologist
The COVID-19 Response and its effect on TB Prevention and Control Efforts from March to April 2020
After the first U.S. case of coronavirus disease 2019 (COVID-19) was reported on January 20, 2020, personnel from state, local, and territorial TB programs were deployed for their jurisdictions’ COVID-19 response. TB control professionals possess critical skills and expertise needed for the COVID-19 response, including contact tracing, infection control, and clinical care and treatment.
From March to April 2020, CDC and the National TB Controllers Association (NTCA) communicated with state, local, and territorial TB programs to understand the effect of COVID-19 deployments on essential TB activities. The discussions revealed that most TB programs experienced partial or high impact on staff capacity and essential TB control services, suggesting that the response to COVID-19 is diverting resources from essential TB elimination activities.
The COVID-19 pandemic has strained public health services, including TB control services, across sectors of public health. Impacted public health programs will need to develop strategies to resume and catch-up on services. Averting a resurgence of TB in the United States requires sustaining essential TB program activities while addressing the COVID-19 pandemic. CDC and NTCA are committed to supporting TB programs through technical assistance and providing opportunities and forums for programs to share innovative strategies and best practices.
Read more in the CDC MMWR publication, Notes from the Field: Effects of the COVID-19 Response on Tuberculosis Prevention and Control Efforts — United States, March–April 2020.
Submitted by Ann Cronin, BA, Associate Director for Policy and Issues Management
Congratulations to FSB’s 68th Annual CDC and ATSDR Honor Award Recipients!
The CDC and ATSDR Honor awards highlights notable and significant achievements over the past calendar year, with some selected awards, presented by the CDC Foundation, given in recognition of career contributions while at the agency. Each year, CDC and ATSDR recognize This year’s honor award ceremony was held virtually due to the COVID-19 pandemic. Encompassing categories across scientific, program, management and operations sectors, the awards, which began in 1952, seeks to honor honored employee for improving agency performance and helping ensure our efforts are not only effective, but also as far-reaching as possible.
Excellence in Program Delivery− International
Congratulations to Dr. Richard Brostrom and the TB Free Majuro team for receiving the 68th Annual CDC & ATSDR Honor Award for This award was presented to TB Free Majuro for their excellence in program delivery for the screening of more than 23,000 people for latent TB infection and treatment of more than 5,000 people for latent TB infection. TB Free Majuro sought to achieve mass TB prevention in the Marshall Islands. The 5-month project was funded primarily by the U.S. Department of Interior. The National TB Controllers Association helped to coordinate more than 100 volunteer doctors and nurses from 21 states to implement the project. The local Marshallese workforce played significant role in delivering the more 50,000 doses one at a time for safe and effective TB prevention.
Watch Dr. Brostrom’s acceptance speech to learn more about the project.
Excellence in Leadership Award
Congratulations to Jolisa Parham for receiving the Excellence in Leadership Award! Jolisa received this award for demonstrating exceptional leadership and being a role model for other junior public health advisors while serving CDC with distinction.
Watch Jolisa’s acceptance speech here.
CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention also presented awards to Outstanding Field Staff. DTBE was well-represented, with winners in the following categories:
Outstanding Field Supervisor
Farah Parvez
New York City Bureau of TB Control
Division of Tuberculosis Elimination
Outstanding Field Investigator/Outbreak Response
Jolisa Parham
Fulton County, Georgia Tuberculosis Program
Division of Tuberculosis Elimination
Outstanding Field Program Management
Stuart McMullen
Los Angeles Tuberculosis Control Program
Division of Tuberculosis Elimination
Submitted by Terry Chorba, MD, MPH, MPA, FBS Branch Chief
Updated ARPE Data Submission Forms to Monitor Contact Follow-up and Targeted Testing Activities
The Aggregate Report for Program Evaluation (ARPE) is an online data reporting system where TB programs in the United States submit information about their contact follow-up activities. Based on recommendations from the Advisory Council for the Elimination of TB (ACET), the ARPE contact investigation form has been updated to include optional fields on contacts’ origin of birth, type of test (IGRA or TST) administered, and among those with latent tuberculosis infection (LBTI), treatment regimen at the start and end of treatment. This additional information will allow for more detail about the characteristics, testing, and treatment of contacts which can help inform program planning and policy development.
These fields are included in the National Tuberculosis Indicators Project (NTIP) online ARPE contact investigation form and a hard copy is available online.
TB programs in areas with >150 TB cases per year are now required to submit information about their targeted testing activities (Tuberculosis Elimination and Laboratory Cooperative Agreement CDC-RFA-PS20-2001). To assist with this reporting requirement, a Targeted Testing and Treatment for Latent Tuberculosis Infection Form has been added to NTIP under the ARPE tab and a hard copy is available online. Although targeted testing data submission is only required for jurisdictions with a high TB incidence (≥150 cases per year), all jurisdictions are encouraged to complete this form. As with the ARPE Contact Investigation (CI) form, the Targeted Testing (TT) form includes optional fields to provide information about the characteristics of contacts (origin of birth), type of test (IGRA and TST), and the treatment regimen at the start and end of LTBI treatment.
