TB NOTES

TB Notes 4, 2019
Notes from the Director
Dear Colleague:

The end of the year marks a time to reflect on achievements, and an opportunity to look forward to future goals. In 2019, I saw many outstanding efforts in the service of our collective mission to prevent, control, and eventually eliminate tuberculosis (TB) in the United States. Thank you for your continued commitment and all that you did this past year.
The end of 2019 was marked by significant updates and activities. In December 2019, the Advisory Council for the Elimination of Tuberculosis (ACET) convened in Atlanta to provide advice and recommendations regarding the elimination of TB in the United States. The meeting included presentations from DTBE, NCHHSTP leadership, the Division of Global Migration and Quarantine, Project ECHO partners, state and local health department partners, and ACET workgroup members.
In November 2019, CDC, in partnership with the American Thoracic Society (ATS), the Infectious Diseases Society of America (IDSA), and the European Respiratory Society, published new practice guidelines for the Treatment of Drug-Resistant Tuberculosis. The new guidelines, published in the American Journal of Respiratory and Critical Care Medicine, provide recommendations for treating multidrug-resistant tuberculosis (MDR TB) and extensively drug-resistant tuberculosis (XDR TB), as well as isoniazid-resistant TB.
Additionally, CDC released a new, free Continuing Education Activity from MMWR and Medscape related to the updated screening, testing, and treatment recommendations for U.S. health care personnel. This activity adds to the many resources and tools available, including FAQs, a Baseline Individual TB Risk Assessment form, an infographic, a video summarizing the new recommendations, and a Medscape Expert Commentary video featuring CDC’s Dr. Sapna Bamrah Morris.
I am proud to work alongside you as we apply innovation and scientific excellence to fulfill our mission and implement strategies for TB elimination. Best wishes for a happy and healthy new year!
Philip LoBue, MD, FACP, FCCP
Director
Division of Tuberculosis Elimination
National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention
Division of Tuberculosis Elimination

This year the Division of Tuberculosis Elimination (DTBE) would like to reflect on the research, resources, and events that shaped a momentous year. Here is a look back at some TB highlights for 2019.
On March 24, 2019, DTBE recognized World TB Day, an annual event to commemorate the date in 1882 when Dr. Robert Koch announced his discovery of Mycobacterium tuberculosis, the bacillus that causes tuberculosis (TB). The 2019 World TB Day theme was “It’s Time!” Activities in 2019 included the CDC U.S. TB Elimination Champions Project, a World TB Day Social Media Photo Challenge, the release of six short World TB Day Personal Stories videos, a World TB Day Twitter Storm, and a World TB Day event cohosted by DTBE and the Division of Global HIV and TB.
In April, public health laboratorians attended the APHL 11th National Conference on Laboratory Aspects of TB and the 2019 National TB Controllers Association (NTCA) National TB Conference held in Atlanta, Georgia. During the conference DTBE released an addition of a new educational module, Mycobacteriology False-Positive Case Studies to the Essentials for the Mycobacteriology Laboratory Promoting Quality Practices training module series. In this module, laboratorians can navigate through five real-world cases in which a false-positive MTBC result may have been reported.
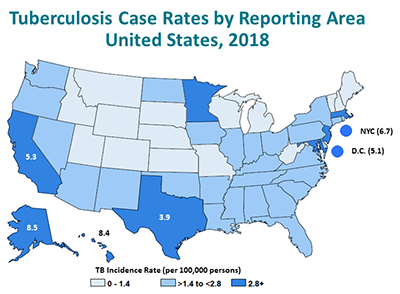
DTBE published the 2018 surveillance report, Reported Tuberculosis in the United States, 2018. This was the first edition of the annual surveillance report published exclusively online. During 2018, the United States again reported the lowest number of TB cases (9,025) and lowest incidence rate (2.8 cases per 100,000 persons) on record. Although TB in the United States continues to decrease each year, the rate of decrease remains low. This low rate of decrease is most evident among the U.S.-born population, although most of reported TB cases continue to occur among non-U.S.–born persons.

