HIV and Men
Data for 2020 should be interpreted with caution due to the impact of the COVID-19 pandemic on access to HIV testing, care-related services, and case surveillance activities in state and local jurisdictions. While 2020 data on HIV diagnoses and prevention and care outcomes are available, we are not updating this web content with data from these reports.
In 2018, mena,b accounted for 30,691 (81%) of the 37,968 new HIV diagnosesc in the United States and dependent areas.d Most (86%) new diagnoses among men were attributed to gay, bisexual, and other men who have sex with men.e,f
The Numbers
HIV Diagnoses



*Based on sex at birth and includes transgender people.
† Includes hemophilia, blood transfusion, perinatal exposure, and risk factors not reported or not identified.
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated). HIV Surveillance Report 2020;31.
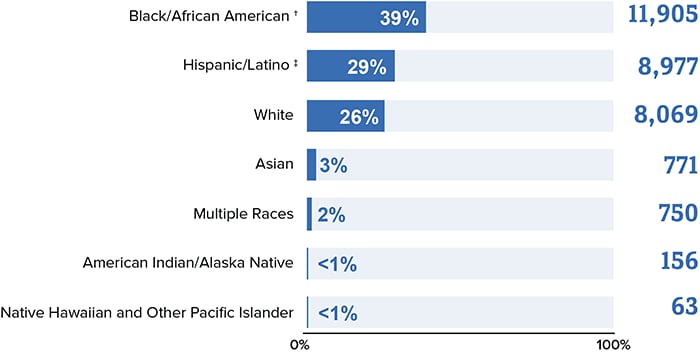
*Based on sex at birth and includes transgender people.
†Black refers to people having origins in any of the Black racial groups of Africa. African American is a term often used for Americans of African descent with ancestry in North America.
‡Hispanics/Latinos can be of any race.
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated). HIV Surveillance Report 2020;31.
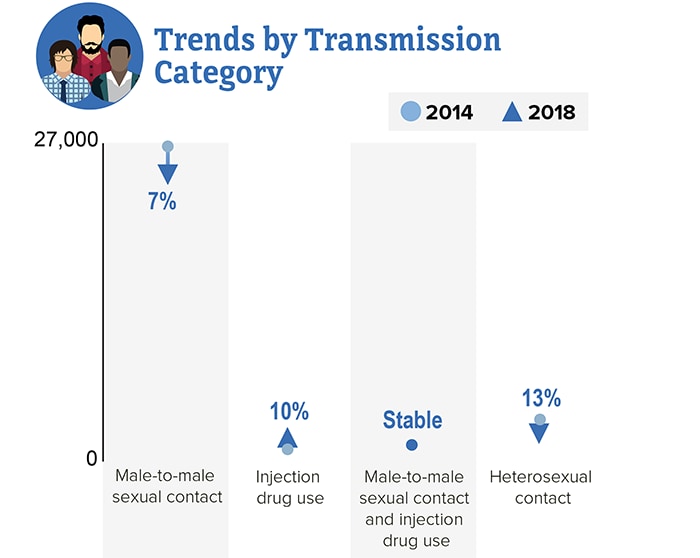
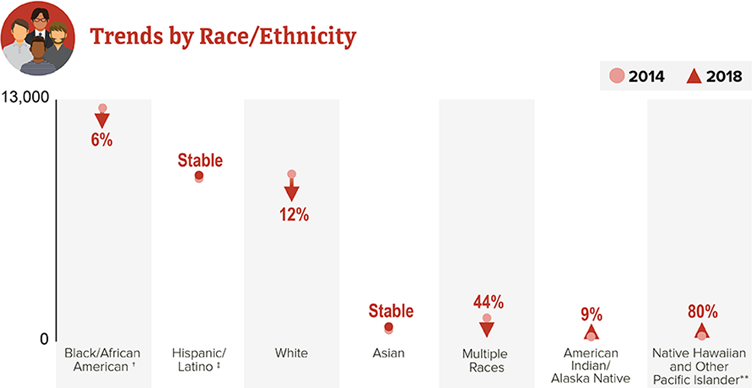
From 2014 to 2018, HIV diagnoses decreased 7% among men overall. But trends varied for different groups of men.

*Based on sex at birth and includes transgender people.
†Black refers to people having origins in any of the Black racial groups of Africa. African American is a term often used for Americans of African descent with ancestry in North America.
‡Hispanics/Latinos can be of any race.
