TB NOTES

TB Notes 42018
Notes from the Director
Dear Colleague:

The Centers for Disease Control and Prevention (CDC) released updated recommendations for the use of once-weekly isoniazid-rifapentine for 12 weeks (3HP) for the treatment of latent tuberculosis (TB) infection. The updated recommendations, published in CDC’s Morbidity and Mortality Weekly Report (MMWR), support expanded use of an effective, shorter, treatment regimen to reach even more people with latent TB infection.
The updated recommendations include the use of 3HP:
- By directly observed therapy or self-administered therapy in persons over 2 years of age,
- In children and adolescents, 2-17 years old, and
- In persons with latent TB infection and HIV/AIDS and taking antiretroviral medications with acceptable drug interactions with rifapentine.
The 3HP regimen can help remove current barriers to initiate and complete latent TB infection treatment. By supporting a shorter treatment timeframe, offering the option for self-administration, and reducing treatment costs, cure of latent TB infection can be improved.

The United States has made great progress towards the goal of TB elimination, but we can increase our prevention efforts to turn TB elimination into a reality. Treatment of latent TB infection is essential to controlling and eliminating TB in the United States because it substantially reduces the risk that latent TB infection will progress to TB disease. Up to 13 million people in the United States have latent TB infection, and without treatment, they are at risk for developing TB disease in the future—but with treatment, this risk is greatly reduced.
Our public health system and private providers play a crucial role in this effort. Clinicians can work with patients to determine the best latent TB infection treatment regimen, prescribe shorter regimens, and provide support and resources to help patients to complete treatment successfully.
We encourage clinicians and public health professionals to review and implement the updated recommendations, which includes guidance on patient education and monitoring. CDC has resources for latent TB infection, including the patient education materials in various languages and the latent TB infection resources hub.
Thank you for your work and continued commitment to turn TB elimination into a reality.
Philip LoBue, MD, FACP, FCCP
Director
Division of Tuberculosis Elimination
National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention
New Team Lead

We are pleased to announce that Allison Maiuri, MPH, CHES, is the new team leader for the Education, Training, and Behavioral Studies Team within the Communications, Education, and Behavioral Studies Branch (CEBSB) in the Division of Tuberculosis Elimination (DTBE).
Allison began her CDC career in DTBE as an Association of Schools of Public Health fellow in 2006 and continued with the division as a CDC employee through 2014. During her time with DTBE, Allison conceptualized, implemented, and evaluated successful training and education resources for diverse audiences. She also applied behavioral and learning theory methodologies to develop effective trainings and educational products. She led the annual TB Program Managers’ Course, a week long, multi-session course and employed Adult Learning Theory when developing course content. She also contributed to the management and oversight of the CDC-funded Regional Training and Medical Consultation Centers.
Since 2014, Allison served as a health communication specialist in CDC’s Division of Viral Diseases. She led the communication efforts to increase awareness about vaccination against measles, mumps, rubella, and polio, while working closely with subject matter experts in epidemiology and laboratory science. She also provided critical communication support to states on measles and mumps outbreaks. In addition, she provided communication support for the STRIVE Ebola vaccine trial in Sierra Leone through two deployments.
Allison recently received the honor of the CDC as well the HHS Secretary’s Employee of the Month and the 2017 National Center for Immunization and Respiratory Diseases’ (NCIRD) Employee of the Year. Allison earned her Master of Public Health from Emory’s Rollins School of Public Health and Bachelor of Science in Psychology from the University of North Carolina at Chapel Hill. Allison loves traveling to new places and learning about other cultures. When at home, her dog, Oliver, keeps her busy with his seemingly boundless energy.
Submitted by Nick DeLuca, PhD, DTBE
TB Education and Training Network (TB ETN) and TB Program Evaluation Network (TB PEN) Conference, Call for Abstracts
The TB Education and Training Network (TB ETN) and the TB Program Evaluation Network (TB PEN) Conference will be held September 18-20, 2018 in Decatur, GA. This joint conference will feature a poster session, giving attendees an opportunity to share and discuss their work.
Appropriate topics for TB ETN posters include activities associated with the systematic health education process, such as needs assessment, development, pilot testing, implementation, and assessing effectiveness. Appropriate topics for TB PEN posters include methods related to systematic program evaluation, such as capacity building, engagement in monitoring and evaluation, sharing lessons learned from evaluation, and using evaluation findings to make systemic changes.
If you have completed or will soon complete an education, training, or program evaluation project that you would like to share, please visit TB ETN PEN Call for Abstracts for an abstract submission form and more information. The deadline for submission is August 3, 2018.
Send your completed abstract submission form to:
- TB ETN abstracts: ssegerlind@cdc.gov
- TB PEN abstracts: ryelkwoodruff@cdc.gov
For further information regarding TB ETN posters, please contact Sarah Segerlind by email at ssegerlind@cdc.gov or by telephone at 404-639-8338.
For further information regarding TB PEN posters, please contact Rachel Yelk Woodruff by email at ryelkwoodruff@cdc.gov or by telephone at 404-639-6018.
TB Education and Training Network (TB ETN), Request for Nominations

