TB and Black or African American Persons
Since 1993, the rates of TB in the United States have declined in almost all racial and ethnic groups. Rates of TB disease in Black or African American persons* have been nearly cut in half (from 6.2 cases per 100,000 persons in 2011 to 3.4 cases per 100,000 persons in 2021) over the past decade.
However, Black or African American persons in the United States continue to be affected by TB at a greater rate compared to White persons.
Addressing the TB disparity among Black or African American persons is an important priority; prevention and control efforts should be targeted to this population.
By the Numbers
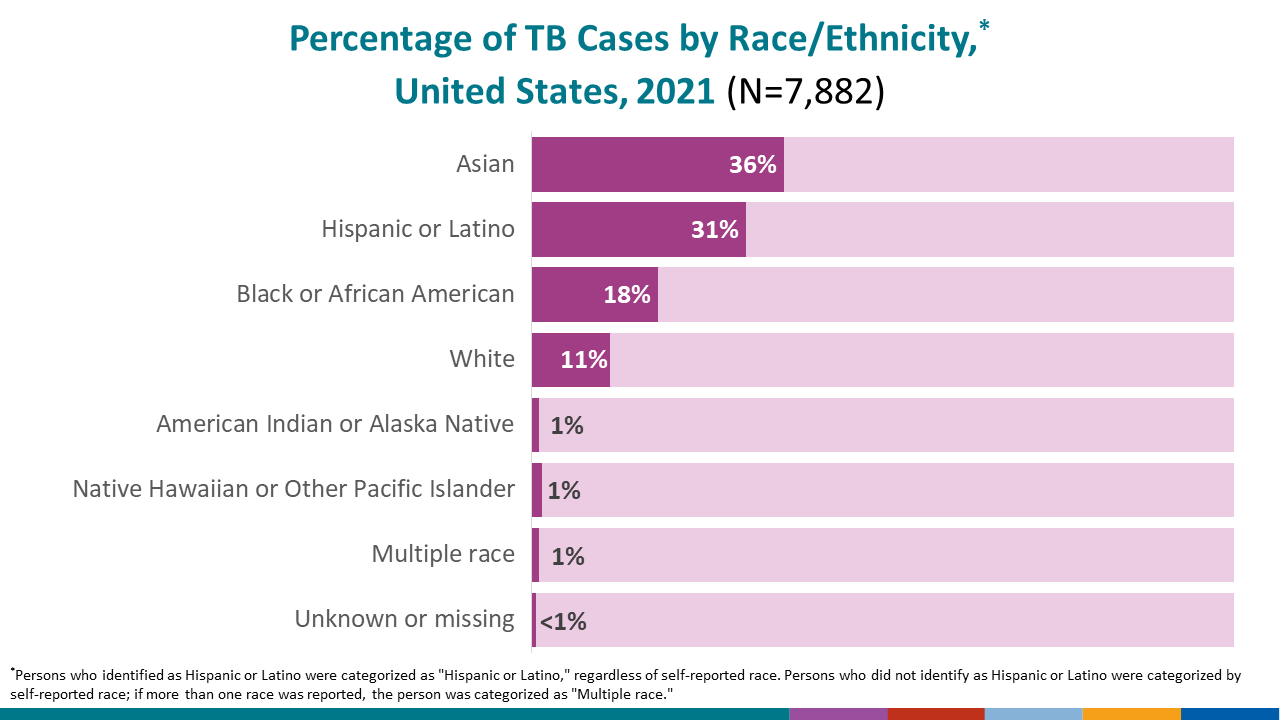
In 2021, U.S. state, local, and territorial health agencies reported a total of 7,882 TB cases to CDC.
- In 2021, TB disease was reported in 1,420 non-Hispanic Black or African American persons in the United States, accounting for 18.0% of all people reported with TB disease nationally.
- The rate of TB disease among Black or African American persons is 3.4 cases per 100,000 persons.
- The TB case rate is 8 times higher for non-Hispanic Black or African American persons than for non-Hispanic White persons.
- Read more in Reported Tuberculosis in the United States, 2021.
Prevention Challenges
TB is a challenging disease to diagnose, treat, and control. Dwindling resources and loss of public health capacity, including access to care, and maintaining clinical and public health expertise, add to the challenge. It is critical to reach those populations at highest risk for TB, and to identify and implement innovative strategies to improve diagnosis and treatment.