Instructions on completing these forms and additional information have been added to the NTIP Online Help Webpage. Additionally, NTIP has been revised to include reports on the new optional fields and targeted testing results. With this information, TB programs can review their program’s performance on contact investigation and targeted testing activities. Each jurisdiction’s project officer and program evaluation consultant can provide more information on the revised ARPE CI and TT forms.
Submitted by David Wilson, M.Ed., DMSEB Deputy Branch Chief
National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention’s TB Epidemiologic and Economic Modeling Agreement 2020 update
In fiscal year 2020, researchers in the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Epidemiologic and Economic Modeling Agreement (NEEMA) had eight journal articles published, an additional three articles awaiting final decisions by editors, and two more drafted to be submitted for publication soon. This productivity is the culmination of five years of TB NEEMA, which resulted in 11 journal and two TB Notes publications prior to fiscal year 2020, listed at https://www.cdc.gov/nchhstp/neema/published-papers/tb.html.
The following are the 2020 publication citations:
Jo Y, Shrestha S, Gomes I, Marks S, Hill A, Asay G, and Dowdy D. Model-Based Cost-Effectiveness of State-level Latent Tuberculosis Interventions in California, Florida, New York and Texas. Clin Infect Dis. 2020 Jun 25;ciaa857. doi:10.1093/cid/ciaa857.
Marks SM, Dowdy DW, Menzies NA, Shete PB, Salomon JA, Parriott A, Shrestha S, Flood J, Hill AN. Policy implications of mathematical modeling of latent tuberculosis infection testing and treatment strategies to accelerate tuberculosis elimination. Public Health Rep 2020;135(1 Suppl):38S–43S. doi:10.1177/0033354920912710
Menzies NA, Bellerose M, Testa C, Swartwood N, Malyuta Y, Cohen T, Marks SA, Hill AN, Date AA, Maloney SA, Bowden SE, Grills AW, Salomon JA. Impact of Effective Global Tuberculosis Control on Health and Economic Outcomes in the United States. Am J Respir Crit Care Med. 2020 Jul 9; doi:10.1164/rccm.202003-0526OC
Menzies NA, Parriott A, Shrestha S, Dowdy DW, Cohen T, Salomon JA, Marks SM, Hill AN, Winston CA, Asay GB, Barry PM, Readhead A, Flood J, Kahn JG, Shete PB. Comparative modelling of TB epidemiology and policy outcomes in California. Am J Respir Crit Care Med. 2020 Feb 1; 201(3):356-365. doi: 10.1164/rccm.201907-1289OC.
Menzies NA, Swartwood N, Testa C, Malyuta Y, Hill AN, Marks SM, Cohen T, Salomon, JA. Time since infection and risks of future disease for individuals with Mycobacterium tuberculosis infection in the United States. Epidemiol. 2020. doi:10.1097/ede.0000000000001271
Miller AP, Malekinejad M, Horváth H, Blodgett JC, Kahn JG, Marks SM. Healthcare facility-based strategies to improve tuberculosis testing and linkage to care in non-U.S.-born populations in the United States: A systematic review. PLoS One. 2019; 14(9):e0223077. doi: 10.1371/journal.pone.0223077.
Parriott A, Kahn JG, Ashki H, Readhead A, Barry PM, Goodell AJ, Flood J, Shete PB. Modeling the Impact of Recommendations for Primary Care-Based Screening for Latent Tuberculosis Infection in California. Public Health Rep. 2020; 135(1_suppl), 172s-181s. doi:10.1177/0033354920927845
Shrestha S, Parriott A, Menzies N, Shete P, Hill A, Marks SM, Dowdy D. Estimated population-level impact of using a six-week regimen of daily rifapentine to treat latent tuberculosis infection in the United States. Ann Am Thorac Soc. 2020 Sep 11. doi: 10.1513/AnnalsATS.202005-574RL.
Reported by Suzanne Marks, MPH, MA, Epidemiologist, Health Economist
In early 2015, the Laboratory Branch’s (LB) began its journey to obtain ISO 17025 accreditation (general requirements for the competence of testing and calibration laboratories) as part of a pilot through the Office of Laboratory Science and Safety (OLSS) at CDC. Accreditation was obtained in May of 2018. As part of the accreditation process, the laboratory must undergo a follow up assessment which was completed on July 9th, 2020. Angela Starks, Beverly Metchock, Lois Diem, Melinda Dunn, Atanaska Marinova-Petkova, and Calin Chiribau participated in the on-site assessment. The American Association for Laboratory Accreditation (A2LA) assessor evaluated the branch’s quality management system and technical documentation including purchasing, customer satisfaction, communication, equipment maintenance, environmental controls, sample accessioning, technical procedures, quality control, test reporting, training and competency. The assessor found no deficiencies whatsoever with LB’s QMS or test under scope. The assessor gave high praise to the laboratory staff. Maintaining accreditation would not have been possible without the support and dedication of the laboratory staff.
