Questions and Answers About Tuberculosis
Tuberculosis is preventable and treatable but remains the world’s deadliest infectious-disease killer. Having infectious TB disease means that you can spread TB germs to others. In the last several years the United States has reported the lowest number of TB cases on record, but too many people still suffer from TB. Even with decreasing numbers, TB continues to be a problem. While the number of TB cases in the United States has gone down, TB still has worse effects among racial and ethnic minorities. This is because certain minority groups are more likely to have TB risk factors that can increase the chance of developing the disease.
This booklet answers common questions about TB. Please ask your doctor, nurse, or other health care provider if you have additional questions.
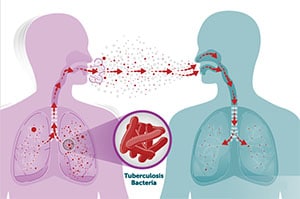
TB is spread through the air from one person to another. The TB germs are spread into the air when a person with infectious TB disease of the lungs or throat coughs, speaks, or sings. People nearby may breathe in these TB germs and become infected.
When a person breathes in TB germs, the TB germs can settle in the lungs and begin to grow. From there, the TB germs can move through the blood to other parts of the body, such as the kidney, spine, or brain.
Anyone can get TB. Some people have a higher risk of getting infected with TB:
- People who have contact with someone who has infectious TB disease
- People who were born in or who frequently travel to countries where TB disease is common, including Mexico, the Philippines, Vietnam, India, China, Haiti, Guatemala, and other countries with high rates of TB
- Health care workers and others who work or live in places at high risk for TB transmission, such as homeless shelters, jails, and nursing homes
In most people who breathe in TB germs and become infected, the body is able to fight the TB germs to stop them from growing. The TB germs become inactive, but they remain alive in the body and can wake up and become active later. This is called latent TB infection, or LTBI for short.
People with LTBI
- Have no symptoms.
- Don’t feel sick.
- Can’t spread TB germs to others.
- Usually have a positive TB blood test or positive skin test reaction.
- May develop TB disease if they do not receive treatment for LTBI.
People with LTBI do not have symptoms, and they cannot spread TB germs to others. However, if latent TB germs become active in the body and multiply, the person will go from having LTBI to being sick with TB disease. For this reason, people with LTBI should be treated to prevent them from developing TB disease. Treatment of LTBI is essential to controlling TB in the United States because it substantially reduces the risk that LTBI will progress to TB disease.
If the immune system can’t stop TB germs from growing, the TB germs begin to multiply in the body and cause TB disease. The TB germs attack the body, and if this occurs in the lungs, the TB germs can create a hole in the lung. Some people develop TB disease soon after becoming infected (within weeks) before their immune system can fight the TB germs. Other people have latent TB infection and may get sick years later, when their immune system becomes weak for another reason. Treating latent TB infection (LTBI) is effective in preventing TB disease.
People with TB disease in the lungs or throat can be infectious, meaning that they can pass TB germs to their family, friends, and others around them. People with TB in other parts of their bodies, such as the kidneys or spine, are usually not infectious.
People with TB disease are most likely to spread it to people they spend time with every day. This includes family members, friends, coworkers, or schoolmates.
People with TB disease need to take several medicines when they start treatment. After taking TB medicine for several weeks, a doctor will be able to tell TB patients when they are no longer able to spread TB germs to others. Most people with TB disease will need to take TB medicine for at least 6 months to be cured.
Many people who have latent TB infection never develop TB disease. While not everyone with LTBI will develop TB disease, about 5–10% will develop TB disease over their lifetimes if not treated. Progression from untreated LTBI to TB disease is estimated to account for approximately 80% of U.S. TB cases. Some people who have LTBI are more likely to develop TB disease than others. People at high risk for developing TB disease generally fall into two categories:
- Those who have been recently infected with TB germs
- Those with medical conditions that weaken the immune system including:
- HIV infection
- Substance use (such as injection drug use)
- Specialized treatment for rheumatoid arthritis or Crohn’s disease
- Organ transplants
- Sever kidney disease
- Head and neck cancer
- Diabetes
- Medical treatments such as corticosteroids
- Silicosis
- Low body weight
Children, especially those under age 5, have a higher risk of developing TB disease once infected.
