Flu and Tdap Vaccination Coverage Among Pregnant Women – United States, April 2021
Summary
Vaccination of pregnant women with influenza (flu) vaccine and tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) can decrease the risk for flu and pertussis (whooping cough) among pregnant women and their infants. The Advisory Committee on Immunization Practices (ACIP) recommends that all women who are or might be pregnant during the flu season receive flu vaccine, which can be administered at any time during pregnancy [1]. ACIP also recommends that women receive Tdap during each pregnancy, preferably during the early part of gestational weeks 27–36 [2, 3]. To assess flu and Tdap vaccination coverage among women pregnant during the 2020–21 flu season, CDC analyzed data from an Internet panel survey conducted during April 2021. Among 1,795 survey respondents who were pregnant anytime during October 2020–January 2021, 54.5% reported receiving flu vaccine before or during their pregnancy. Among 729 respondents who had a live birth by their survey date, 53.5% reported receiving Tdap during pregnancy. Vaccination coverage was highest among women who reported receiving a provider offer or referral for vaccination (flu = 68.1%; Tdap = 69.9%). Racial/ethnic disparities in vaccination coverage among pregnant women persist [4]: Non-Hispanic Black (Black) women had lower flu and Tdap vaccination coverage than non-Hispanic White (White) women; Hispanic women had higher flu vaccination coverage but lower Tdap coverage than White women. Overall, reasons for non-vaccination included concern about safety of flu vaccine and lack of knowledge regarding the need for Tdap during every pregnancy. Provider offers or referrals for vaccination in combination with tailored conversations to educate patients and address their concerns could help increase flu and Tdap vaccination coverage among pregnant women.
Methods
An Internet panel survey was conducted to assess end-of-season flu and Tdap vaccination coverage among women pregnant during the 2020–21 flu season. The survey was conducted during March 31–April 16, 2021, among women aged 18–49 years who reported being pregnant anytime since August 1, 2020, through the date of their survey. Participants were recruited from a large, pre-existing, opt-in Internet panel of the general population operated by Dynata (https://www.dynata.com/) through both Dynata’s GenPop and Dynamix systems. Among 12,571 women who elected to answer the screening questions, 2,522 were eligible, and of these, 2,300 completed the survey (cooperation rate = 91.2%). Data were weighted to reflect the current pregnancy status at the time of interview, age, race/ethnicity, and geographic distribution of the total U.S. population of pregnant women. Analysis of flu vaccination coverage was limited to 1,795 women pregnant anytime during October 2020–January 2021. A woman was considered to have been vaccinated against flu if she reported having received a dose of flu vaccine before or during their most recent pregnancy since July 1, 2020. To accommodate the optimal timing for Tdap vaccination during 27–36 weeks’ gestation, analysis of Tdap coverage was limited to women pregnant anytime since August 1, 2020, who had a live birth by their survey date. A woman was considered to have received Tdap if she reported receiving a dose of Tdap during their most recent pregnancy. Among 857 women with a recent live birth, 128 (14.9%) were excluded because they did not know or would rather not say whether they had ever received Tdap (12.8%) or did not know whether they received it during their pregnancy (2.1%), leaving a final analytic sample of 729; the proportion of pregnant women who received both recommended maternal vaccines (i.e., full vaccination) was assessed among these same 729 women. SAS-callable SUDAAN software (version 11.0.1; RTI International) was used to conduct all analyses. Differences between groups were determined using t-tests with significance set at p<0.05. Increases or decreases noted in this report represent statistically significant differences.