The TB Education and Training Network (TB ETN) is currently accepting nominations for two awards:
- Project Excellence Award
- TB Educator of the Year Award
These two awards were established to recognize excellence in TB health education, training, and communication. The awards will be presented during the annual TB ETN conference (September 18-20, 2018) in Decatur, GA. To be considered for recognition, a completed nomination form, along with supporting documentation, must be received by TB ETN no later than August 3, 2018. A person may self-nominate or be nominated by someone else. Submissions will be reviewed by the Division of TB Elimination.
Please see TB ETN Awards for a nomination form and more information regarding award criteria and nomination requirements.
For more information, contact Peri Hopkins at (404) 639-8988/phopkins@cdc.gov or Sarah Segerlind at (404) 639-8338/ ssegerlind@cdc.gov
Submitted by Sarah Segerlind, MPH, DTBE and Peri Hopkins, MPH, DTBE
New York City TB Summit
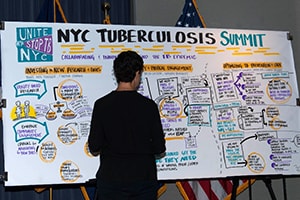
On June 29th, the New York City Department of Health and Mental Hygiene’s first-ever TB Summit gathered 200 policy makers, thought leaders, innovators, TB survivors, and public health experts to kick off strategic efforts towards eliminating TB in New York City (NYC). The NYC TB rate is still more than double the national rate (7.5 vs 2.8 cases per 100,000 persons in 2017).
The Summit theme was “Inform, Engage, and Innovate for TB Elimination.” Expert speakers shared perspectives on TB elimination, the importance of education and advocacy, and sparked discussion on innovations in TB prevention and care. Of 200 participants, 150 stakeholders were in attendance and another 50+ participants joined by webinar; participants represented a diverse range of industries and groups including healthcare, public health, advocacy, pharmaceutical, diagnostic, laboratory, academia, research, and information technology.

Dr. Demetre Daskalakis, Deputy Commissioner for Disease Control with the New York City Department of Health and Mental Hygiene, commenced the Summit by articulating the New York City Health Department’s commitment to TB elimination efforts. The morning plenary, “Bending the Curve: Ending TB in New York City,” featured panelists representing local, state, national, and international organizations. Dr. Joseph Burzynski, Director of the New York City Bureau of Tuberculosis Control, presented the rationale and framework for developing a strategic plan to eliminate TB in New York City and the discussed the importance of key stakeholders working collaboratively and creatively to achieve our vision.” Dr. Margaret Oxtoby, Director of the Bureau of

TB Control for the New York State Department of Health, discussed New York State TB epidemiology and the need for a cohesive and collaborative elimination plan. Dr. Philip LoBue, Director of CDC’s Division of Tuberculosis Elimination, presented the national perspective on TB elimination. Mr. Jose Luis Castro from the International Union Against TB and Lung Disease, and Ms. Jane Coyne, from the Office of the United Nations Special Envoy for TB presented the global TB context and its relevance to New York City. Next, a series of panel discussions addressed three aspects of building a framework for TB elimination in New York City: research and tools, advocacy, and prevention and care.
After lunch, panelists described innovative approaches to TB elimination, highlighting the development of the California TB Elimination strategy, the scaling up of latent TB infection services at a community health center in Massachusetts, and the expansion of Project ECHO in New Mexico.
In breakout groups, participants returned to the questions posed by the elimination framework presentations:
- Based on what is required to further TB testing and treatment, what research do you believe we need?
- What could be done, or what needs to be done, to enhance testing and treatment for TB?
- Based on the resources that TB elimination requires, in what areas should advocacy be focused?