Submitted by Lois Diem, BS, Biologist
Landmark TB Trial Identified Shorter-Course Treatment Regimen
On October 21, 2020 during the virtual 51st Union World Conference on Lung Health, the Tuberculosis Trials Consortium (TBTC) from the U.S. Centers for Disease Control and Prevention (CDC), along with collaborators from the National Institute of Health’s AIDS Clinical Trial Group (ACTG), announced the results of Study 31/A5349. Study 31/A5349 – an international, randomized, controlled, open label, phase 3 non-inferiority clinical trial – examined the efficacy and safety of two four-month regimens with high-dose rifapentine with or without moxifloxacin for the treatment of drug-susceptible TB disease. The results from this study identified a shorter four-month daily treatment regimen with high-dose, or “optimized,” rifapentine and moxifloxacin that is as effective as (non-inferior to) the standard daily six-month regimen in curing drug-susceptible TB disease. This is the first successful short treatment regimen for drug-susceptible TB disease identified in almost 40 years.
Reducing the length of time for treating TB has been a longstanding public health goal. Shortening treatment for TB disease can benefit patients, families, healthcare providers and health systems. The availability of shorter regimens enables patients to be cured faster, and has the potential to reduce treatment costs, improve patient quality of life, and increase completion of therapy.
These results can help inform future TB disease treatment. CDC will continue to work with TB control programs and clinicians to improve available treatment regimens for TB disease.
Find more information about Study 31/A5349 in a recent Dear Colleague Letter.
Submitted by Andrew Vernon, MD, MHS, CRB Branch Chief
Launch of the TB Community Engagement Network
CDC has partnered with the Asian Pacific Islander American Health Forum (APIAHF), Association of Asian Pacific Community Health Organizations (AAPCHO), Hepatitis B Foundation (HBF), and Stop TB USA to lead the TB Community Engagement Network (CEN), a new initiative to work more closely with state and local TB control programs, as well as community-based organizations and community health centers.
The goals of the TB CEN are to:
- Conduct outreach to underserved Asian Americans and Native Hawaiian and Pacific Islander communities at risk for TB
- Increase awareness and understanding of culturally and linguistically appropriate latent TB infection and TB disease testing and treatment strategies
- Share resources and best practices among providers
- Develop partnerships to scale existing initiatives
The TB CEN held its first meeting on July 29, 2020. Fourteen organizations across the United States have joined the CEN. We look forward to the great work of the TB CEN to help increase testing, diagnosis and treatment of latent TB infection and TB disease to end TB in the United States!
Learn more information about the TB CEN here or contact tb-cen@aapcho.org.
We Are TB: Creating a support network for patients being treated for TB disease and latent TB infection
We are TB is a volunteer organization that provides support to current TB patients during diagnosis and treatment of TB disease and latent TB infection, advocates for funding of TB programs, and raises awareness about TB through education and outreach. Founded in 2015, the organization has grown and now includes roughly 50 active volunteer members.
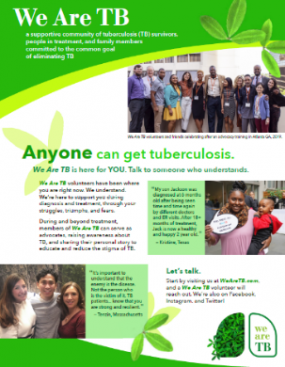
Members provide patient support by connecting with individuals who were recently diagnosed with TB disease or latent TB infection and have a similar TB story. Through a shared experience, the members can provide emotional support and guidance through the treatment process. We Are TB creates a community for people who have been diagnosed with TB. Support is currently available in English and the organization is looking to expand to other languages soon.
We Are TB raises awareness around TB through education and outreach efforts. Many We Are TB volunteers have shared their personal story of being treated for TB disease or latent TB infection, as well as the work of TB control professionals, through CDC’s Personal Stories. These stories help to put a ‘face’ with TB to provide education and reduce stigma around TB.
We Are TB volunteers also meet with U.S. government representatives to raise awareness of TB in the U.S. and to advocate for funding of TB programs. Members participate on U.S. and international panels and advisory committees to advocate for people who have been diagnosed with TB.
A new brochure, created in collaboration with the California Tuberculosis Controllers Association, highlights We Are TB to raise awareness about the organization and to provide information on its activities. TB programs are encouraged to print the brochure to share with patients who are diagnosed with TB disease or latent TB infection who may like to connect with others with a shared experience.
We Are TB is a subset of the National Tuberculosis Controllers Association. Learn more about We Are TB on their website or follow them on Twitter, Facebook, & Instagram for the latest updates of activities.
Submitted by Kate O’Brien, We Are TB Speaker Coordinator
Skills-based Contact Tracing Training Now Available!
Successful case investigation and contact tracing for COVID-19 depends on a robust and well-trained public health workforce. CDC is partnering with the National Network of Disease Intervention Training Centers (NNDITC) to offer virtual skills-based trainings for contact tracers and case investigators. The “National COVID-19 Virtual Skills-Based Training Program” will train staff to support public health systems throughout the United States as they mobilize to address COVID-19. State and local health departments are encouraged to offer these trainings to staff that will be conducting COVID-19 case investigation or contact tracing activities in their jurisdictions.
These contact tracing and case investigation training sessions began at the end of August. Four Regional Training Centers will support two training courses per week to accommodate demand. Registration is open to all jurisdictions at the following link: https://www.nnditc.org/index.html. All participants must first complete either the ASTHO or Johns Hopkins online knowledge-based course prior to being approved for these courses. Participants should register for the training conducted by the regional Disease Intervention Training Center for their respective state. This fact sheet provides additional information on the knowledge- and skill-based courses and provides links for registration.