Results
Among women pregnant anytime during October 2020–January 2021, 54.5% reported receiving a dose of flu vaccine since July 1, 2020; Tdap coverage during pregnancy was 53.5% among women with a recent live birth (Table). Receipt of both flu and Tdap vaccines was reported by 30.7% of women with a recent live birth overall, but only among 17.7% of Black women compared with 33.3% of White women. Flu vaccination coverage was lowest among Black women (41.4%), and Tdap coverage was lowest among Black (27.3%) and Hispanic (48.4%) women, compared with White women (flu = 54.2%; Tdap = 60.3%). Flu vaccination was highest among those with an offer or referral (68.1%) compared with those who reported receiving a recommendation but no offer or referral (29.1%) and no recommendation (17.4%). Coverage with Tdap was higher among women with an offer or referral (69.9%) than those with a recommendation but no offer or referral (24.7%); a stable coverage estimate could not be calculated for those without a provider recommendation for Tdap because of the small number vaccinated. In addition, lower flu vaccination coverage was observed among those with less education, who were not working, were living below poverty, living in the South, and were without prenatal insurance, compared with referent groups. Lower Tdap coverage was observed among those living below poverty, living in the South, and with public prenatal insurance.
Overall, a provider offer or referral for flu vaccination during the 2020–21 flu season was reported by 71.6% of respondents pregnant between October and January; 8.5% reported receiving a provider recommendation but no offer or referral, and 20.0% reported not receiving a provider recommendation for flu vaccine.
The proportion of women who reported receipt of a provider offer or referral for influenza vaccination was higher among Hispanic women (79.0%) than among White (68.6%) and Black (69.1%) women. Among Tdap-eligible respondents, 73.8% reported receipt of an offer or referral for Tdap, while 5.8% received a provider recommendation with no offer or referral, and 20.4% did not receive a recommendation for Tdap. Black women (58.2%) were less likely to report receipt of an offer or referral for Tdap than White women (75.0%) and Hispanic women (75.4%).
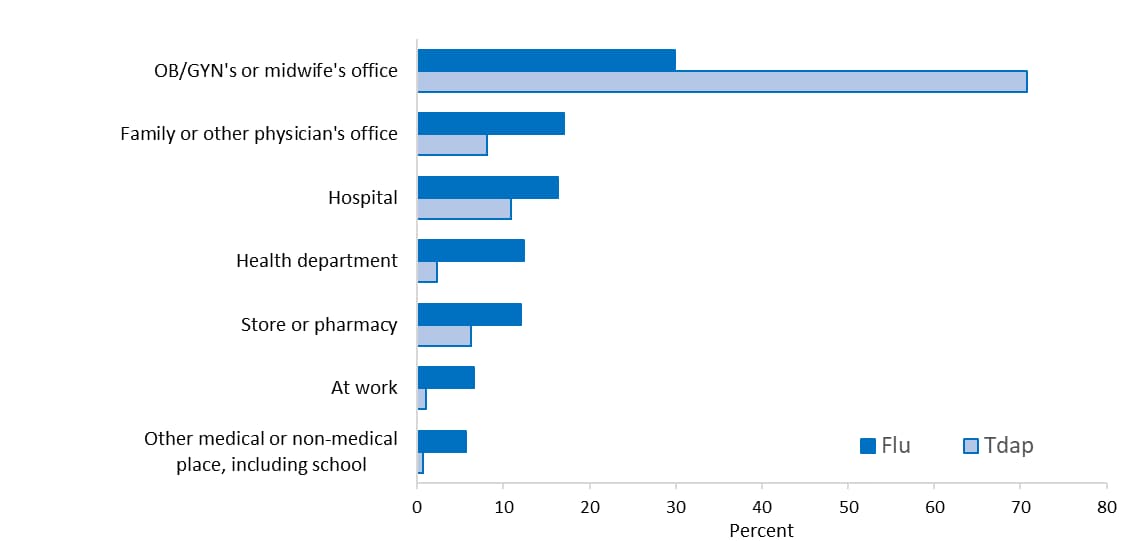
Place of flu vaccination among pregnant women in the 2020–21 flu season was most often the office of an obstetrician/gynecologist (OB/GYN) or midwife (29.9%), followed by family or other physician’s office (17.0%), hospital (16.4%), health department (12.4%), and store or pharmacy (12.0%) (Figure 1). The most commonly reported place of Tdap vaccination among pregnant women with a live birth was an OB/GYN or midwife’s office (70.8%) followed by hospital (10.9%), family or other physician’s office (8.1%), and store or pharmacy (6.3%).