**Changes in subpopulations with fewer HIV diagnoses can lead to a large percentage increase or decrease.
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated). HIV Surveillance Report 2020;31.
Living With HIV



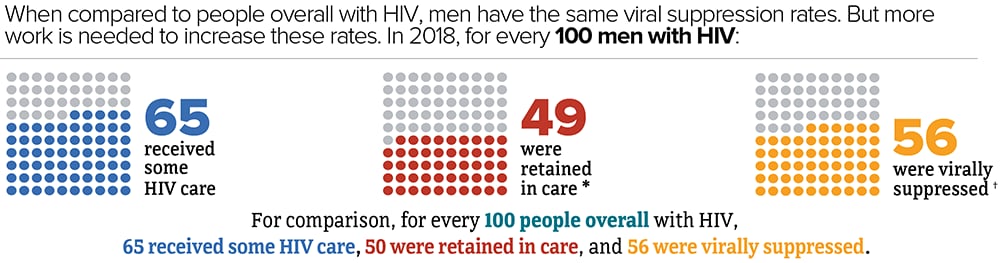
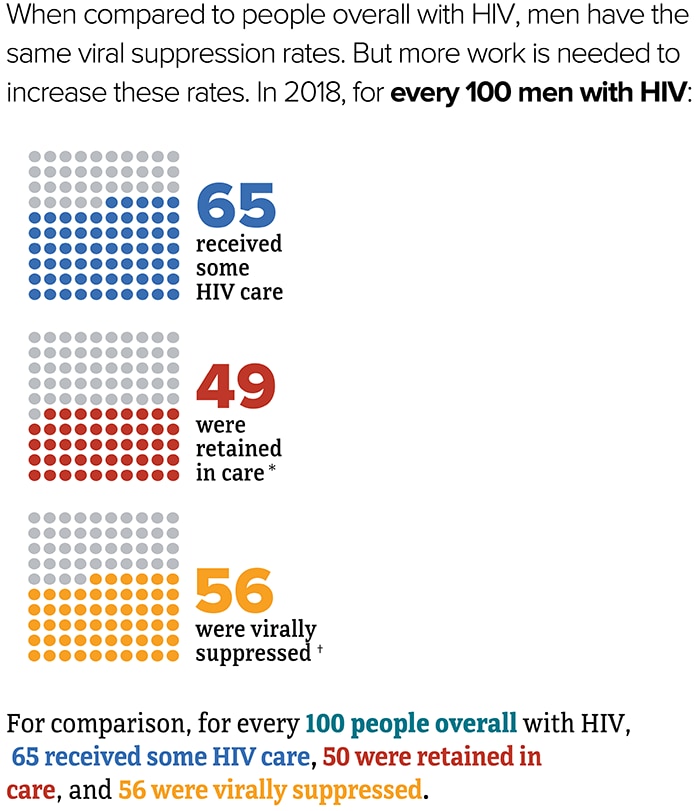
It is important for men to know their HIV status so they can take medicine to treat HIV if they have the virus. Taking HIV medicine every day can make the viral load undetectable. People who get and keep an undetectable viral load (or stay virally suppressed) can live a long and healthy life. They also will not transmit HIV to their sex partners.
*Had 2 viral load or CD4 tests at least 3 months apart in a year.
†Based on most recent viral load test.
Source: CDC. Estimated HIV incidence and prevalence in the United States, 2014–2018 [PDF – 3 MB]. HIV Surveillance Supplemental Report. 2019;25(1).
Source: CDC. Selected national HIV prevention and care outcomes [PDF – 2 MB] (slides).
Deaths
In 2018, there were 11,975 deaths among men with diagnosed HIV in the US and dependent areas. These deaths could be from any cause.
Prevention Challenges
Nearly 1 in 7 men with HIV are unaware they have it. People who do not know they have HIV cannot get the medicine they need to stay healthy and prevent transmitting HIV to their partners. Therefore, they may transmit HIV to others without knowing it.
Most men get HIV through sexual contact, especially anal sex. Anal sex is the riskiest type of sex for getting or transmitting HIV. Receptive anal sex is 13 times as risky for getting HIV as insertive anal sex. Men can also get HIV from having vaginal sex with a woman who has HIV because vaginal fluid and blood can carry HIV. Using condoms or taking medicine to prevent or treat HIV can decrease this risk.