Symptoms of TB disease depend on where in the body the TB germs are growing. TB disease in the lungs may cause the following symptoms:
- Cough (lasting longer than 3 weeks)
- Coughing up sputum (phlegm from inside the lungs) or blood
- Chest pain
- Fever
- Night Sweats
- Chills
- Loss of appetite
- Weakness or fatigue
- Weight loss
Symptoms of TB disease in other parts of the body may include the following:
- TB of the kidney may cause blood in the urine.
- TB meningitis may cause headache or confusion.
- TB of the spine may cause back pain.
- TB of the larynx may cause hoarseness.
| A Person with Latent TB Infection | A Person with TB Disease |
|---|---|
|
|
|
» a bad cough that lasts 3 weeks or longer
» pain in the chest » coughing up blood or sputum » weakness or fatigue » weight loss » no appetite » chills » fever » sweating at night |
|
|
|
|
|
|
|
|
|
|
You should get tested for TB if:
- You have spent time with a person known or thought to have infectious TB disease.
- You were born in or frequently travel to countries where TB disease is common, including Mexico, the Philippines, Vietnam, India, China, Haiti, and Guatemala, and other countries where TB is common.
- You currently live, used to live, or are employed in a large group setting where TB is more common, such as a homeless shelter, prison, jail, or nursing home.
- You are a health care worker who cares for patients with TB disease.
- You are part of a population that is more likely to have latent TB infection (LTBI) or TB disease, including people who don’t have good access to health care, have lower income, or misuse drugs or alcohol.
In addition, children, especially those under 5, have a higher risk of developing TB disease once infected. Therefore, testing for TB infection in children who may have been exposed to a person with TB disease is important.
There are two types of tests for TB infection: the TB blood test and the TB skin test. Your health care provider should choose which TB test to use. Factors in selecting which test to use include the reason for testing, test availability, and cost. Health care providers are encouraged to use newer TB blood tests to screen for TB infection. Generally, it is not recommended to use both a TB skin test and a TB blood test to test the same person.
TB Blood Tests
TB blood tests use a blood sample to find out if you are infected with TB germs. Two TB blood tests are approved by the U.S. Food and Drug Administration and are available in the United States:
- QuantiFERON®-TB Gold Plus (QFT-Plus)
- T-SPOT®.TB test (T-Spot)
You can get a TB blood test at the health department or at your doctor’s office. The health care provider will draw your blood and send it to a laboratory for analysis and results. If your health department uses a TB blood test, only one visit is required to draw blood for the test.
- A positive TB blood test means that you have been infected with TB germs. Additional tests are necessary to determine whether you have LTBI or TB disease.
- A negative TB blood test means that your blood did not react to the test and that you likely do not have TB infection.
TB blood tests are the recommended TB test for:
- People who have received the bacille Calmette–Guérin (BCG) TB vaccine.
- People who have a difficult time returning for a second appointment to look for a reaction to the TB skin test.
TB Skin Test
The TB skin test may be used to find out if you are infected with TB germs. You can get a skin test at the health department or at your doctor’s office. A health care worker will inject a small amount of testing fluid (called tuberculin or PPD) into the skin on the lower part of your arm. After 2 or 3 days, you must return to have your skin test read by the health care worker. You may have swelling where the tuberculin was injected. The health care worker will measure this swelling and tell you if your reaction to the test is positive or negative.
- Positive skin test: This means the person’s body is infected with TB germs. Additional tests are needed to determine if the person has LTBI or TB disease.
- Negative skin test: This means the person’s body did not react to the test, and that LTBI or TB disease is not likely.
If your exposure to TB germs was recent, your TB skin test reaction may not be positive yet. You may need a second skin test 8 to 10 weeks after the last time you spent time with the person with TB disease. This is because it can take several weeks after infection for your immune system to react to the TB skin test. If your reaction to the second test is negative, you probably do not have TB infection.
If you have a positive reaction to the TB blood test or TB skin test, your doctor or nurse will do other tests to see if you have TB disease. These tests usually include a chest x-ray. They may also include a test of the sputum you cough up. Because TB germs may be found somewhere other than your lungs, your doctor or nurse may check your urine, take tissue samples, or do other tests. Without treatment, LTBI can progress to TB disease. If you have LTBI, you should be treated to prevent developing TB disease. If you have TB disease, you will need to take medicine to treat the disease.
