HIV and Hispanic/Latino Gay and Bisexual Men: Viral Suppression
Viral suppression is one of the six Ending the HIV Epidemic in the U.S. indicators. Viral suppression refers to the percentage of people with diagnosed HIV who have less than 200 copies of HIV per milliliter of blood.
* Hispanic/Latino people can be of any race.
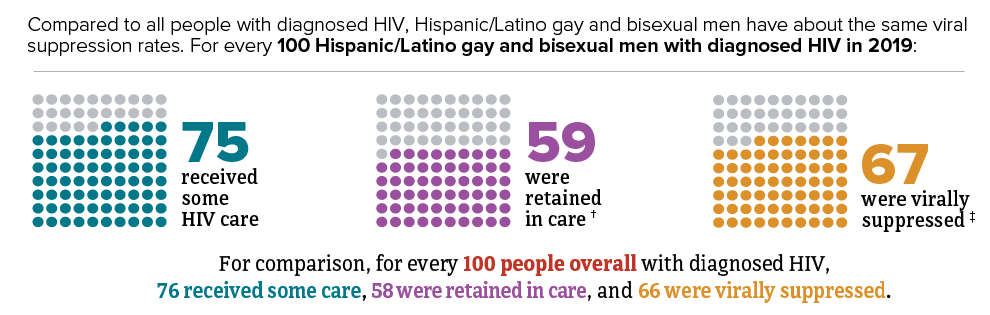
† Had 2 viral load or CD4 tests at least 3 months apart in a year.
‡ Based on most recent viral load test.
Source: CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2019. HIV Surveillance Supplemental Report 2021;26(2).
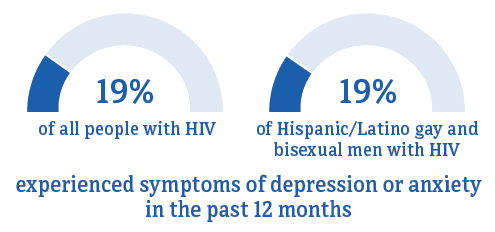
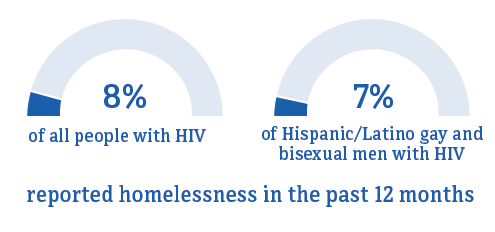
Many people with HIV may experience challenges with achieving and maintaining viral suppression over time. Some of these challenges include missing HIV medical appointments, needing but not receiving other important health care services, or missing doses of HIV treatment.
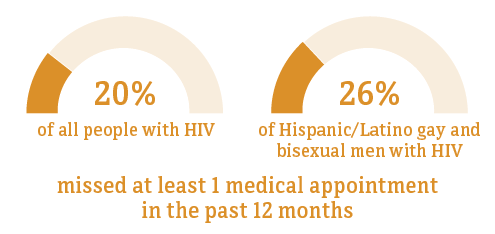
* Hispanic/Latino people can be of any race.
† Among people aged 18 and older.
Source: CDC. Medical Monitoring Project.

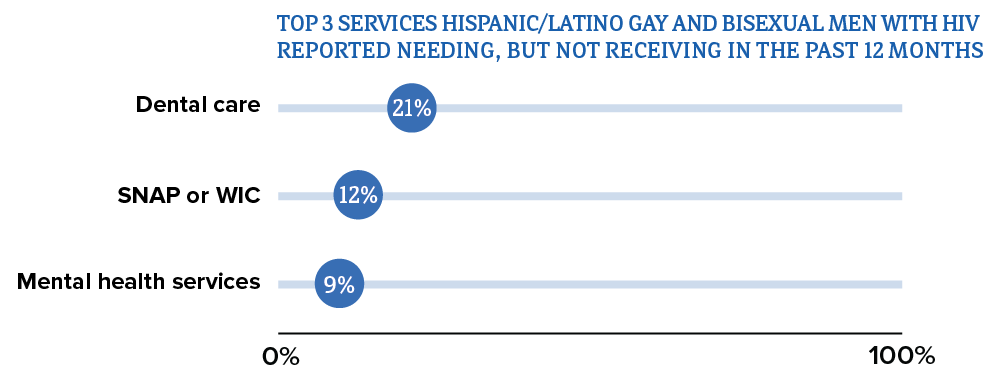

Abbreviations: SNAP = Supplemental Nutrition Assistance Program; WIC = Special Supplemental Nutrition Program for Women, Infants, and Children.
* Hispanic/Latino people can be of any race.
† Among people aged 18 and older.
‡ HIV ancillary services, such as case management and mental health services, are services that support retention in HIV care and viral suppression.
Source: CDC. Medical Monitoring Project.
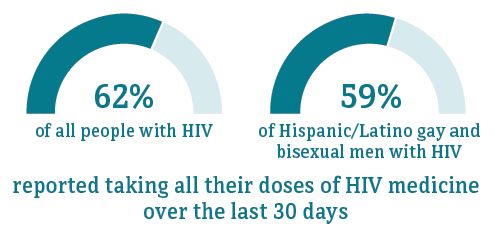
* Hispanic/Latino people can be of any race.
† Among people aged 18 and older.
Source: CDC. Medical Monitoring Project.