High rates of sexually transmitted diseases (STDs). In 2018, rates of syphilis and gonorrhea were higher among men compared to women. Having other STDs can greatly increase the likelihood of getting or transmitting HIV. Using condoms the right way every time you have sex can protect from some STDs, including HIV.
Injection drug use. Sharing needles, syringes, and other injection drug equipment (for example, cookers) puts people at risk for getting or transmitting HIV. In 2018, men accounted for 73% (2,806) of the 3,864 HIV diagnoses attributed to injection drug usef in the US and dependent areas. People who exchange sex for money or drugs may be at an increased risk for HIV. According to a 2018 National HIV Behavior Surveillance Special Report, [PDF – 317 KB] 23% of men received or gave money or drugs in exchange for sex.
What CDC Is Doing
CDC is pursuing a high-impact HIV prevention approach to maximize the effectiveness of current HIV prevention interventions and strategies. Funding state, territorial, and local health departments and community-based organizations (CBOs) to develop and implement tailored programs is CDC’s largest investment in HIV prevention. This includes longstanding successful programs and new efforts funded through the Ending the HIV Epidemic in the U.S. initiative. In addition to funding health departments and CBOs, CDC is also strengthening the HIV prevention workforce and developing HIV communication resources for consumers and health care providers.
- Under the integrated HIV surveillance and prevention cooperative agreement, CDC awards around $400 million per year to health departments for HIV data collection and prevention efforts. This award directs resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the US.
- In 2019, CDC awarded $12 million to support the development of state and local Ending the HIV Epidemic in the U.S. plans in 57 of the nation’s priority areas. To further enhance capacity building efforts, CDC uses HIV prevention resources to fund the National Alliance of State and Territorial AIDS Directors (NASTAD) $1.5 million per year to support strategic partnerships, community engagement, peer-to-peer technical assistance, and planning efforts.
- In 2020, CDC awarded $109 million to 32 state and local health departments that represent the 57 jurisdictions across the United States prioritized in the Ending the HIV Epidemic in the U.S. This award supports the implementation of state and local Ending the HIV Epidemic in the U.S. plans.
- Under the flagship community-based organization cooperative agreement, CDC awards about $42 million per year to community organizations. This award directs resources to support the delivery of effective HIV prevention strategies to key populations.
- CDC is funding a demonstration project in 4 jurisdictions to identify active HIV transmission networks and implement HIV interventions for Hispanic/Latino gay, bisexual, and other men who have sex with men. Activities include assessing transmission and risk networks, HIV testing, and linking people with HIV to care and treatment.
- In 2017, CDC awarded nearly $11 million per year for five years to 30 CBOs to provide HIV testing to young gay and bisexual men of color and transgender youth of color, with the goal of identifying undiagnosed HIV infections and linking those who have HIV to care and prevention services.
- In 2019, CDC awarded a cooperative agreement to strengthen the capacity and improve the performance of the nation’s HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training, and technical assistance tailored within four geographic regions.
- Through its Let’s Stop HIV Together campaign, CDC offers resources about HIV stigma, testing, prevention, and treatment and care. This campaign is part of the Ending the HIV Epidemic in the U.S. initiative.
a Adult and adolescent men aged 13 and older.
b Based on sex at birth and includes transgender people.
c HIV diagnoses refers to the number of people who received an HIV diagnosis during a given time period, not when the people got HIV infection.
d Unless otherwise noted, the term United States (US) includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
e The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
f Includes infections attributed to male-to-male sexual contact and injection drug use (men who reported both risk factors).
- CDC-INFO 1-800-CDC-INFO (232-4636)
- CDC HIV Website
- Let’s Stop HIV Together
- CDC HIV Risk Reduction Tool
- Find Testing Sites Near You
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated). HIV Surveillance Report 2020;31.
- CDC. Estimated HIV incidence and prevalence in the United States, 2014–2018 [PDF – 3 MB]. HIV Surveillance Supplemental Report 2020;25(1).
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2018. [PDF – 4 MB] HIV Surveillance Supplemental Report 2020;25(2).
- CDC. Selected national HIV prevention and care outcomes [PDF – 2 MB] (slides).
- CDC. Sexually transmitted disease surveillance, 2018.
- CDC. HIV infection risk, prevention, and testing behaviors among persons who inject drugs–national HIV behavioral surveillance: injection drug use – 23 U.S. Cities, 2018 [PDF – 2 MB]. HIV Surveillance Special Report 2020; 24.