Tuberculosis (TB) Screening, Testing, and Treatment of U.S. Health Care Personnel Frequently Asked Questions (FAQs)
On May 17, 2019, the Centers for Disease Control and Prevention (CDC) and the National Tuberculosis Controllers Association (NTCA) released updated recommendations for TB screening, testing, and treatment of health care personnel. These recommendations update the health care personnel screening and testing section of the 2005 CDC Guidelines for Preventing the Transmission of Mycobacterium tuberculosis in Health-Care Settings. The recommendations for facility risk assessments and infection control practices are unchanged from the 2005 guidelines.
Key Changes in the Recommendations
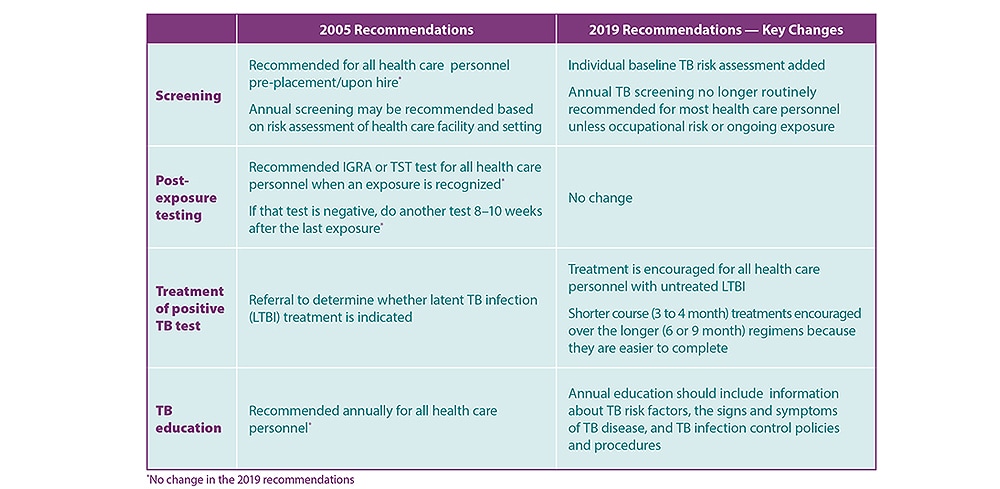
Summary of updates to TB Screening, Testing, and Treatment Recommendations of U.S. Health Care Personnel
The changes in recommendations reflect the overall decrease in the number of people diagnosed with TB disease and the low incidence of TB due to occupational exposure among health care personnel in the United States.
Experts from the National TB Controllers Association (NTCA), state and local public health departments, academia, occupational health associations, and CDC developed the recommendations after conducting a systematic review of scientific studies on TB screening and testing of health care personnel.
CDC and the National TB Controllers Association (NTCA) recommend that all U.S. health care personnel be screened for TB upon hire (i.e., pre-placement). Pre-placement screening should include a TB risk assessment, a TB symptom screen, and a TB test. These recommendations should be used for people who work or volunteer in health care settings, including: inpatient and outpatient settings, laboratories, emergency medical services (EMS), medical settings in correctional facilities, home-based health care and outreach settings, long-term care facilities, and homeless shelters.
CDC and NTCA do not recommend annual TB testing for health care personnel unless there is a known exposure or ongoing transmission in a health care setting.
All health care personnel should receive TB education annually. TB education should include information on TB risk factors, the signs and symptoms of TB disease, and TB infection control policies and procedures. TB education materials can be found through CDC, the TB Centers of Excellence for Training, Education, and Medical Consultation, NTCA, State TB Programs, and the Find TB Resources website.
TB screening is a process that includes an individual risk assessment, a symptom evaluation, a TB test (e.g., a TB blood test or a TB skin test), and additional evaluation for TB disease as needed.
Health care personnel should be screened for TB upon hire (i.e., pre-placement). Annual TB testing is not recommended unless there is a known exposure or ongoing transmission.
A positive TB test only tells that a person has been infected with TB bacteria. It does not tell whether the person has latent TB infection (LTBI) or has progressed to TB disease. Health care personnel with a positive TB test result should receive a symptom evaluation and chest x-ray to rule out TB disease.
Treatment for LTBI is strongly encouraged for health care personnel diagnosed with LTBI. Shorter treatment regimens, including once-weekly isoniazid and rifapentine for 3 months and daily rifampin for 4 months, should be used as they are more likely to be completed when compared to the traditional regimens of 6 or 9 months of isoniazid. However, ultimately, taking treatment for latent TB infection is a decision a person should make together with their health care provider.
Health care personnel with untreated LTBI should receive a yearly TB symptom screen to detect early evidence of TB disease and to evaluate the risks and benefits of LTBI treatment.
Health-care facilities might consider using serial TB screening for certain groups at increased occupational risk for TB exposure (e.g., pulmonologists or respiratory therapists) or in certain settings if transmission has occurred in the past (e.g., emergency departments). Facilities should work with their state and local health departments to help make these decisions.