* Hispanic/Latino people can be of any race.
† Among people aged 18 and older.
Source: CDC. Medical Monitoring Project.

* Hispanic/Latino people can be of any race.
† Among people aged 18 and older.
Source: CDC. Medical Monitoring Project.
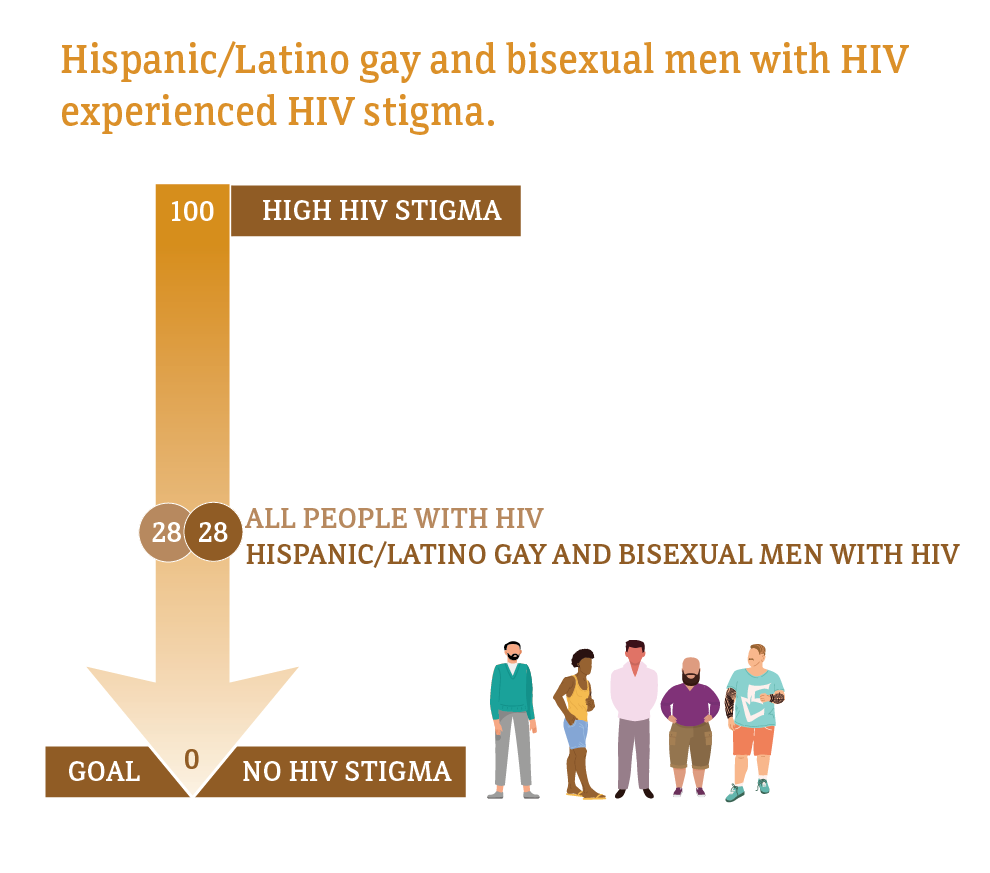
Median HIV stigma scores are presented based on a ten-item scale ranging from 0 (no stigma) to 100 (high stigma) that measures personalized stigma during the past 12 months, current disclosure concerns, current negative self-image, and current perceived public attitudes about people with HIV.
* Hispanic/Latino people can be of any race.
† Among people aged 18 and older.
Source: CDC. Medical Monitoring Project.
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2019. HIV Surveillance Report 2021;32.
- CDC. Estimated HIV incidence and prevalence in the United States, 2015–2019. HIV Surveillance Supplemental Report 2021;26(1).
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2019. HIV Surveillance Supplemental Report 2021;26(2).
- CDC. Barriers to antiretroviral therapy adherence among HIV-positive Hispanic and Latino men who have sex with men—United States, 2015–2019. MMWR 2020;69(40):1437-42.
- CDC. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 23 U.S. cities, 2017. HIV Surveillance Special Report 2019;22.
- CDC. HIV care outcomes among men who have sex with men with diagnosed HIV infection—United States, 2015. MMWR 2017;66(37):969-74.
- Crepaz N, Mullins M, Higa D, Gunn J, Salabarría-Peña Y. A rapid review of disparities in HIV prevention and care outcomes among Hispanic/Latino men who have sex with men in the United States. AIDS Educ Prev 2021; 33(4):276-89. PubMed abstract.
- McCree DH, Walker T, DiNenno E, et al. A programmatic approach to address increasing HIV diagnoses among Hispanic/Latino MSM, 2010-2014. Prev Med 2018;114:64-71. PubMed abstract.
- CDC. Behavioral and clinical characteristics of persons with diagnosed HIV infection—Medical Monitoring Project, United States, 2020 cycle (June 2020–May 2021). HIV Surveillance Special Report 2022;29.