These training have also benefited from the expertise of the TB Centers of Excellence for Training, Education, and Medical Consultation (TB COEs). The TB COEs contributed their knowledge and skills to the development of the training curriculum as well as the implementation of the trainings.
If you have questions about registering or need assistance, please contact info@nnditc.org for guidance.
COVID-19 Contact Tracing Resources
Check out CDC’s COVID-19 Contact Tracing resources! These resources for health departments include social media graphics, translations of the contact tracing fact sheet and infographic, and contact tracing implementation tools.
Contact Tracing Communications Toolkit for Health Departments
- The toolkit, also available in Spanish, features talking points, sample public service announcements, graphics, social media posts, questions and answers, and more.
- Resources include:

Contact Tracing Resources for Health Departments
- On this page, you can find a compilation of contact tracing resources, including CDC guidance documents and contact tracing implementation guides and tools.
Customizable versions of the Contact Tracing Steps Infographic are also available on the STLT Collaboration Space’s Communication Resource Center (CRC).
Submitted by Allison Maiuri, MPH, Education, Training, and Behavioral Studies Team Lead
DTBE-authored COVID-19 Publications
Chow EJ, Schwartz NG, Tobolowsky FA, Zacks RLT, Huntington-Frazier M, Reddy SC, Rao AK. Symptom Screening at Illness Onset of Health Care Personnel With SARS-CoV-2 Infection in King County, Washington. JAMA. 2020 May 26;323(20):2087-2089. doi: 10.1001/jama.2020.6637.
Dawood FS, Ricks P, Njie GJ, Daugherty M, Davis W, Fuller JA, Winstead A, McCarron M, Scott LC, Chen D, Blain AE, Moolenaar R, Li C, Popoola A, Jones C, Anantharam P, Olson N, Marston BJ, Bennett SD. Observations of the global epidemiology of COVID-19 from the prepandemic period using web-based surveillance: a cross-sectional analysis. Lancet Infect Dis. 2020 Jul29;S1473-3099(20)30581-8.doi:10.1016/S1473-3099(20)30581-8. Epub ahead of print.
Dawson P, Rabold EM, Laws RL, Conners EE, Gharpure R, Yin S, Buono SA, Dasu T, Bhattacharyya S, Westergaard RP, Pray IW, Ye D, Nabity SA, Tate JE, Kirking HL. Loss of Taste and Smell as Distinguishing Symptoms of Coronavirus Disease 2019. Clin Infect Dis. 2020 Jun 21: ciaa799. doi: 10.1093/cid/ciaa799. Epub ahead of print.
Feng Z, Glasser JW, Hill AN. On the benefits of flattening the curve: A perspective. Math Biosci. 2020 Aug;326:108389. doi: 10.1016/j.mbs.2020.108389. Epub ahead of print.
Godfred-Cato S, Bryant B, Leung J, Oster ME, Conklin L, Abrams J, Roguski K, Wallace B, Prezzato E, Koumans EH, Lee EH, Geevarughese A, Lash MK, Reilly KH, Pulver WP, Thomas D, Feder KA, Hsu KK, Plipat N, Richardson G, Reid H, Lim S, Schmitz A, Pierce T, Hrapcak S, Datta D, Bamrah Morris S, Clarke K, Belay E, California MIS-C Response Team. COVID-19–associated multisystem inflammatory syndrome in children—United States, March–July 2020. MMWR Morb Mortal Wkly Rep 2020;69:1074–80. doi: 10.15585/mmwr.mm6932e2
Gold JAW, Wong KK, Szablewski CM, Patel PR, Rossow J, da Silva J, Natarajan P, Morris SB, Fanfair RN, Rogers-Brown J, Bruce BB, Browning SD, Hernandez-Romieu AC, Furukawa NW, Kang M, Evans ME, Oosmanally N, Tobin-D’Angelo M, Drenzek C, Murphy DJ, Hollberg J, Blum JM, Jansen R, Wright DW, Sewell WM 3rd, Owens JD, Lefkove B, Brown FW, Burton DC, Uyeki TM, Bialek SR, Jackson BR.
Characteristics and Clinical Outcomes of Adult Patients Hospitalized with COVID-19 – Georgia, March 2020. MMWR Morb Mortal Wkly Rep. 2020 May 8;69(18):545-550. doi: 10.15585/mmwr.mm6918e1.
Hatcher SM, Agnew-Brune C, Anderson M, Zambrano LD, Rose CE, Jim MA, Baugher A, Liu GS, Patel SV, Evans ME, Pindyck T, Dubray CL, Rainey JJ, Chen J, Sadowski C, Winglee K, Penman-Aguilar A, Dixit A, Claw E, Parshall C, Provost E, Ayala A, Gonzalez G, Ritchey J, Davis J, Warren-Mears V, Joshi S, Weiser T, Echo-Hawk A, Dominguez A, Poel A, Duke C, Ransby I, Apostolou A, McCollum J. COVID-19 Among American Indian and Alaska Native Persons — 23 States, January 31–July 3, 2020 MMWR Morb Mortal Wkly Rep. 2020 Aug 28; 69(34): 1166–1169. doi: 10.15585/mmwr.mm6934e1.
