Elimination of Perinatal HIV Acquisition in the United States

In collaboration with national experts and federal partners, the Centers for Disease Control and Prevention (CDC) has developed a framework directed at the goal of eliminating perinatal HIV transmission in the United States. The framework is illustrated in the Figure [the numbers in superscript below refer to the corresponding numbered activities in the figure] and emphasizes consistent use of public health personnel to 1) assure that HIV care includes comprehensive reproductive health, family planning services and prepregnancy (formerly preconception) care and that women of childbearing age are provided HIV testing according to CDC recommendations1; and 2) conduct comprehensive, real-time case finding2 of all pregnant women with HIV and their infants. These two large tasks are conducted under the concept of Perinatal HIV Services Coordination (PHSC). PHSC in each state (or jurisdiction) can assure comprehensive, real-time case finding. It may be helpful to have these functions combined with other related activities, such as the prevention of other perinatally acquired infections. Since many pregnant women with HIV are, in care, it will not be possible—and may not be necessary—for PHSC to actively monitor each woman, once it has been determined that a woman is in care. For women recognized as not in care, finding cases in real time would enable the conduct and coordination of the following components of the perinatal HIV prevention Framework:
- Comprehensive Care (facilitation of comprehensive clinical and psychosocial HIV services for women and infants3; )
- Case Review and Community Action (FIMR-HIV) to identify and address missed prevention opportunities and local systems issues through continuous quality improvement4;
- Research and long-term monitoring to develop and ensure safe and efficacious interventions5; and Data reporting for HIV surveillance and program evaluation6.
Reproductive Health, Family Planning Services and Prepregnancy Care
Increased identification of HIV infection prior to pregnancy, and maintenance of more women in care would result in more opportunities to optimize women’s health prior to and between pregnancies. Proper attention to women’s HIV care inclusive of reproductive health and family planning will support women with their pregnancy as well as pre-pregnancy and postpartum desires.
Comprehensive real-time case finding
Case-finding of women with HIV who are pregnant requires both HIV testing of pregnant women and a mechanism for detecting pregnancy among women with diagnosed HIV.
Comprehensive Care
Clinical management for pregnant women with HIV and their infants is credited with much of the documented reduction in perinatal HIV. Local expertise in clinical care has been nurtured by the support for clinical activities provided by the Health Resources and Services Administration (HRSA), under the Ryan White HIV/AIDS Program. Assuring linkages to these clinical providers is a key function of the PHSC.
Because perinatal HIV transmission is often the result of failures of local health systems, CDC has worked with partners to develop a community-based, continuous quality improvement methodology. This methodology is modeled after the HRSA-funded Fetal-Infant Mortality Review (FIMR) program. The FIMR-HIV Prevention Methodology National Resource Center has training materials available. With consent, FIMR-HIV summarizes the experience from the mother’s perspective through an interview and medical records abstraction. This de-identified information is presented to a multidisciplinary case review team to assess missed prevention opportunities and to develop recommendations for local system improvements. These recommendations are presented to community action teams of locally recognized persons who are in a position to implement the suggested system improvements. Cases of perinatal HIV occur in diverse and ever-changing environments, so utilizing a proven methodology to assess and improve local systems is particularly important. Such systems improvements could also affect other perinatal infections (e.g., hepatitis B, hepatitis C, and syphilis) and maternal and child health services overall.
Research and Long-term Monitoring
The prevention regimens used are evolving and expose thousands of children to antiretroviral (ARV) medications every year. Research to monitor the long-term safety and efficacy of interventions for both women and ARV-exposed children needs a long-term plan and sustained action.
Data Reporting
Accurate data reporting is necessary to direct the activities described above and should include surveillance of infants born to women with HIV “perinatal HIV exposure”.
This framework describes how health care and public health systems may interact to eliminate perinatal HIV in the United States. Considering the multifaceted approach of the Framework, reaching and maintaining elimination requires coordination and active collaboration across multiple agencies at the national, state and local level.
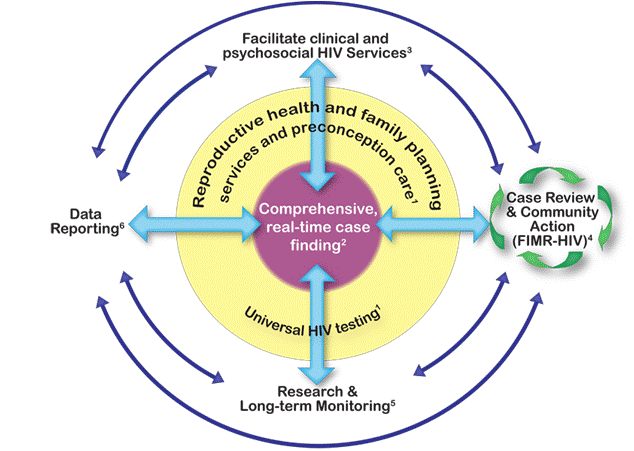
Figure – Framework to Eliminate Perinatal HIV Transmission in the United States
1 Reproductive health and family planning services, prepregnancy care, and universal HIV testing are essential components of perinatal HIV prevention and facilitate
2 comprehensive real-time case finding of all pregnant women with HIV. Real-time case finding enables:
3 comprehensive clinical care and social services for women and infants;
4 detailed review of select cases to identify and address missed prevention opportunities and local systems issues through continuous quality improvement;
5 research and long-term follow-up to develop and ensure safe, efficacious interventions for perinatal HIV prevention;
6 thorough data reporting for HIV surveillance and program evaluation.