In September, DTBE released the national TB program objectives and performance targets for 2025. The national objectives include decreasing TB incidence rates for both US-born (0.4 cases per 100,000) and non-US—born populations (8.8 cases per 100,000), as well as for US-born minorities (1.0 case per 100,000) and children less than five years of age (0.1 cases per 100,000). The objectives incorporate key process indicators for patient management, laboratory reporting, contact investigations of infectious TB patients, and follow-up examination of immigrants and refugees who recently arrived in the United States with Class B notifications.
Additionally, in September , the Republic of Palau and Global TB Institute co-hosted the Pacific Islands TB Controllers Association (PITCA) Conference and TB Surveillance Training. This event assembled TB experts from throughout the Pacific Islands and U.S. to engage in learning and discussion on the management and control of TB and provided training and networking opportunities for TB professionals in the region. On September 16–18, 2019, the Republic of Palau hosted a TB Surveillance Training following the 2019 PITCA Conference. There were 27 participants at the training, which included representatives from five of the USAPI jurisdictions.

In October, DTBE released the personal stories of four people diagnosed and treated for tuberculosis (TB) disease or latent TB infection. These stories are part of DTBE’s ongoing TB Personal Stories series to help raise awareness about TB in the United States. You can view the video, print, and social media content for each story by visiting CDC’s TB Personal Stories website. DTBE would like to thank We Are TB, The National TB Controllers Association, and the Stop TB USA for their contributions to this project.
Each year we recognize World TB Day on March 24 with a variety of activities leading up to the official day. This annual event commemorates the date Dr. Robert Koch announced his discovery of the bacillus that causes tuberculosis (TB). The Centers for Disease Control and Prevention (CDC) joins our international partners by adapting the global Stop TB Partnership’s 2020 World TB Day theme, which will once again be “It’s Time.”
Activities for this year’s World TB Day will include:
- 2020 CDC U.S. TB Elimination Champions Project: This year, the DTBE is seeking photo submissions from organizations or individuals that represent their work and commitment to the “It’s Time to End TB!” mission.
- World TB Day Social Media Photo Challenge: Share your own “It’s Time” message! Download the template, write your World TB Day message, and post on Twitter, Facebook, and Instagram.
- World TB Day Activities Map: If you are planning an event around the 2020 World TB Day, we would like to add it to our map.
More information on these activities can be found on the CDC’s World TB Day website, a one-stop-shop for resources and information, including:
- Digital Media Toolkit which includes social media, graphics, posters, and videos
- World TB Day Key Messages and Resources
Revised Self-Study Modules on Tuberculosis, 1-5, Now Available to Order
The CDC Division of Tuberculosis Elimination (DTBE) is pleased to announce that the Self-Study Modules on Tuberculosis, 1-5 are now available to order. If you would like to request a print copy of the modules, please use the CDC online ordering system: http://wwwn.cdc.gov/pubs/CDCInfoOnDemand.aspx.
The modules are designed to provide basic information about tuberculosis (TB) in a self-study format for outreach workers, nurses, physicians, administrators, health educators, and students. Originally developed in 1995, these booklets have served as an important resource in training new TB control workers for over two decades. The modules have recently been updated with the latest TB treatment recommendations and surveillance data.
The Self-Study Modules on Tuberculosis, 1-5 packet includes an introduction, five modules, and a glossary:
Introduction
Module 1: Transmission and Pathogenesis of Tuberculosis
Module 2: Epidemiology of Tuberculosis
Module 3: Targeted Testing and the Diagnosis of Latent Tuberculosis Infection and Tuberculosis Disease
Module 4: Treatment of Latent Tuberculosis Infection and Tuberculosis Disease
Module 5: Infectiousness and Infection Control
Glossary
Continuing education for Modules 1-5 is offered free of charge for various professions. For more information on continuing education, visit: www.cdc.gov/tb/education/ssmodules/cont_ed_regist.htm.
