TB and Asian Persons
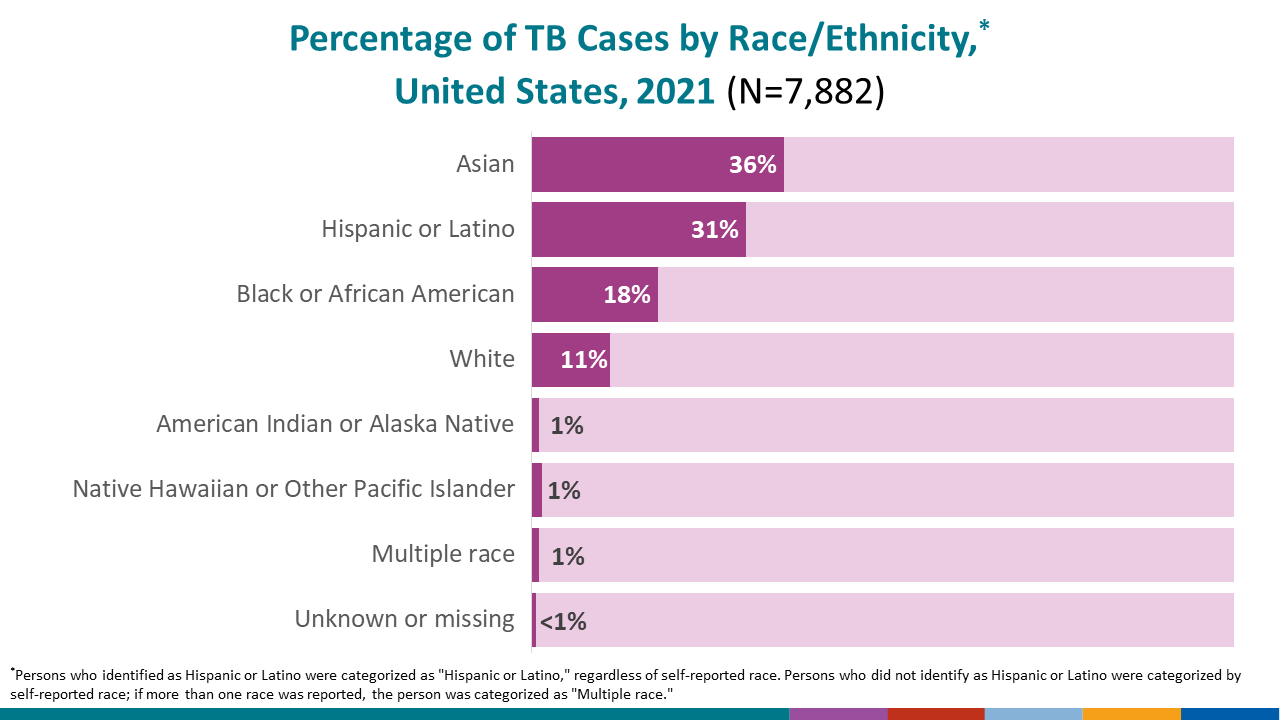
In 2021, a total of 7,882 TB cases were reported in the United States; however, Asian persons* continue to be affected by TB at a greater rate compared to other racial and ethnic minority groups.
Several important factors contribute to the higher rates of TB among racial and ethnic minority groups, including Asian persons. These factors include being born in a country with a high rate of TB disease or travel to a country with a high rate of TB disease.
By the Numbers
In 2021, U.S. state, local, and territorial health agencies reported a total of 7,882 TB cases to CDC.
- In 2021, TB disease was reported in 2,834 Asian persons in the United States, accounting for 36.0% of all people reported with TB disease nationally.
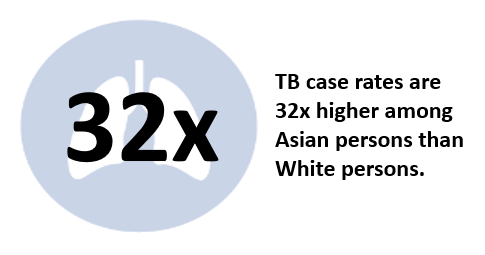
- The rate of TB disease among Asian persons is 14.4 cases per 100,000 persons.