State and local TB screening and testing regulations may have different requirements. The CDC and the National TB Controllers Association (NTCA) TB screening and testing recommendations do not override or replace state regulations. For TB regulations in your area, please contact your state or local TB control program.
Either a TB blood test or a TB skin test can be used to test for TB infection. For consistency, the same type of TB test should be used upon hire (i.e., pre-placement) and for any follow-up testing.
If the TB skin test is used to test for TB infection upon hire (i.e., pre-placement), two-step testing should be conducted. Two-step testing is NOT required for TB blood tests.
Health care personnel with a positive TB test result should receive a symptom evaluation and chest x-ray to rule out TB disease. Additional workup may be needed based on these results.
The health care personnel’s local health department should be notified immediately if TB disease is suspected.
Treatment for latent TB infection (LTBI) is strongly encouraged for health care personnel diagnosed with LTBI. Shorter treatment regimens, including once-weekly isoniazid and rifapentine for 3 months and daily rifampin for 4 months, should be used as they are more likely to be completed when compared to the traditional regimens of 6 or 9 months of isoniazid.
If health care personnel with LTBI do not take LTBI treatment, they should receive an annual TB symptom screen.
Information from the individual TB risk assessment and symptom evaluation help to interpret the results of a TB blood test or TB skin test upon hire (i.e., pre-placement). Risk factors for TB include
- exposure to TB disease,
- time spent in countries where TB is common (e.g., born in or frequent travel to countries with a high rate of TB), and
- current or planned immune system suppression (e.g., HIV infection or taking medication that suppresses the immune system).
A sample risk assessment tool is available here.
The risk assessment and symptom evaluation help guide decisions when interpreting test results. Low-risk health care personnel who test positive for TB infection should have a second TB test to confirm the result. For example, health care personnel with a positive TB test who do not have any TB symptoms are unlikely to be infected and are at low risk for progression to TB disease. These persons should receive a second confirmatory TB test. A positive TB test only tells that a person has been infected with TB bacteria. It does not tell whether the person has latent TB infection (LTBI) or has progressed to TB disease. If the second test is also positive, the health care personnel is considered to have TB infection and should be evaluated with a chest x-ray and TB symptom screen to rule out TB disease.
Treatment for LTBI is strongly encouraged for health care personnel diagnosed with LTBI. Shorter treatment regimens, including once-weekly isoniazid and rifapentine for 3 months and daily rifampin for 4 months, should be used as they are more likely to be completed when compared to the traditional regimens of 6 or 9 months of isoniazid.
Health care personnel with a documented history of a prior positive TB test should receive an individual TB risk assessment and TB symptom screen upon hire (i.e., pre-placement). Additionally, individuals with a prior positive TB test should receive a chest x-ray or provide documentation of a normal chest x-ray. Requirements regarding acceptable documentation may be determined by local or state regulations. Repeating the TB test (e.g., TB blood test or TB skin test) is not required.
Treatment for LTBI is strongly encouraged for health care personnel diagnosed with LTBI. Shorter treatment regimens, including once-weekly isoniazid and rifapentine for 3 months and daily rifampin for 4 months, should be used as they are more likely to be completed when compared to the traditional regimens of 6 or 9 months of isoniazid.
Health care personnel with untreated LTBI should receive a yearly symptom screen to detect early evidence of TB disease and to reevaluate the risks and benefits of LTBI treatment. Repeat chest x-rays are not required unless health care personnel are symptomatic or as part of the repeat evaluation prior to starting LTBI treatment.
All health care personnel with a known exposure to TB disease should receive a symptom screen and timely testing, if indicated.
- Health care personnel with a previous negative TB test result should be tested immediately and re-tested 8 to 10 weeks after the last known exposure. For consistency, the same type of TB test (e.g., TB blood test or TB skin test) should be used at hire (i.e., pre-placement) and for any follow-up testing.
- Health care personnel with a documented history of a positive TB test result do not need to be re-tested after exposure to TB. They should receive a TB symptom screen, and if they have symptoms of TB, they should be evaluated for TB disease.
Yes. Health care personnel are strongly encouraged to take treatment for LTBI to prevent the development of TB disease. Several treatment regimens are available, including short-course regimens. Shorter treatment regimens, including once-weekly isoniazid and rifapentine for 3 months and daily rifampin for 4 months, should be used as they are more likely to be completed when compared to the traditional regimens of 6 or 9 months of isoniazid.
Symptoms for TB disease include any of the following: a cough lasting longer than three weeks, unexplained weight loss, night sweats or a fever, and loss of appetite.
Please contact your state or local TB control program for information regarding TB regulations in your area.
- Fact Sheets on Tuberculosis
- Tuberculosis Screening, Testing, and Treatment of U.S. Health Care Personnel: Recommendations from the National Tuberculosis Controllers Association and CDC
- Health Care Settings
- TB Screening and Testing of Health Care Personnel
- National TB Controllers Association
- Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005
- State TB Control Offices
- Testing and Diagnosis Guidelines
- Using the Isoniazid/Rifapentine Regimen to Treat Latent Tuberculosis Infection (LTBI)
- Questions and Answers About TB
- CDC Info