Lasry A, Kidder D, Hast M, Poovey J, Sunshine G, Winglee K, Zviedrite N, Ahmed F, Ethier KA; CDC Public Health Law Program; New York City Department of Health and Mental Hygiene; Louisiana Department of Health; Public Health – Seattle & King County; San Francisco COVID-19 Response Team; Alameda County Public Health Department; San Mateo County Health Department; Marin County Division of Public Health. Timing of Community Mitigation and Changes in Reported COVID-19 and Community Mobility – Four U.S. Metropolitan Areas, February 26-April 1, 2020. MMWR Morb Mortal Wkly Rep. 2020 Apr 17;69(15):451-457. doi: 0.15585/mmwr.mm6915e2.
McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, Lewis J, Baer A, Kawakami V, Lukoff MD, Ferro J, Brostrom-Smith C, Rea TD, Sayre MR, Riedo FX, Russell D, Hiatt B, Montgomery P, Rao AK, Chow EJ, Tobolowsky F, Hughes MJ, Bardossy AC, Oakley LP, Jacobs JR, Stone ND, Reddy SC, Jernigan JA, Honein MA, Clark TA, Duchin JS; Public Health–Seattle and King County, EvergreenHealth, and CDC COVID-19 Investigation Team. Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. N Engl J Med. 2020 May 21;382(21):2005-2011. doi: 10.1056/NEJMoa2005412. Epub 2020 Mar 27.
Moore JT, Ricaldi JN, Rose CE, Fuld J, Parise M, Kang GJ, Driscoll AK, Norris T, Wilson N, Rainisch G, Valverde E, Beresovsky V, Brune CA, Oussayef NL, Rose DA, Adams LE, Awel S, Villanueva J, Meaney-Delman D, Honein MA, COVID-19 State, Tribal, Local, and Territorial Response Team. Disparities in Incidence of COVID-19 Among Underrepresented Racial/Ethnic Groups in Counties Identified as Hotspots During June 5–18, 2020 — 22 States, February–June 2020. MMWR Morb Mortal Wkly Rep. 2020 Aug 21; 69(33): 1122–1126. doi: 10.15585/mmwr.mm6933e1.
Mosites E, Parker EM, Clarke KEN, Gaeta JM, Baggett TP, Imbert E, Sankaran M, Scarborough A, Huster K, Hanson M, Gonzales E, Rauch J, Page L, McMichael TM, Keating R, Marx GE, Andrews T, Schmit K, Bamrah Morris S, Dowling NF, Peacock G; COVID-19 Homelessness Team. Assessment of SARS-CoV-2 Infection Prevalence in Homeless Shelters – Four U.S. Cities, March 27-April 15, 2020. MMWR Morb Mortal Wkly Rep. 2020 May 1;69(17):521-522. doi: 10.15585/mmwr.mm6917e1. 2020.
Njuguna H, Wallace M, Simonson S, Tobolowsky FA, James AE, Bordelon K, Fukunaga R, Gold JAW, Wortham J, Sokol T, Haydel D, Tran H, Kim K, Fisher KA, Marlow M, Tate JE, Doshi RH, Curran KG. Serial Laboratory Testing for SARS-CoV-2 Infection Among Incarcerated and Detained Persons in a Correctional and Detention Facility — Louisiana, April–May 2020. MMWR Morb Mortal Wkly Rep. 2020 Jul 3;69(26):836-840. doi: 10.15585/mmwr.mm6926e2.
Stokes EK, Zambrano LD, Anderson KN, Marder EP, Raz KM, El Burai Felix S, Tie Y, Fullerton KE. Coronavirus Disease 2019 Case Surveillance – United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020 Jun 19;69(24):759-765. doi: 10.15585/mmwr.mm6924e2.
Szablewski CM, Chang KT, Brown MM, Chu VT, Yousaf AR, Anyalechi N, Aryee PA, Kirking HL, Lumsden M, Mayweather E, McDaniel CJ, Montierth R, Mohammed A, Schwartz NG, Shah JA, Tate JE, Dirlikov E, Drenzek C, Lanzieri TM, Stewart RJ. SARS-CoV-2 transmission and infection among attendees of an overnight camp—Georgia, June 2020. MMWR Morb Mortal Wkly Rep 2020 Aug 7;69:1023–5. doi:10.15585/mmwr.mm6931e1
Tobolowsky FA, Gonzales E, Self JL, Rao CY, Keating R, Marx GE, McMichael TM, Lukoff MD, Duchin JS, Huster K, Rauch J, McLendon H, Hanson M, Nichols D; Pogosjans S, Fagalde M, Lenahan J, Maier E, Whitney H, Sugg N, Chu H, Rogers J, Mosites E, Kay M. COVID-19 Outbreak Among Three Affiliated Homeless Service Sites – King County, Washington, 2020. MMWR Morb Mortal Wkly Rep. 2020 May 1;69(17):523-526. doi: 10.15585/mmwr.mm6917e2.