Companion Product
The Self-Study Modules on Tuberculosis, 6-9 provide programmatic TB information. The Modules 6-9 packet includes an introduction, four modules, and a glossary:
Introduction
Module 6: Managing Tuberculosis Patients and Improving Adherence
Module 7: Patient Rights and Confidentiality in Tuberculosis Control
Module 8: Contact Investigations for Tuberculosis
Module 9: Tuberculosis Outbreak Detection and Response
Glossary
To view Modules 6-9 online, visit the DTBE website: www.cdc.gov/tb/education/ssmodules/default.htm. To order hardcopies, visit the CDC online ordering system: http://wwwn.cdc.gov/pubs/CDCInfoOnDemand.aspx?Pubid=221235.
Continuing education for Modules 6-9 is offered free of charge for various professions. For more information on continuing education, visit: www.cdc.gov/tb/education/ssmodules/cont_ed_regist6_9.htm.
If you have questions about the Self-Study Modules on Tuberculosis, please contact Sarah Segerlind at ssegerlind@cdc.gov or Carissa Sera-Josef at cserajosef@cdc.gov.
Submitted by Sarah Segerlind
Follow the Call of the Disco Ball!

DTBE was feeling like funky town this holiday season! That’s because the Communications, Education, and Behavioral Studies Branch (CEBSB) proudly unveiled the 2019 holiday theme – Arctic Disco!
Joan Mangan, Behavioral Scientist and disco inferno mastermind, led the 2019 holiday theme and wouldn’t stop ‘til she got enough. The festive scene is not only entertaining, but educational as well – with a holiday tree adorned with bacteria, lungs, and pill bottles.
Visitors who boogied over to the 4th floor lobby saw Dr. LoBear, the Disco Hulk, a field dressed deer, and more. Those who weren’t feeling the disco fever were about to catch up on TB history by reading the bedazzled TB icon ornaments.
New Drug-Resistant TB Treatment Guidelines

In November 2019, DTBE released new practice guidelines for the Treatment of Drug-Resistant Tuberculosis. The guidelines were published in the American Journal of Respiratory and Critical Care Medicine and developed by CDC, the American Thoracic Society (ATS), the Infectious Diseases Society of America (IDSA), and the European Respiratory Society.
The new guidelines provide recommendations for treating multidrug-resistant tuberculosis (MDR TB) and extensively drug-resistant tuberculosis (XDR TB), as well as isoniazid-resistant TB. The recommendations prioritize orally-administered medications to make treatment more tolerable and improve patient outcomes, and provide guidance on the choice and number of drugs to use during treatment. Importantly, the recommendations address treatment of contacts to drug-resistant TB cases to prevent future drug-resistant TB disease. Recommendations also cover treatment length, the role of surgery, practices for treating special populations, and monitoring treatment.
CDC offers resources to help raise awareness of drug-resistant TB, including personal stories of MDR TB survivors like Nauman and Tenzin, infographics, and the latest U.S. drug-resistant TB data.

2019 TB Program Managers’ Course
DTBE hosted the 2019 TB Program Managers’ Course in Atlanta on October 21-24. The TB Program Managers’ Course is designed for TB program managers, nurse consultants, public health advisors, and TB controllers who have program management responsibilities. Participants included 33 TB program managers from state and big city TB programs and 15 observers from DTBE.
Submitted by Carissa Sera-Josef
The National TB Program Objectives and Performance Targets for 2025
In September 2019, the Division of Tuberculosis Elimination released the national TB program objectives and performance targets for 2025. The national objectives include decreasing TB incidence rates for both US-born (0.4 cases per 100,000) and non-US—born populations (8.8 cases per 100,000), as well as for US-born minorities (1.0 case per 100,000) and children less than five years of age (0.1 cases per 100,000). The objectives incorporate key process indicators for patient management, laboratory reporting, contact investigations of infectious TB patients, and follow-up examination of immigrants and refugees who recently arrived in the United States with Class B notifications. The complete list of national objectives and targets can be found via https://www.cdc.gov/tb/programs/evaluation/indicators/default.htm
Indicators for measuring progress toward reaching the national objectives were established by the National TB Indicators Project (NTIP). Data reported to the National TB Surveillance System on the Report of a Verified Case of Tuberculosis (RVCT), the Aggregate Report for Program Evaluation (ARPE), and the Electronic Disease Notification (EDN) system are used in NTIP to calculate the indicators.