Participants were asked to consider each question in the context of “an ideal world” – that is, one with infinite resources – and to consider what resources or information would be required to proceed with any proposed plans. Several CDC staff including Dr. Sapna Bamrah Morris, Dr. Neha Shah, Dr. Neela Goswami, Dr. Terence Chorba, Chee Kin Lam, Jimmy Keller, and Mark Miner facilitated or participated in the breakout groups. Dr. Nick DeLuca and Dr. Joan Mangan facilitated the report back from the breakout groups. Live graphic recording was used to capture themes and recommendations from the discussions.
The Summit planning team, led by Dr. Farah Parvez, is grateful to everyone who participated. The knowledge and experience shared by attendees, panelists, facilitators, and moderators was critical to ensuring a successful event. The newly-energized Coalition for a TB-Free NYC will use the information shared at the Summit as a starting point to build a citywide elimination action plan, building on new and existing community partnerships. This collective effort will bring us closer to eliminating TB in NYC. Read more about the TB Summit, and learn how you can join the Coalition for a TB-Free New York Cityexternal icon.
Submitted by Shaila Rao Ed.D., MPH; Farah Parvez, MD, MPH; Martha Alexander, MHS, Bureau of Tuberculosis Control New York City Department of Health and Mental Hygiene
TB Emergency Drug Stockpile

The Division of Tuberculosis Elimination (DTBE) recently established a TB Emergency Drug Stockpile (TEDS) that has already been put to the test. Although the stockpile was created to help TB programs weather manufacturer drug shortages, recently release of drugs from the stockpile was needed in two other situations. The first involved providing drugs from the stockpile that were soon expiring to TB programs so that they could be used in treatment before they expired. The second involved providing rifapentine (RPT) to TB programs experiencing interruption in supplies from their distributor.
The TEDS had drugs that were due to expire in a few months and to avoid waste, DTBE made many of those drugs available in the form of Direct Assistance (DA) to programs so that they could be used before expiration. TB programs were informed through DTBE’s Project Officers who provided assistance in submitting their requests. Offering these drugs to programs allowed for greater cost savings for both DTBE and the programs receiving the drugs at no cost. The drugs that were offered were isoniazid (INH) (100 and 300 mg), amikacin injection, and capreomycin injection. DTBE arranged for delivery of 808 bottles of INH, 139 packages of amikacin, and 764 vials of capreomycin to seven TB programs preventing over $139,000 worth of medications going to waste.
In March 2018, DTBE began to receive notification from the field that several programs were unable to order RPT from their distributors. After talking with these programs and with the National Tuberculosis Controllers Association (NTCA), it was confirmed there was a distribution problem with more than one distributor. Though not a manufacturer shortage, the unavailability of RPT from distributors posed a risk for many patients being treated for latent TB infection (LTBI). DTBE decided that as many patients as possible affected by the shortage of RPT would be able to complete treatment. Many of these patients were on a short-course regimen of 3 months of INH and RPT (3HP) for treatment of LTBI. To ensure patients did not miss treatment, DTBE worked with the affected TB programs and the Department of Health and Human Services (HHS) Supply Service Center to expeditiously provide drugs to programs that requested assistance. In some instances, drugs were shipped overnight. Fourteen TB programs requested RPT, one from as far away as the Republic of the Marshall Islands, and one program requested quantities for four different counties in the state. DTBE delivered 884 packages of RPT at a cost of over $57,000, which contributed to the continuity of care for over 530 patients on treatment. Responses from TB programs to these two releases of drugs from the TEDS were overwhelmingly positive, and validated the value of TEDS in supporting TB programs when life-saving TB drugs become unavailable due to manufacturing shortages or other large scale disruption Challenges.
DTBE continues to work collaboratively with HHS, NTCA, the Food and Drug Administration (FDA), the cooperative agreement recipients (state and local programs), and CDC’s Office of Grants Services to ensure that TEDS medications are utilized prior to expiration, and to assist programs so that patients are not without appropriate and adequate medications during times of shortages.
Submitted by Bruce Bradley, MPA, DTBE

After Hurricane Maria, the Puerto Rico Department of Health (PRDOH) Tuberculosis (TB) Laboratory, with the assistance of DTBE, CDC Foundation, CDC’s Emergency Operations Center, and the Association of Public Health Laboratories, began sending samples from patients at high risk for TB disease to CDC. CDC is a triage site for shipment of these specimens to the Georgia, Florida, and Virginia public health laboratories (PHL). To date, over 400 specimens from Puerto Rico have been tested by these PHL. A secure file transfer protocol (FTP) site was implemented to allow Puerto Rico to download daily results from the three PHL, which were then emailed to the island’s submitter hospitals and clinics.
The PRDOH laboratory building is being painted and refurbished for improved laboratory space for reopening and implementing testing. Parts have been replaced on the air conditioning system to allow full functionality. The TB Laboratory has received reagents, culture media, and equipment purchased through the CDC Foundation and has certified negative pressure of the TB isolation room. Laboratory personnel have also been busy preparing reagents and organizing and cleaning the laboratory in preparation for the reopening. The College of American Pathologists (CAP) proficiency test (PT) was used as an internal PT and results were submitted as a verification of PRDOH’s ability to perform TB testing on patient specimens. Once the PRDOH TB Laboratory is ready to perform testing again, all island hospitals, PRDOH clinics, and private laboratories will be notified and performance indicators such as culture positivity, turnaround times, and contamination rates, will be routinely monitored. PRDOH is looking forward to resuming TB testing services on the island in the near future and would like to thank everyone involved in the Hurricane response. PRDOH TB Laboratory is especially grateful for the Florida, Georgia, and Virginia PHL and their assistance after Hurricane Maria.
Hector Rivera Arbolay, DTBE
Clinical Research Branch Updates