Waltenburg MA, Victoroff T, Rose CE, Butterfield M, Jervis RH, Fedak KM, Gabel JA, Feldpausch A, Dunne EM, Austin C, Ahmed FS, Tubach S, Rhea C, Krueger A, Crum DA, Vostok J, Moore MJ, Turabelidze G, Stover D, Donahue M, Edge K, Gutierrez B, Kline KE, Martz N, Rajotte JC, Julian E, Diedhiou A, Radcliffe R, Clayton JL, Ortbahn D, Cummins J, Barbeau B, Murphy J, Darby B, Graff NR, Dostal TKH, Pray IW, Tillman C, Dittrich MM, Burns-Grant G, Lee S, Spieckerman A, Iqbal K, Griffing SM, Lawson A, Mainzer HM, Bealle AE, Edding E, Arnold KE, Rodriguez T, Merkle S, Pettrone K, Schlanger K, LaBar K, Hendricks K, Lasry A, Krishnasamy V, Walke HT, Rose DA, Honein MA, COVID-19 Response Team. Update: COVID-19 Among Workers in Meat and Poultry Processing Facilities — United States, April–May 2020. MMWR Morb Mortal Wkly Rep. 2020 Jul 10;69(27):887-892. doi: 10.15585/mmwr.mm6927e2.
Wilson RF, Sharma AJ, Schluechtermann S, Currie DW, Mangan J, Kaplan B, Goffard K, Salomon J, Casteel S, Mukasa A, Euhardy N, Ruiz A, Bautista G, Bailey E, Westergaard R, Gieryn D. Factors Influencing Risk for COVID-19 Exposure Among Young Adults Aged 18–23 Years — Winnebago County, Wisconsin, March–July 2020. MMWR Morb Mortal Wkly Rep. ePub: 2020 Oct 9. doi: http://dx.doi.org/10.15585/mmwr.mm6941e2
Yousaf AR, Duca LM, Chu V, Reses HE, Fajans M, Rabold EM, Laws RL, Gharpure R, Matanock A, Wadhwa A, Pomeroy M, Njuguna H, Fox G, Binder AM, Christiansen A, Freeman B, Gregory C, Tran CH, Owusu D, Ye D, Dietrich E, Pevzner E, Conners EE, Pray I, Rispens J, Vuong J, Christensen K, Banks M, O’Hegarty M, Mills L, Lester S, Thornburg NJ, Lewis N, Dawson P, Marcenac P, Salvatore P, Chancey RJ, Fields V, Buono S, Yin S, Gerber S, Kiphibane T, Dasu T, Bhattacharyya S, Westergaard R, Dunn A, Hall AJ, Fry AM, Tate JE, Kirking HL, Nabity S. A prospective cohort study in non-hospitalized household contacts with SARS-CoV-2 infection: symptom profiles and symptom change over time. Clin Infect Dis. 2020 Jul28:ciaa1072. doi:10.1093/cid/ciaa1072. Epub ahead of print.
Agizew T, Boyd R, Mathebula U, Mathoma A, Basotli J, Serumola C, Pals S, Finlay A, Lekone P, Rankgoane-Pono G, Tlhakanelo T, Chihota V, Auld AF. Outcomes of HIV-positive patients with non-tuberculous mycobacteria positive culture who received anti-tuberculous treatment in Botswana: Implications of using diagnostic algorithms without non-tuberculous mycobacteria. PLoS One. 2020 Jun 12;15(6):e0234646. doi: 10.1371/journal.pone.0234646.
Agizew T, Surie D, Oeltmann JE, Letebele M, Pals S, Mathebula U, Mathoma A, Kassa M, Hamda S, Pono P, Rankgoane-Pono G, Boyd R, Auld A, Finlay A. Tuberculosis preventive treatment opportunities at antiretroviral therapy initiation and follow-up visits. Public Health Action. 2020 Jun 21;10(2):64-69. doi: 10.5588/pha.19.0056.
Armstrong LR, Kammerer JS, Haddad MB. Diabetes mellitus among adults with tuberculosis in the USA, 2010-2017. BMJ Open Diabetes Res Care. 2020 Jul;8(1). doi: 10.1136/bmjdrc-2020-001275.