- The TB case rate is 32 times higher for Asian persons than for non-Hispanic White persons.
- Being born in or traveling to countries with a high rate of TB disease increases a person’s risk of becoming sick with TB disease. The most common countries of birth among non-U.S.–born Asian persons with TB disease in 2021 were
-
- Philippines; 12.3%,
- India; 10.2%,
- Vietnam; 7.5%,
- China; 5.6%
- Myanmar; 1.8%
- Read more in Reported Tuberculosis in the United States, 2021.
Prevention Challenges
TB is a challenging disease to diagnose, treat, and control. Dwindling resources and loss of public health capacity, including access to care, and maintaining clinical and public health expertise, add to the challenge. It is critical to reach those populations at highest risk for TB, and to identify and implement innovative strategies to improve diagnosis and treatment.
Ending TB will require a dual approach of maintaining and strengthening current TB control priorities, while increasing efforts to identify and treat latent TB infection in populations at risk for TB disease.
CDC’s Think. Test. Treat TB campaign aims to reach those most at risk for latent TB infection and their healthcare providers to encourage TB testing and accelerate elimination of this treatable disease. Think. Test. Treat TB is the first national multilingual communications campaign to increase testing for latent TB infection, a major health disparity among Asian Americans.
Similar to other racial and ethnic minority groups, Asian persons face a number of challenges that contribute to higher rates of TB. Challenges may include:
- Testing and Diagnosis
- Many people born outside of the United States have been given a vaccine for TB called BCG. Vaccination with BCG may cause a false positive reaction to a TB skin test. A positive reaction to a TB skin test may be due to the BCG vaccine itself or due to infection with TB bacteria. TB blood tests are the preferred method of TB testing for people who have received the BCG vaccine. TB blood tests are not affected by prior BCG vaccination and do not give a false-positive result in people who have received the BCG vaccine.
- Treatment Duration and Completion
- Treatment for TB disease can be lengthy. Patients are often unable or reluctant to take medication for several months. For people with TB disease, inadequate treatment can lead to treatment failure, relapse, ongoing transmission, and development of drug resistance.
- For people with latent TB infection, treatment for a condition with no symptoms of illness may not be a priority.
- Socioeconomic Factors
- People experiencing poverty, including those with limited access to quality health care, employment opportunities, housing, and transportation, and those who disproportionately experience adverse health outcomes. These factors can directly or indirectly increase the risk for TB disease and present barriers to treatment.
- Language and cultural barriers, including health knowledge, stigma associated with the disease, values, and beliefs may also place certain populations at higher risk for TB. Stigma may deter people from seeking medical care or follow up care.
* Note: Persons who identified as Hispanic or Latino were categorized as “Hispanic or Latino,” regardless of self-reported race. Persons who did not identify as Hispanic or Latino were categorized by self-reported race; if more than one race was reported, the person was categorized as “Multiple race.”
- Think. Test. Treat TB Education Materials
- Questions and Answers About Tuberculosis (available in multiple languages)
- Patient Education Materials Series (English, Spanish, Tagalog, Vietnamese)
- TB Treatment Information and Medication Trackers
- TB Personal Stories
- Think. Test. Treat TB
CDC’s campaign to raise awareness of latent TB infection
- Trends in Tuberculosis, 2021
- 2021 TB Statistics
- Reported Tuberculosis in the United States, 2021
- Disparities in HIV, Viral Hepatitis, STDs, and TB
- NCHHSTP AtlasPlus
- Find TB Resources
- TB Elimination Alliance
The TB Elimination Alliance is a national partnership of community leaders dedicated to eliminating TB and latent TB infection inequities among Asian American and Native Hawaiian/Pacific Islander populations through education, raising awareness, and innovation.