BCG is a vaccine for TB. This vaccine is not widely used in the United States. Many people born outside of the United States have received the BCG TB vaccine.
It is often given to infants and small children in other countries where TB is more common. It protects children in those countries from getting severe forms of TB disease, such as TB meningitis. The BCG TB vaccine is not thought to protect people from getting TB disease in the lungs, which is the most common form of disease in the United States.
In some people, BCG TB vaccine may cause a positive skin test when they are not infected with TB germs. However, there is no way to know if a positive skin test reaction is caused by BCG vaccination or caused by true TB infection. When using the skin test, people who have been vaccinated with BCG and who have a positive skin test reaction should always be further evaluated for TB disease as if they were not vaccinated with BCG.
Unlike the TB skin test, TB blood tests are not affected by prior BCG vaccination. Therefore, TB blood tests are the preferred test for people who have received the BCG vaccine.
Without treatment, latent TB infection (LTBI) can progress to TB disease. If you have LTBI, you should be treated to prevent TB disease even if you do not feel sick. Treatment of LTBI is essential to preventing TB because it substantially reduces the risk that latent TB infection will progress to TB disease.
Treating latent TB infection is effective in preventing TB disease. There are several options for the treatment of LTBI. There have been advances in shortening the length of LTBI treatment from 6–9 months to 3–4 months. Short-course LTBI treatments are effective, are safe, and have higher completion rates than longer treatments.
If you have latent TB infection and you are in one of these high-risk groups, it is even more urgent that you take medicine so you don’t develop TB disease. The following TB medications are used on their own or in combination to treat LTBI:
- Isoniazid (INH)
- Rifapentine (RPT)
- Rifampin (RIF)
CDC and the National Tuberculosis Controllers Association recommend one of the following treatment options for LTBI:
- Three months of once-weekly isoniazid plus rifapentine (3HP)
- Four months of daily rifampin (4R)
- Three months of daily isoniazid plus rifampin (3HR)
If none of the treatment regimens above is an option for you, there are alternative effective LTBI treatment regimens which include 6 or 9 months of isoniazid. When taking isoniazid, your doctor may have you take vitamin B6 with your medication. Your doctor will be able to determine which treatment option is best for your situation. Your treatment may have to be modified if you have had contact with someone whose TB disease is caused by germs that are resistant to isoniazid or rifampin, two of the most important medicines for treating LTBI and TB disease. This means that those medicines can no longer kill the TB germs.
Sometimes people are given treatment for LTBI even if their TB blood test result or TB skin test reaction is negative. This is often done with infants, children, and HIV-infected people who have recently spent time with someone with TB disease. This is because these groups are at very high risk of developing TB disease soon after they become infected with TB germs.
If you start taking treatment for LTBI, you will need to see your doctor or nurse on a regular schedule. It is important that you take all the medicine as prescribed. The doctor or nurse will check on how you are doing.
Most people can take their latent TB infection (LTBI) medicines without any problems; however, sometimes there are side effects. Some side effects are minor problems. For example, the rifampin or rifapentine medicine may cause orange discoloration of body fluids such as urine (pee), saliva, tears, or sweat, and breast milk. Orange discoloration of body fluids is expected and harmless. This is normal and the color may fade over time. The doctor or nurse may advise you not to wear soft contact lenses because they may get permanently stained. If you have any of these side effects, you can continue taking your medicine.
If you have a serious side effect, call your doctor or nurse immediately. You may be told to stop taking your LTBI medicines or to return to the clinic for tests. Serious side effects include:
- Dizziness or lightheadedness
- Loss of appetite
- Flu-like symptoms
- Severe diarrhea or light-colored stools
- Shortness of breath
- Feelings of sadness or depression
- Fever
- Unexplained weight loss
- Brown urine (color of coffee or cola)
- Yellowish skin or eyes
- Rash
- Persistent tingling or prickling sensation of hands and feet
- Persistent tiredness or weakness lasting 3 or more days
- Stomach pain
- Easy bruising or bleeding
- Joint pain
- Nausea
- Vomiting
You should provide a list of current medicines you are taking to your health care provider to avoid drug interactions. Some oral contraceptives (birth control pills) may not work as well when you take them with TB medicines. This is because the TB medicines can sometimes interfere with birth control pills and possibly make the birth control pills less effective. If you are using birth control pills, talk with your doctor before beginning any new medicines. More information on side effects from TB medicine can be found at www.cdc.gov/tb/topic/treatment/adverseevents.htm.