Beeler Asay GR, Lam CK, Stewart B, Mangan JM, Romo L, Marks SM, Bamrah Morris S, Gummo CL, Keh CE, Hill AN, Thomas A, Macaraig M, St John K, Ampie TJ, Chuck C, Burzynski, J. (2020). Cost of Tuberculosis Therapy Directly Observed on Video for Health Departments and Patients in New York City; San Francisco, California; and Rhode Island (2017-2018). Am J Public Health, 110(11), 1696-1703. doi:10.2105/ajph.2020.305877
Bisson GP, Bastos M, Campbell JR, Bang D, Brust JC, Isaakadis P, Lange C, Menzies D, Migliori GB, Pape JW,Palmero D, Baghei P, Tabarsi P, Viiklepp P, Vilbrun S, Walsh J, Marks SM. Mortality in adults with multidrug-resistant tuberculosis and HIV by antiretroviral therapy and tuberculosis drug use: an individual patient data meta-analysis. Lancet 2020;396:402–11. doi:10.1016/s0140-6736(20)31316-7
Cole B, Nilsen DM, Will L, Etkind SC, Burgos M, Chorba T. Essential Components of a Public Health Tuberculosis Prevention, Control, and Elimination Program: Recommendations of the Advisory Council for the Elimination of Tuberculosis and the National Tuberculosis Controllers Association. MMWR Recomm Rep. 2020 Jul 31; 69(7), 1-27. doi:10.15585/mmwr.rr6907a1
Cronin AM, Railey S, Fortune D, Wegener DH, Davis JB. Notes from the Field: Effects of the COVID-19 Response on Tuberculosis Prevention and Control Efforts – United States, March-April 2020. MMWR Morb Mortal Wkly Rep. 2020 Jul 24; 69(29), 971-972. doi:10.15585/mmwr.mm6929a4
Ershova JV, Volchenkov GV, Somova TR, Kuznetsova TA, Kaunetis NV, Kaminski D, Demikhova OV, ChernousovaLN, Vasilyeva IA, Kerr EM, Cegielski JP, Kurbatova EV. Impact of GeneXpert MTB/RIF® on treatment initiation and outcomes of RIF-resistant and RIF-susceptible TB patients in Vladimir TB Dispensary, Russia. BMC Infect Dis. 2020 Jul 25; 20(1), 543. doi:10.1186/s12879-020-05243-9
Fernando R, McDowell AC, Bhavaraju R, Fraimow H, Wilson JW, Armitige L, Haley C, Goswami ND. A model for bringing TB expertise to HIV providers: Medical consultations to the CDC-funded Regional Tuberculosis Training and Medical Consultation Centers, 2013-2017. PLoS One. 2020 Aug 31; 15(8). doi:10.1371/journal.pone.0236933
Figueroa A, Vonnahme L, Burrell K, Vera-García C, Gulati RK. CureTB and continuity of care for globally mobile patients. Int J Tuberc Lung Dis. 2020;24(7):694–9. doi:10.5588/ijtld.19.0486
Hedges KNC, Borisov AS, Saukkonen JJ, Scott NA, Hecker EJ, Bozeman L, Dukes Hamilton C, Kerrigan A, Bessler P, Moreno-Martinez A, Arevalo B, Goldberg SV. Nonparticipation reasons in a randomized international trial of a new latent tuberculosis infection regimen. Clin Trials. 2020 Feb;17(1):39-51. doi: 10.1177/1740774519885380.
Iqbal SA, Isenhour CJ, Mazurek G, Truman BI. Diagnostic code agreement for electronic health records and claims data for tuberculosis. Int J Tuberc Lung Dis. 2020 Jul 1;24(7):706-711. doi: 10.5588/ijtld.19.0792.
Jenks JD, Garfein RS, Zhu W, Hogarth M. Latent Tuberculosis Screening Using Electronic Health Record Data. Emerg Infect Dis. 2020; 26(9), 2285-2287. doi:10.3201/eid2609.191391
Jo Y, Shrestha S, Gomes I, Marks S, Hill A, Asay G, and Dowdy D. Model-Based Cost-Effectiveness of State-level Latent Tuberculosis Interventions in California, Florida, New York and Texas. Clin Infect Dis. 2020 Jun 25;ciaa857. doi:10.1093/cid/ciaa857.
Kerr EM, Vonnahme LA, Goswami ND. Impact of targeted local interventions on tuberculosis awareness and screening among persons experiencing homelessness during a large tuberculosis outbreak in Atlanta, Georgia, 2015–2016. Public Health Rep 2020;135(1 Suppl):90S–9S. doi:10.1177/0033354920932644
Liu Y, Phares CR, Posey DL, Maloney SA, Cain KP, Weinberg MS, Schmit KM, Marano N, Cetron MS. Tuberculosis among newly arrived immigrants and refugees in the United States. Ann Am Thorac Soc. 2020 Jul 30. doi:10.1513/AnnalsATS.201908-623OC. Epub ahead of print.
Marks SM, Dowdy DW, Menzies NA, Shete PB, Salomon JA, Parriott A, Shrestha S, Flood J, Hill AN. Policy implications of mathematical modeling of latent tuberculosis infection testing and treatment strategies to accelerate tuberculosis elimination. Public Health Rep 2020;135(1 Suppl):38S–43S. doi:10.1177/0033354920912710
Marks SM, Katz DJ, Davidow AL, Pagaoa MA, Teeter LD, Graviss EA. The impact of HIV infection on TB disparities among US-born black and white tuberculosis patients in the United States. J Public Health Manag Pract 2020;26(5):E5–12. doi:10.1097/phh.0000000000000949
Menzies NA, Bellerose M, Testa C, Swartwood N, Malyuta Y, Cohen T, Marks SA, Hill AN, Date AA, Maloney SA, Bowden SE, Grills AW, Salomon JA. Impact of Effective Global Tuberculosis Control on Health and Economic Outcomes in the United States. Am J Respir Crit Care Med. 2020 Jul 9; doi:10.1164/rccm.202003-0526OC
Menzies NA, Parriott A, Shrestha S, Dowdy DW, Cohen T, Salomon JA, Marks SM, Hill AN, Winston CA, Asay GB, Barry PM, Readhead A, Flood J, Kahn JG, Shete PB. Comparative modelling of TB epidemiology and policy outcomes in California. Am J Respir Crit Care Med. 2020 Feb 1; 201(3):356-365. doi: 10.1164/rccm.201907-1289OC.