The 2025 national performance targets describe the level of success achieved by the top 10% of TB programs in the United State. To determine the targets, we used statistical models to find trends in NTIP data from 2010 through 2018. State and local TB programs with fewer than 150 TB cases from 2016–2018 were excluded. For each indicator, we developed a regression model to estimate the 90th percentile for each year, then used the fitted model to estimate the 90th percentile in the year 2025. The 90th-percentile values reflect the projected performance of the top 10% of TB programs in the United States in 2025.
TB program officials are encouraged to work closely with CDC Project Officers and Evaluation Consultants to conduct evaluation studies and to develop strategies to optimize performance to meet the targets.
Reported by Kai H. Young
Case and Cohort Reviews: What are TB programs doing and how are they doing it?

Systematic review of TB case management activities is a required component of TB cooperative agreement funding. However, the type of review, timing of the review and methods used can differ between TB programs. The developed a survey to better understand how programs were meeting this requirement. The objectives of the survey were to catalogue the different methods being used and to gain information that would improve support for program evaluators and others conducting the reviews.
The survey was developed and administered by the TB PEN Steering Committee. It was distributed via SurveyMonkey to the TB PEN email listserv, which includes over 100 recipients, in July 2019.
Type and Frequency of Reviews
There was a total of 29 responses from 25 different state and city TB programs. All but one respondent reported using a systematic review process or processes for TB case management: 24 (86%) respondents reported conducting case reviews, 23 (82%) reported doing cohort reviews, and 5 (18%) reported doing chart reviews. Of respondents conducting case reviews, 42% conduct them monthly; whereas those who do cohort reviews conduct them quarterly (35%) or twice per year (22%). Chart reviews are conducted monthly (40%) or as needed (60%).
Methods Used to Conduct Reviews
Most respondents (71%) reported initiating reviews at the state level. One respondent commented, “The cohort reviews are initiated by the state. Most of the case reviews are initiated by the local health districts. There are exceptions when the state identifies needs in a district and then initiates a case review.” Most respondents who do case reviews (83%) and cohort reviews (78%) work with the local health jurisdiction to complete the reviews; whereas only 20% of those who do chart reviews reported including the local health jurisdiction. For case reviews, most respondents review only current cases, and 60% of those who do chart reviews use both current and completed cases.
Criteria for Case Selection
Most (79%) respondents for all review types report not using any comorbidities or social/economic criteria for selecting patients to include in a review. Of those who did use such criteria, respondents select patients based on HIV status (14%), experiencing homelessness, drug use, or being a resident or employee of a healthcare facility (11% each). Medical criteria for selecting cases for review include genetic clustering (25%), drug resistant disease (21%), history of prior treatment for TB or LTBI, history of treatment noncompletion, or patient requiring therapeutic drug monitoring (18% each).
For case reviews, most respondents reported not using a defined time period to identify cases for review. This was reversed in respondents who do cohort reviews, with 35% using a defined time period and 4% not using a defined time period. For chart review, 20% of respondents reported using a defined time period compared to 40% not using a defined time period. There was no standard definition of ‘time period’ for selecting cases to include in a review, however, respondents included examples: “Cases counted within a 6-month time frame”, “Cases counted in the current calendar year”, or “All cases and suspects in their 4th month of treatment…”.
Use and Dissemination of Results from Reviews
Most programs (64%) analyze data and information from TB reviews and share it with local health jurisdictions. The same percentage include the information in their annual progress reports to CDC. Only 11% reported disseminating the information beyond the program.