Ending TB will require a dual approach of maintaining and strengthening current TB control priorities, while increasing efforts to identify and treat latent TB infection in populations at risk for TB disease.
Similar to other racial and ethnic minority groups, Black or African American persons face a number of challenges that contribute to higher rates of TB. Challenges may include:
- Treatment Duration and Completion
- Treatment for TB disease can be lengthy. Patients are often unable or reluctant to take medication for several months. For people with TB disease, inadequate treatment can lead to treatment failure, relapse, ongoing transmission, and development of drug resistance.
- For people with latent TB infection, treatment for a condition with no symptoms of illness may not be a priority.
- Socioeconomic Factors
- People experiencing poverty, including those with limited access to quality health care, employment opportunities, housing, and transportation, and those who disproportionately experience adverse health outcomes. These factors can directly or indirectly increase the risk for TB disease and present barriers to treatment.
- Language and cultural barriers, including health knowledge, stigma associated with the disease, values, and beliefs may also place certain populations at higher risk. Stigma may deter people from seeking medical care or follow up care.
- HIV and Other Medical Conditions
- TB remains a serious threat, especially for people with human immunodeficiency virus (HIV). People with HIV are more likely than people who do not have HIV to get sick with other infections and diseases, including TB.
- Without treatment, as with other opportunistic infections, HIV and TB can shorten the life of the person infected.
- In addition to HIV, other underlying medical conditions may increase the risk that latent TB infection will progress to TB disease. For example, the risk is higher in people with diabetes, substance abuse (including injection of illegal drugs), silicosis, or those undergoing medical treatments with corticosteroids.
- TB remains a serious threat, especially for people with human immunodeficiency virus (HIV). People with HIV are more likely than people who do not have HIV to get sick with other infections and diseases, including TB.
* Note: Persons who identified as Hispanic or Latino were categorized as “Hispanic or Latino,” regardless of self-reported race. Persons who did not identify as Hispanic or Latino were categorized by self-reported race; if more than one race was reported, the person was categorized as “Multiple race.”
Additional References
Marks SM, Katz DJ, Davidow AL, Pagaoa MA, Teeter LD, Graviss EA. The Impact of HIV Infection on TB Disparities Among US-Born Black and White Tuberculosis Patients in the United States. J Public Health Manag Pract. 2019.
Khan A, Marks S, Katz D, Morris SB, Lambert L, Magee E, Bowman S, Grant G. Changes in Tuberculosis Disparities at a Time of Decreasing Tuberculosis Incidence in the United States, 1994-2016. Am J Public Health. 2018;108(S4):S321-S326.
Royce RA, Colson PW, Woodsong C, Swinson-Evans T, Walton W, Maiuri A, DeLuca N; Tuberculosis Epidemiologic Studies Consortium (TBESC). Tuberculosis Knowledge, Awareness, and Stigma Among African-Americans in Three Southeastern Counties in the USA: a Qualitative Study of Community Perspectives. J Racial Ethn Health Disparities. 2017;4(1):47-58.
Howley MM, Rouse CD, Katz DJ, Colson PW, Hirsch-Moverman Y, Royce RA; Tuberculosis Epidemiologic Studies Consortium. Knowledge and Attitudes About Tuberculosis Among U.S.-Born Blacks and Whites with Tuberculosis. J Immigr Minor Health. 2015;17(5):1487-95.
Pagaoa MA, Royce RA, Chen MP, Golub JE, Davidow AL, Hirsch-Moverman Y, Marks SM, Teeter LD, Thickstun PM, Katz DJ; Tuberculosis Epidemiologic Studies Consortium. Risk factors for transmission of tuberculosis among United States-born African Americans and Whites. Int J Tuberc Lung Dis. 2015;19(12):1485-92.
- Questions and Answers About Tuberculosis (available in multiple languages)
- Tuberculosis – The Connection between TB and HIV (The AIDS Virus) (Pamphlet)
- TB and HIV/AIDS (fact sheet)
- Patient Education Materials Series (English, Spanish, Tagalog, Vietnamese)
- TB Treatment Information and Medication Trackers
- TB Personal Stories