The Rise of Resistant Ringworm: Genomic Sequencing Confirms the First Two Reported U.S. Cases of Trichophyton indotineae
Posted on Monday, September 18, 2023
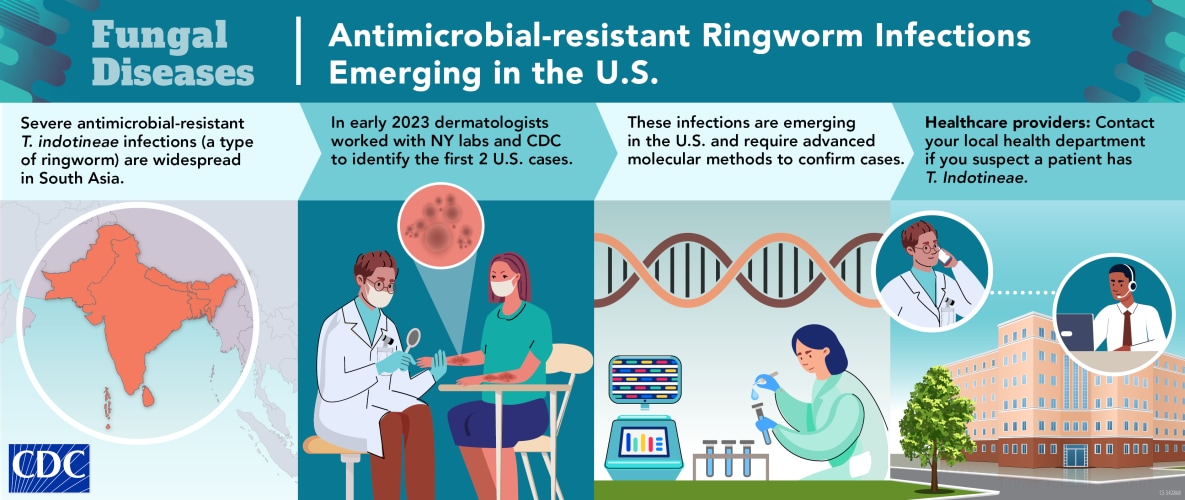
“The more of this we see, the more we know, and the easier it is to recognize,” says Dr. Avrom Caplan of the Department of Dermatology at the NYU Grossman School of Medicine as reflecting on his first encounter with a patient infected with Trichophyton indotineae (T. indotineae). T. indotineae is a highly transmissible, frequently antimicrobial-resistant species of fungus that causes severe ringworm infections. Over the last decade, T. indotineae emerged and spread widely throughout parts of South Asia but had not been reported in the United States until March 2023. That was when Caplan sent isolates from two noteworthy ringworm infections to the Wadsworth Center (New York state public health laboratory). Specialized genomic sequencing identified the isolates as T. indotineae, the first reported cases in the United States.
Not Your Usual Ringworm
Like most dermatologists, Dr. Caplan sees ringworm cases on a regular basis. One of the most common types of fungal skin infections, ringworm is typically considered a mild, though highly contagious, nuisance. Most of the time, ringworm can be treated easily with over-the-counter topical antifungal ointments or prescription oral antifungal medicines.
In January 2023, Dr. Caplan saw a patient in his clinic whose ringworm infection appeared to be different and unusually severe. Instead of the typical small, red, circular rash, the patient had a widespread, inflamed, scaly infection covering their thighs and trunk. The patient seemed to have a travel-associated infection. Symptoms began during a trip to Bangladesh to visit family the previous summer. At that time, several of their family members also developed the skin infection. In Bangladesh, the patient was first treated with topical antifungal and steroid ointments. Their symptoms continued after returning to the United States. Between three emergency room visits and the patient’s first appointment with a dermatologist, the patient was prescribed three additional types of topical antifungals and a full four-week prescription of the first-line antifungal treatment for ringworm. After all the treatments failed without symptom improvement, the patient came to Dr. Caplan’s office.
Putting the Pieces Together
Dr. Caplan began to piece together the unique aspects of this story: the patient’s travel history, severity of infection, and resistance to commonly used antifungals. He began digging into the current literature on ringworm infections. All evidence pointed to an infection with T. indotineae, which had not yet been reported in the United States.
Caplan presented the unusual case to his dermatology residents. The description reminded the residents of a patient that they had treated in December 2021 with similar widespread scaly ring-shaped rashes on their neck, abdomen, and trunk. The patient was first treated with first-line medication for ringworm infections but did not get better. After four weeks of an alternative antifungal, the symptoms subsided. Initial testing at that time indicated that the patient had Trichophyton mentagrophytes, a common species of fungus closely related to T. indotineae. The two fungi are indistinguishable by standard laboratory testing. The clinical team was now questioning that diagnosis. However, this patient had not recently traveled and had no known contact with anyone who had been in the areas with widespread transmission of T. indotineae. If the patient were in fact infected with T. indotineae, it would suggest community transmission within the U.S.
Dr. Caplan remembered a notice from the American Academy of Dermatology and updates to CDC’s website advising clinicians to be on the lookout for severe or potentially antimicrobial-resistant cases of ringworm. He contacted the Mycotic Diseases Branch at CDC. CDC’s mycotic disease experts connected Dr. Caplan with scientists and clinicians in India who had been studying and treating T. indotineae.
Novel Genomic Sequencing Detects an Emerging Fungal Species
New York’s Wadsworth Center, supported by CDC’s Epidemiology and Laboratory Capacity (ELC) program, is one of the few laboratories in the United States that can perform the highly specialized fungal genomic sequencing used to distinguish T. indotineae from T. mentagrophytes. Caplan and his colleagues sent isolates from both patients to the Wadsworth Center, and genomic sequencing confirmed the isolates were T. indotineae.
Next Steps
Between March and September 2023, Dr. Caplan has seen about 10 patients with confirmed or possible T. indotineae infections. Cases have been reported across the United States; the majority associated with international travel to the Indian Subcontinent. It is likely that there are more patients that have not received diagnoses or have been misdiagnosed, which can lead to severe discomfort, continued spread, and unnecessary exposure to ineffective antifungal medications. Most clinicians are not familiar with these infections, and nearly all clinical laboratories would identify the isolates from infected patients as T. mentagrophytes. Dr. Caplan emphasized the importance of building laboratory capacity to allow for detecting and monitoring trends in emerging antimicrobial-resistant ringworm. CDC recognizes the importance of having this testing more widely available and is evaluating best options to provide this support.
Informing Healthcare Providers
“We need to get the word out to dermatologists and need to educate healthcare providers and patients about T. indotineae,” said Dr. Caplan. He also advises primary care, urgent care, and emergency room clinicians that patients with widespread rashes should be referred to dermatologists, especially if they have tried antifungal ointments and/or oral antifungal medications without success. Dermatologists should confirm fungal infections before prescribing treatment and have a clinical suspicion for T. indotineae.
Caplan and clinical, public health, and laboratory colleagues began the type of outreach he is advocating for in a May 2023 publication in CDC’s Morbidity and Mortality Weekly Report (MMWR). Following its release, the report received mainstream media coverage bringing this emerging infection to national attention.
Healthcare providers and dermatologists who suspect a patient has T. indotineae should contact their state or local health departments for assistance. Health departments can contact CDC for assistance with testing by emailing FungalOutbreaks@cdc.gov.