Several key staff from the Clinical Research Branch (CRB) attended the Network meeting of the AIDS Clinical Trials Group (ACTG) in Washington DC in June. ACTG is collaborating with the Division of Tuberculosis Elimination (DTBE) and Tuberculosis Trials Consortium (TBTC) in the conduct of Study 31/A5349, which is assessing a 4-month regimen based on high dose daily Rifapentine for treatment of active TB disease. The study is being conducted in over 30 sites across the globe, and has enrolled over 2,150 patients of the target sample of 2,500. The network meeting included presentations on TB diagnostics, on efforts to develop long-acting formulations for TB treatment, on a recent study of TB prevention in pregnant women, and on a planned assessment of treatment for TB meningitis. CRB staff participated in meetings and discussions with ACTG TB Lab leadership and site staff, provided an update on Study 31/A5349 for the participating sites, and conducted individual meetings with staff from 7 involved ACTG clinical sites and with ACTG leadership.
Kia Bryant, Nigel Scott, and Erin Sizemore attended the Drug Information Association annual meeting in Boston, Massachusetts from June 25-28. Each had both an oral and poster presentation. Nigel presented, “Innovations in the Management of Study Drug Inventory through a Web-based System,” Kia presented “Protocol Deviation Reporting and Tracking without a Deviations Case Report Form,” and Erin presented “Incremental Implementation of Risk-Based Monitoring in a Resource-Constrained Environment.” All three presentations focused on operational aspects of TBTC Study 31 / ACTG 5349 implementation at the TBTC Data and Coordinating Center.
Submitted by Barbara DeCausey, MPH, MBA, DTBE
TB Modeling Tool Shows Potential Impact of Improvements in TB Prevention
Through the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention’s cooperative agreement for epidemiologic and economic modeling, NEEMA: Harvard University’s Prevention Policy Modeling Lab in collaboration with the CDC Division of Tuberculosis Elimination developed a web tool for predicting TB trends in the United States: Tabbyexternal icon. This tool can be used to understand the possible trajectory of TB cases, TB deaths, latent TB infection prevalence, and other outcomes for the population overall as well as for specified subpopulations by age and nativity. The tool allows users to pick several scenarios to compare, each describing strengthening of one aspect of TB services in the United States. The tool is based on a recently published modelling study,[1] in which the researchers found that while the United States is unlikely to reach TB elimination before the end of the century without intensification of TB prevention and control activities, improvements in TB services, particularly escalations in latent TB infection treatment, could substantially increase rates of TB decline. More aggressive prevention and treatment (all modeled scenarios together) could reduce TB incidence in 2050 by 77% from 2016 levels.
Submitted by Nick Menzies, Harvard University; Suzanne Marks and Andrew Hill, DTBE
[1] Menzies NA, Cohen T, Hill AN, Yaesoubi R, Galer K, Wolf E, Marks SM, Salomon JA. Prospects for Tuberculosis Elimination in the United States: Results of a Transmission Dynamic Model. American Journal of Epidemiology. 2018. https://www.ncbi.nlm.nih.gov/pubmed/29762657external icon
To receive the TB Notes Newsletter, enter your email address at the bottom of the TB Notes webpage. If you would like to submit an article or update in TB Notes, please email Sloane Bowman at wnv2@cdc.gov.
You can follow us on Twitter @CDC_TB and Facebook @CDCTB and sign up for email updates here.
Cohn DL, El Sadr WM, Abrams DI, Neaton JD, Benator DA, Vernon AA. In memoriam, Fred Gordin, MD, 1951–2018. Clin Infect Dis 2018. Epub ahead of print.
Njie GJ, Bamrah Morris S, Yelk Woodruff R, Moro RN, Vernon AA, Borisov AS. Isoniazid-rifapentine for latent tuberculosis infection: a systematic review and meta-analysis. Am J Prev Med 2018. Epub ahead of print. (Moro, also with the CDC Foundation Research Collaboration).
Stockbridge EL, Miller TL, Carlson EK, Ho C. Predictors of latent tuberculosis infection treatment completion in the US private sector: an analysis of administrative claims data. BMC Public Health 2018;18:662.