Warning: Drinking alcoholic beverages, such as wine, beer, or liquor, while taking treatment for LTBI or TB disease can be dangerous. Check with your doctor or nurse for more information.
Everyone who has latent TB infection needs to know the symptoms of TB disease. If you develop symptoms of TB disease, you should see a doctor right away.
People sometimes need help managing the LTBI medicine they must take. The CDC has developed LTBI medicine trackers to help patients organize and manage their LTBI medicine. On these medicine trackers, there is space to write treatment schedules, medication intake, and doctor/clinic contact information. There is also a checklist of signs and symptoms that may develop while taking LTBI medicine.
The three medicine trackers include:
- 12-Dose Regimen for Latent TB Infection- Medication Tracker and Symptom Checklist (available in English, Spanish, Tagalog, and Vietnamese languages).
- 4 Months Daily Rifampin (4R) Regimen for Latent TB Infection Medication Tracker and Symptom Checklist (available in English).
- 3 Months of Daily Isoniazid plus Rifampin (3HR) Regimen for Latent TB Infection Medication Tracker and Symptom Checklist (available in English).
To download or print these materials, visit the CDC Patient & General Public Materials Publications & Products.
To learn more about LTBI, visit these CDC webpages:
If you have HIV infection and latent TB infection (LTBI), you need treatment as soon as possible to prevent TB disease. A person with HIV infection who also has untreated LTBI is much more likely to develop TB disease during his or her lifetime than someone without HIV infection. Among people with LTBI, HIV infection is the strongest known risk factor for progressing to TB disease. All people with HIV infection should be tested to find out if they have LTBI and promptly seek treatment if necessary. There are several effective LTBI treatment regimens available for people with HIV.
If you were exposed to someone with TB disease, you may become infected with TB bacteria, but you would not be able to spread the bacteria to others right away. Only people with infectious TB disease can spread TB germs to others. Before you would be able to spread TB germs to others, you would have to breathe in TB germs and become infected. Then the germs would have to multiply in your body and cause infectious TB disease. At this point, you could possibly spread TB germs to others.
In most people who breathe in TB germs and become infected, the body can fight the germs to stop them from growing. The germs become inactive, but they remain alive in the body and can become active later. This is called latent TB infection (LTBI). People with LTBI cannot spread TB germs to others. People who have LTBI can be treated to prevent TB disease.
There is good news for people with TB disease! It can almost always be treated and cured with medicine. But the medicine must be taken as directed by your doctor or nurse.
If you have TB disease, you will need to take several different TB medicines. This is because there are many TB germs to be killed. Taking several TB medicines will do a better job of killing all the TB germs and preventing them from becoming resistant to the medicines. “Resistant” means that the medicine can no longer kill the TB bacteria.
The most common medicines used to treat TB disease are
- Isoniazid (INH)
- Rifampin (RIF)
- Ethambutol (EMB)
- Pyrazinamide (PZA)
If you have TB disease of the lungs or throat, you are probably infectious. You need to stay home from work or school so that you don’t spread TB germs to other people. After taking your medicine for a few weeks, you will feel better and you may no longer be infectious to others. Your doctor or nurse will tell you when you can return to work or school or visit with friends.
Having TB disease should not stop you from leading a normal life. People who are no longer infectious or feeling sick are often able to do the same things they did before they had TB disease. If you take your medicines as directed by your doctor or nurse, they should kill all the TB germs. This will keep you from becoming sick again.