Where do We Go from Here?
The results were presented to the TB PEN community via conference call in October 2019. The TB PEN Steering Committee plans to reach out to programs who expressed a need for support and guidance in conducting reviews. Additionally, the TB PEN Steering Committee may create and lead a TB cohort review workgroup in order to continue to elicit information from programs and create and update review resources. TB cohort and case reviews will also be a topic during the 2020 TB ETN/PEN conference scheduled for September 20-22, 2020.
Submitted by Helen McGuirk and Rachel Yelk Woodruff
Lessons Learned from TB Modeling through the NCHHSTP Epidemiologic and Economic Modeling Agreement
The first 5 years of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention’s epidemiologic and economic modeling cooperative agreement, NEEMA, concluded at the end of September 2019. When asked what they learned from their TB modeling experience, all three grantees determined based on model results that TB elimination is a distant goal using current tools and service provision levels; however, substantial progress can be achieved with extensive scale-up of targeted testing and treatment (TTT) of latent TB infection (LTBI) in non-US-born populations or with great improvements in global TB control.

The University of California’s Consortium for Applied Prevention Economics (CAPE) highlighted model findings that California TB cases could be cut in half by 2024 with a 4-fold increase in TTT of non-US-born residents and of persons with medical risks for progression. In addition, they estimated that full implementation of the US Preventive Services Task Force Recommendations or of the California TB Risk Assessment would also prevent half of projected TB cases in California within the first 10 years (over 9,500 TB cases). Models by each grantee showed that TTT of non-US-born persons would be most effective in making progress towards TB elimination, but that TTT of persons with HIV (e.g., those having the highest progression rates) would be most efficient.
Modelers from Johns Hopkins Bloomberg School of Public Health (JHSPH) emphasized that risk populations and their demographics differ by state, as does TB transmission and reactivation, and consequent cost effectiveness of TTT. Harvard University’s Prevention Policy Modeling Lab (PPML) remarked that comparing TB transmission models produced by each grantee applied to California data helped to enhance understanding of uncertainties around TB trends and the impact of interventions. Close collaboration with DTBE and state TB controllers was invaluable to modeling efforts, according to JHSPH.
NEEMA model results have corroborated CDC’s decision to focus on TTT for TB elimination, extended prior CDC modeling to 50 states and 20 counties, and produced TB case and LTBI prevalence point estimates and prediction intervals by population (including for some co-morbidities) that can assist TB programs in planning for TB elimination. The modeled scenarios produced powerful results and interactive tools by the United States TB community:
- Tabby 1, Harvard PPML US TB projections by scenario: https://ppmltools.org/tabby/
- Tabby 2, Harvard PPML State-level TB projections by scenario: https://ppmltools.org/tabby2/
- JHSPH State-level historical TB rates by risk population: http://www.modeltb.org/tbheteroinc/index.html
- JHSPH TB projections by scenario for CA, FL, NY, TX: http://modeltb.org/fourState/pa10yr.html
While models relied greatly on National TB Surveillance System (NTSS) data to which they were calibrated, additional data to reduce uncertainties are needed on population dynamics, LTBI prevalence and TB incidence progression rates by population, and on costs. DTBE encourages TB programs to publish programmatic experiences to document the impact and cost of activities. DTBE also encourages sharing of model results, specifically those on cost-effectiveness.
A current challenge is how to implement the modeled scenarios. Other key questions are:
- How can we best reach persons at highest risk for TB for targeted testing and treatment? In the context of electronic health records (EHRs), how can we identify populations having the highest risks of progression?
- How can we compare interventions such as better diagnostics and tools/algorithms to rule out TB disease using EHRs?
- How can we predict who will accept or decline LTBI treatment?
- In the United States, what do we need to do to accelerate TB elimination that might differ from other contexts? The United States is a leader in TB elimination efforts and often sets the standards for other countries.