Menzies NA, Swartwood N, Testa C, Malyuta Y, Hill AN, Marks SM, Cohen T, Salomon, JA. Time since infection and risks of future disease for individuals with Mycobacterium tuberculosis infection in the United States. Epidemiol. 2020. doi:10.1097/ede.0000000000001271
Miele K, Bamrah Morris S, Tepper NK. Tuberculosis in Pregnancy. Obstet Gynecol. 2020 Jun;135(6):1444-1453. doi: 10.1097/AOG.0000000000003890.
Miller AP, Malekinejad M, Horváth H, Blodgett JC, Kahn JG, Marks SM. Healthcare facility-based strategies to improve tuberculosis testing and linkage to care in non-U.S.-born populations in the United States: A systematic review. PLoS One. 2019; 14(9):e0223077. doi: 10.1371/journal.pone.0223077.
Muloma E, Stewart R, Townsend H, Koch S, Burkholder S, Railey S, White K, Redington-Noble, R, Caine, V. Multipronged Approach to Controlling a Tuberculosis Outbreak Among Persons Experiencing Homelessness. J Public Health Manag Pract. 2020 Sept 9. doi:10.1097/phh.0000000000001211 Epub ahead of print.
Nahid P, Mase SR, Migliori GB, Sotgiu G, Bothamley GH, Brozek JL, Cattamanchi A, Cegielski JP, Chen L, Daley CL, Dalton TL, Duarte R, Fregonese F, Horsburgh CR Jr, Ahmad Khan F, Kheir F, Lan Z, Lardizabal A, Lauzardo M, Mangan JM, Marks SM, McKenna L, Menzies D, Mitnick CD, Nilsen DM, Parvez F, Peloquin CA, Raftery A, Schaaf HS, Shah NS, Starke JR, Wilson JW, Wortham JM, Chorba T, Seaworth B. Treatment of Drug-Resistant Tuberculosis. An Official ATS/CDC/ERS/IDSA Clinical Practice Guideline. Am J Respir Crit Care Med. 2019 Nov 15;200(10):e93-e142. doi: 10.1164/rccm.201909-1874ST.
Reichler MR, Hirsch C, Yuan Y, Khan A, Dorman SE, Schluger N, Sterling TR; Tuberculosis Epidemiologic Studies Consortium Task Order 2 Team. Predictive value of TNF-α, IFN-γ, and IL-10 for tuberculosis among recently exposed contacts in the United States and Canada. BMC Infect Dis 2020 Jul 31;20(1):553. doi:10.1186/s12879-020-05185-2
Schmit KM, Shah N, Kammerer S, Marks SM, Bamrah Morris S. Factors Associated with Recent Tuberculosis Transmission or Mortality during Tuberculosis Treatment among Persons Living with HIV, United States, 2011–2016. J Racial Ethn Health Disparities. 2020 doi: 10.1007/s40615-020-00709-7.
Shrestha S, Parriott A, Menzies NA, Shete PB, Hill AN, Marks SM, Dowdy DW. Estimated population-level impact of using a six-week regimen of daily rifapentine to treat latent tuberculosis infection in the United States. Ann Am Thorac Soc. 2020 Sep 11. doi: 10.1513/AnnalsATS.202005-574RL. Epub ahead of print.
Stewart RJ, Wortham J, Parvez F, Morris SB, Kirking HL, Cameron LH, Cruz AT. (2020). Tuberculosis Infection in Children. J Nurse Pract. doi: 10.1016/j.nurpra.2020.06.027
Talwar A, Stewart R, Althomsons SP, Rinsky J, Jackson DA, Galvis ME, Graham P, Huaman MA, Karrer J, Kondapally K, Mitchell S, Wortham J, de Fijter S. Notes from the Field: Multidrug-resistant tuberculosis among workers at two food processing facilities—Ohio, 2018–2019. MMWR Morb Mortal Wkly Rep 2020;69:1104–5. doi: 10.15585/mmwr.mm6932a6
Thanassi W, Behrman AJ, Reves R, Russi M, Swift M, Warkentin J, Miyakawa R, Wegener D, Budnick L, Murray E, Scarpita A, Hurst BJ, Foster-Chang S, Mathew T, Gruden MA, Higashi J, Hudson III, TW. Tuberculosis Screening, Testing, and Treatment of US Health Care Personnel: ACOEM and NTCA Joint Task Force on Implementation of the 2019 MMWR Recommendations. J Occup Environ. 2020 Jul; 62(7). doi:10.1097/jom.0000000000001904
Yelk Woodruff R, Hill A, Marks S, Navin T, Miramontes R. Estimated latent tuberculosis infection prevalence and tuberculosis reactivation rates among non-U.S.-born residents in the United States, from the 2011–2012 National Health and Nutrition Examination Survey. J Immigr Minor Health. 2020 Aug 5. doi: 10.1007/s10903-020-01065-8. Epub ahead of print.
To receive the TB Notes Newsletter, enter your email address at the bottom of the TB Notes webpage. If you would like to submit an article or update in TB Notes, please email Meredith Moore at mue1@cdc.gov.
You can follow us on Twitter @CDC_TB and Facebook @CDCTB and sign up for email updates through Adobe Campaign.