If you are taking medicines for TB disease, you should take them as directed by your doctor or nurse. The TB medicines may cause side effects. Some side effects are minor problems. Others are more serious. If you have a serious side effect, call your doctor or nurse immediately. You may be told to stop taking your TB medicines or to return to the clinic for tests. Serious side effects include:
- Skin rash
- Blurred or changed vision
- Stomach pain
- Brown urine or light-colored stool
- Tiredness
- Fever for 3 or more days
- Flu-like symptoms
- Lack of appetite
- Nausea
- Vomiting
- Yellowish skin or eyes
- Dizziness
- Tingling or numbness around the mouth
- Tingling sensation in the hands and feet
- Stomach upset
- Joint aches
- Easy bruising or bleeding
Some side effects are minor problems. For example, the rifampin may cause orange discoloration of body fluids such as urine (pee), saliva, tears, or sweat, and breast milk. Orange discoloration of body fluids is expected and harmless.
This is normal and the color may fade over time. The doctor or nurse may advise you not to wear soft contact lenses because they may get permanently stained. If you have any of these side effects, you can continue taking your medicine.
Medicine that is prescribed to treat TB disease may interact with other drugs. You should provide a list of current medicines you are taking to your health care provider to avoid drug interactions.
For example, medicine for TB disease can interact with oral contraceptives (birth control pills) and possibly make the birth control pills less effective. If you are using birth control pills, ask your doctor about alternative birth control while you are taking TB medicines. If you are taking methadone (used to treat drug addiction) during TB treatment, you may have withdrawal symptoms. Your doctor or nurse may need to adjust your methadone dosage.
More information on side effects from TB medicine can be found at www.cdc.gov/tb/topic/treatment/adverseevents.htm.
TB germs die very slowly. For the treatment of latent TB infection, it takes at least 3 months (and possibly longer depending on which medications you are on) to kill the TB germs.
For TB disease, it takes even longer and at least 6 months for the medicines to kill all the TB germs. You will probably start feeling well after only a few weeks of treatment, but beware! The TB germs are still alive in your body, even if you feel better. You must continue to take your medicines until all the TB germs are dead, even though you may feel better and have no more symptoms of TB disease.
It can be very dangerous to stop taking your medicines or not to take all your medicines regularly. The TB germs will grow again, and you will remain sick for a longer time. The TB germs may also become resistant to the medicines you are taking. You may need new different medicines to kill the TB germs if the old medicines no longer work. These new medicines must be taken for a longer time and usually have more serious side effects.
If you become infectious again, you could give TB germs to your family, friends, or anyone else who spends time with you. It is very important to take all your medicines as directed by your doctor or nurse.
Sometimes the TB germs are resistant to the medicines used to treat TB disease. This means that the medicine can no longer kill the TB germs.
Multidrug-resistant TB (MDR TB) is caused by TB germs that are resistant to at least two of the most important TB medicines: isoniazid and rifampin.
A more serious form of MDR TB is called extensively drug-resistant TB (XDR TB). XDR TB is a rare type of TB that is resistant to nearly all medicines used to treat TB disease.
If you do not take your medicines as directed by your doctor or nurse, the TB germs may become resistant to certain medicine(s). Also, people who have spent time with someone who is sick with MDR TB or XDR TB can become infected with these multidrug-resistant TB germs.
- Drug resistance is more common in people who
- Have spent time with someone with drug-resistant TB disease.
- Do not take all their medicines as directed by their doctor or nurse.
- Develop TB disease again after having taken TB medicines in the past.
- Come from areas where drug-resistant TB is common.
People with MDR TB or XDR TB must be treated with special medicines. Treatment takes much longer than for regular TB and the medicines may cause more side effects. People with MDR TB or XDR TB are at greater risk of dying from the disease. People with MDR TB or XDR TB must see a TB expert who can closely observe their treatment to make sure it is working.
The best way to remember to take your medicines is to get directly observed therapy (DOT), especially treatment for TB disease. If you get DOT, you will meet with a health care worker every day or several times a week. You will meet at a place you both agree on, or by electronic methods. Meeting in person can be the TB clinic, your home or work, or any other convenient location. You will take your medicines at this place while the health care worker watches. Some TB programs now use electronic methods of DOT for both TB disease and latent TB infection (LTBI). Electronic DOT (eDOT) is an alternative to in-person DOT. If eDOT is available in your area and you qualify for eDOT, a health care worker will watch you take your TB medication remotely over a smartphone or other video-capable electronic device. DOT, whether in-person or using an electronic device, helps you remember to take your medicines and complete your treatment. This means you will get well as soon as possible.