Submitted by Suzanne Marks, MPH, MA
CDC Laboratory Safety Star: Mindy Dunn, PhD, DTBE
Mindy Dunn, PhD, DTBE safety officer, was recently recognized as the October CDC Laboratory Safety Star for her work in developing best practices, training, and tools for implementing and improving safety practices within Laboratory Branch. The CDC Laboratory Safety Star is a monthly effort by the Office of Laboratory Safety (OLSaf) within the Office of Laboratory Science and Safety (OLSS) to recognize CDC scientists who promote laboratory safety and best practices and whose work exemplifies the highest standards of laboratory safety.

Dunn began her position as a safety officer in DTBE in 2017. In this role, Dunn has applied her knowledge and previous experience as a laboratorian and leader to strengthen the safety program in DTBE. In addition to the daily functions of a safety officer, she has developed and implemented laboratory specific hands‐on trainings, begun and piloted a comprehensive biosafety plan for the branch. Her nominator, Jennifer Whitmon, PhD, specifically highlighted how Dunn “is interested in bringing creativity to safety training.”
A prime example of her creativity was showcased during last year’s National Biosafety Month, when Dunn created a Mobile Safety Station to better involve lab personnel in hands-on safety refreshers on hand washing, and proper glove doffing. At first, she had safety games and prizes in her office and asked people to drop by. “No one came,” recalls Dunn. “So I made a cart, put all my stuff on it…pushed it around the hall, and every time someone was in their office, I said, ‘Hey, do you want to play a safety game? I’ve got prizes.’” Taking the safety refreshers directly to staff proved to be an effective way to engage them. The mobile station was a success, and participation increased from 10 percent to 56 percent.
She serves as the 2019 vice‐chair of the DDID Infectious Diseases Safety Committee. Through this position, she hopes to encourage support among officers and wants to address the topic of leadership development in safety as well.
Her positive attitude and fun spin ideas do not make Dunn underestimate the seriousness of safety. She recognizes its importance on both the large and small scale. “We’re working in an important field: people’s health. And we want to keep encouraging people to come into the field, but if it is unsafe, if people end up with illness, that’s going to be discouraging. So, it’s important that the field itself is seen as a safe one. Smaller picture, I care about everyone in my laboratory. I want them to be safe, so I feel strongly about making sure that the people that I know are safe in what they’re doing.”
Improving screening, testing, and treatment for Latent TB Infection (LTBI): Closing the Gaps in the TB Prevention Cascade in Community Health Clinics (CHCs)

More than two-thirds of tuberculosis (TB) cases diagnosed in the United States are among non-U.S.–born persons, and more than 90% of these TB cases are due to reactivation of latent TB infection (LTBI) most likely acquired in their countries of origin. Improved screening, testing, and curative treatment of LTBI among high-risk populations is a critical component of the U.S. TB elimination strategy.
The Tuberculosis Epidemiologic Studies Consortium (TBESC) is a partnership of the Division of Tuberculosis Elimination (DTBE), Centers for Disease Control and Prevention (CDC) with academic institutions and TB control programs in 11 states; its current focus is LTBI prevention, identification, and treatment. To help meet CDC’s TB elimination goals, TBESC initiated a study to identify barriers to LTBI diagnosis and treatment at community health clinics (CHCs), and to inform interventions to overcome them. CHCs are important partners for TB prevention and control; they promote community engagement and reach high-risk communities in medically underserved areas. The study, “Improving screening, testing, and treatment for Latent TB Infection (LTBI): Closing the Gaps in the TB Prevention Cascade in Community Health Clinics,” began data collection in November 2019.
The study will use a mixed methods approach to quantify current levels of LTBI testing and treatment in CHCs and investigate barriers to scale-up of these activities. Consortium members recruited 16 CHCs that serve non-U.S.—born populations, primarily Asian and Hispanic communities. Most clinics serve as safety net clinics for under- and uninsured individuals. Patient chart abstractions will help identify gaps in the LTBI Care Cascade. Provider surveys and in-depth interviews with clinic leadership, providers, and support staff will identify barriers and facilitators for screening, testing, and treatment. The results of this study will help guide the development and implementation of future CHC-based interventions to address LTBI in at-risk communities.
Submitted by Katharine Tatum
Research Initiatives to Improve TB Prevention and Control Efforts
The Clinical Research Branch (CRB) continues to work on several research initiatives to improve TB prevention and control efforts. Study descriptions and updates include the following:
- Study 31: This is the flagship project of DTBE, and the largest active TB treatment trial conducted by CDC to date. Over 2500 participants are enrolled at 34 clinical sites in 13 countries. The study aims to evaluate if high dose (1200 mg) daily rifapentine can shorten the necessary duration of treatment to 4 months, with or without moxifloxacin (rather than ethambutol). Study 31 has been conducted in partnership with NIH’s ACTG trials network, and expects to report results in late 2020. Current activities include completion of follow-up, database cleaning, collating data, preparing for primary data analysis, and designing a dissemination plan.
- Study 32: This is a phase two trial for active TB treatment aiming to optimize the dose of levofloxacin based on pharmacodynamic data. Currently, minimal inhibitory concentrations for all study isolates are being determined at CDC.
- Study 35: This is a pediatric study, for children ages 0-12. Recently there has been a global effort to scale-up use of pediatric preventive therapy, with a special emphasis on 3HP and related short-course rifapentine-based regimens. Study 35 is CDC’s first collaboration in the development of a novel TB drug formulation for young children and aims to assess the safety and pharmacokinetics of new water-dispersible formulations of isoniazid and rifapentine, allowing development of dosing guidelines for children of all ages. The study is being conducted entirely in South Africa. One site has begun enrolling, and two other sites will begin in early 2020.
- Study 37: This is a phase three treatment shortening regimen for LTBI. It compares six-weeks of daily rifapentine to the currently recommended 3-4-month rifamycin containing regimens and is currently enrolling.
Submitted by Carla Jeffries
Lam CK, Fluegge K, Macaraig M, Burzynski J. Cost savings associated with video directly observed therapy for treatment of tuberculosis. Int J Tuberc Lung Dis 2019;23:1149–54.
Langer AJ, Navin TR, Winston CA, LoBue P. Epidemiology of tuberculosis in the United States. Clin Chest Med 2019;40:693–702.
Mase SR, Chorba T. Treatment of drug-resistant tuberculosis [Review]. Clin Chest Med 2019;40:775–95.
Menzies NA, Parriott A, Shrestha S, Dowdy DW, Cohen T, Salomon JA, Marks SM, Hill AN, Winston CA, Asay G, Barry P, Readhead A, Flood J, Kahn JG, Shete PB. Comparative modelling of tuberculosis epidemiology and policy outcomes in California. Am J Respir Crit Care Med 2019. Epub ahead of print.
Nahid P, Mase SR, Migliori GB, Sotgiu G, Bothamley GH, Brozek JL, Cattamanchi A, Cegielski JP, Chen L, Daley CL, Dalton TL, Duarte R, Fregonese F, Horsburgh CR Jr, Ahmad Khan F, Kheir F, Lan Z, Lardizabal A, Lauzardo M, Mangan JM, Marks SM, McKenna L, Menzies D, Mitnick CD, Nilsen DM, Parvez F, Peloquin CA, Raftery A, Schaaf HS, Shah NS, Starke JR, Wilson JW, Wortham JM, Chorba T, Seaworth B. Treatment of drug-resistant tuberculosis. An Official ATS/CDC/ERS/IDSA clinical practice guideline. Am J Respir Crit Care Med 2019;200:e93–142. (Parvez, also with the New York City Department of Health and Mental Hygiene).
To receive the TB Notes Newsletter, enter your email address at the bottom of the TB Notes webpage. If you would like to submit an article or update in TB Notes, please email Annie Rossetti at wuw0@cdc.gov.
You can follow us on Twitter @CDC_TB and Facebook @CDCTB and sign up for email updates through Adobe Campaign.