The health care worker will also make sure that the medicines are working as they should. This person will also watch for side effects and answer any questions you have about TB.
Even if you are not getting DOT, you must be checked at different times to make sure everything is going well. You should see your doctor or nurse regularly while you are taking your medicines. This will continue until you are cured.
The only way to get well is to take your medicines exactly as directed by your doctor or nurse. This may not be easy! You will be taking your LTBI medicines for 3 months or longer. If you have TB disease, you will generally be taking medicine for 6 months or longer.
Getting into a routine can help you remember to take your medicines as directed. Here are some ways to help you remember to take your medicine whether you are on LTBI medicine or TB disease medicine:
- Take your pills at the same time every day—for example, you can take them before eating breakfast, during a regular coffee break, or after brushing your teeth.
- Ask a family member or a friend to remind you to take your pills.
- Mark off each day on a calendar as you take your medicine.
- Put your pills in a weekly pill dispenser that you keep by your bed or in your purse or pocket.
- Use a medicine tracker to organize and manage your pills. The CDC website has printable LTBI medicine trackers available. On the LTBI medicine trackers, there is space to write your treatment schedule, number of pills to be taken per week, and doctor/clinic contact information. To download or print the medicine trackers, visit the CDC website www.cdc.gov/tb/education/patient_edmaterials.htm#Treatment.
NOTE: Remember to keep all medicine out of reach of children.
If you forget to take your pills one day, skip that dose and take the next scheduled dose. Tell your doctor or nurse that you missed a dose. You may also call your doctor or nurse for instructions.
The most important way to keep from spreading TB is for people with infectious TB disease to take all medicines exactly as directed by a doctor or nurse. You also need to keep all your clinic appointments! Your doctor or nurse needs to see how you are doing. This often requires another chest x-ray or a test of the phlegm you may cough up. These tests will show whether the medicines are working. They will also show whether you can still give TB germs to others. Be sure to tell the doctor about anything you think is wrong.
If you are sick enough with TB disease to go to a hospital, you may be put in a special room. These rooms use air vents that keep TB germs from spreading to other rooms. People who work in these special rooms must wear a special face mask to protect themselves from TB germs. You must stay in the room so that you will not spread TB germs to other people.
If you are infectious while you are at home, there are things you can do to
- Take your medicines as directed. This is very important!
- Always cover your mouth with a tissue when you cough or laugh. Put the tissue in a closed bag and throw it away.
- Do not go to work or school. Separate yourself from others and avoid close contact with anyone. Sleep in a bedroom away from other family members.
- Air out your room often to the outside of the building (if it is not too cold outside). TB spreads in small closed spaces where air doesn’t move. Put a fan in your window to blow out (exhaust) air that may be filled with TB germs. If you open other windows in the room, the fan also will pull in fresh air. This will reduce the chances that TB germs will stay in the room and infect someone who breathes the air.
Remember, TB is spread through the air. People cannot get infected with TB germs through handshakes, sitting on toilet seats, or sharing dishes and utensils with someone who has TB.
After you take the medicines for about 2 or 3 weeks, you may no longer be able to spread TB germs to others. Your doctor or nurse will tell you when you can return to work or school or visit with friends.
Remember, you will get well only if you take your medicines exactly as directed by your doctor or nurse.
Think about people who may have spent time with you, such as family members, close friends, and coworkers. The local health department may need to test them for TB infection. TB is especially dangerous for children and people infected with HIV. If infected with TB germs, these people need medicine right away to keep from developing TB disease.
For additional information about LTBI and TB disease, please visit www.cdc.gov/tb. Patient materials on LTBI and TB disease are also available in multiple languages at www.cdc.gov/tb/publications/culturalmaterials.htm and https://findtbresources.cdc.gov/.
For information on TB patient support and outreach, visit We Are TB (www.wearetb.com). CDC also highlights the personal experiences of people who were diagnosed and treated for latent TB infection and TB disease, as well as the work of TB control professionals. Visit the CDC TB personal stories page for more information: https://www.cdc.gov/tb/topic/basics/personalstories.htm.