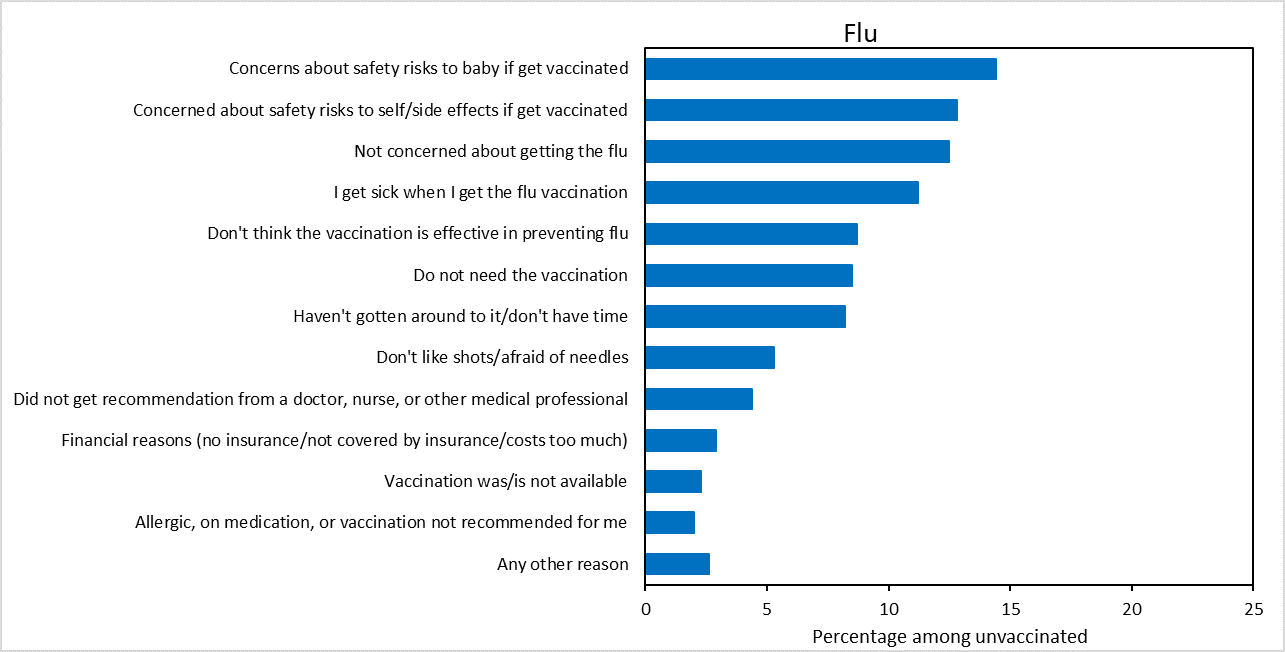
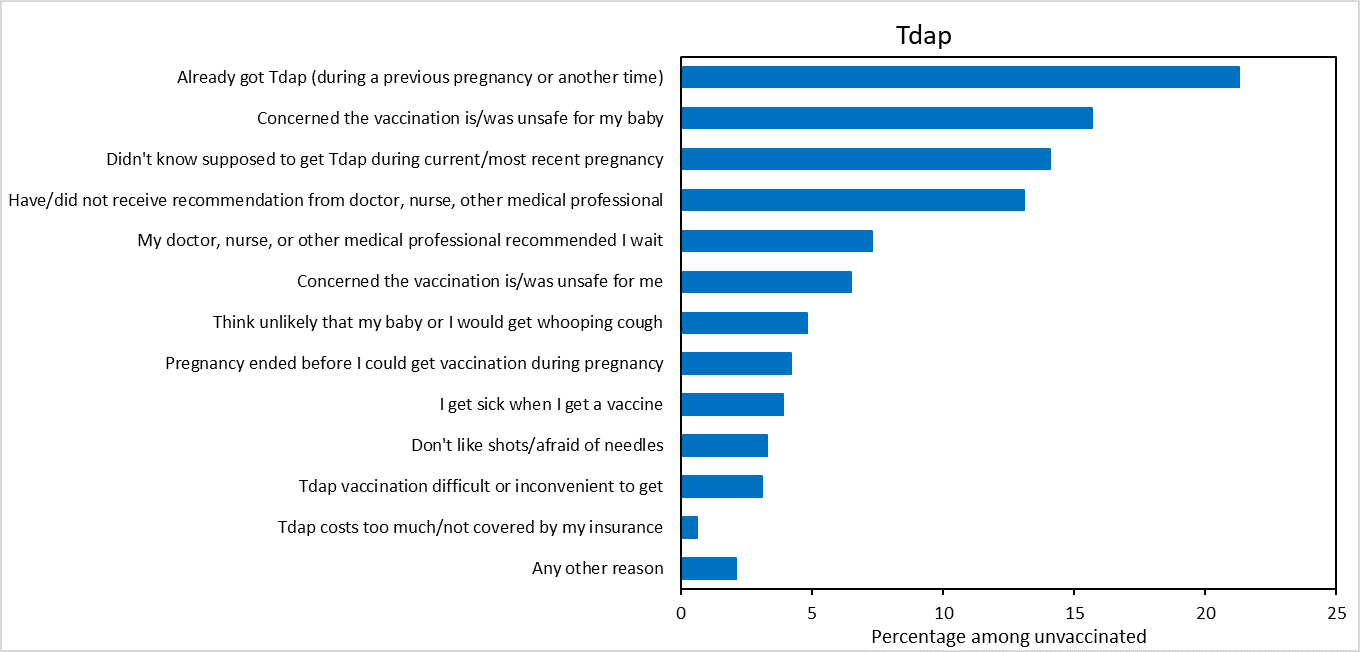
The most frequently reported main reason for not receiving flu vaccination before or during pregnancy was concern about safety (27.2%); 14.4% of unvaccinated women were concerned about the safety of their baby if they were to get vaccinated, and 12.8% were concerned about their own safety and side effects of the vaccine (Figure 2). The most common main reason for not receiving Tdap during pregnancy was a lack of knowledge about the need to be vaccinated during every pregnancy (35.4%): specifically, 21.3% of women who did not receive Tdap during pregnancy reported having been vaccinated with Tdap previously, and 14.1% reported not knowing they were supposed to receive Tdap during their recent pregnancy. The second most common main reason for nonreceipt of Tdap was concern about safety risks to the baby (15.7%).
Discussion
Findings from this survey indicate that approximately 45% of pregnant women did not receive flu or Tdap vaccines, leaving themselves and their infants more vulnerable to flu and whooping cough infection and potentially serious complications including hospitalization and death [5]. Only 30.7% of eligible women received both vaccines recommended during pregnancy. Similar to previous reports, vaccination coverage for both vaccines was highest among pregnant women with a provider offer or referral for vaccination [4]. More than 20% of women indicated not receiving a provider recommendation for vaccination for either flu or Tdap vaccine, suggesting an area for improvement. However, among women who reported receiving a provider offer or referral for flu or Tdap vaccine, nearly one-third of these women remained unvaccinated against flu or whooping cough, suggesting additional need for intervention and improvement among those offered vaccines.
Differences in reported receipt of provider vaccine recommendations might be partly attributable to differences in perception of a provider recommendation between patients and providers. Results from a survey of obstetric care providers conducted by the American College of Obstetricians and Gynecologists (ACOG) suggest that although providers believe they are giving a recommendation for vaccination, the recommendation might not be strong enough to be remembered by patients [6]. Providers are encouraged to follow the Standards for Adult Immunization Practice by assessing vaccination status at every clinical encounter, strongly recommending vaccines that their patients need, administering needed vaccines or referring patients to a vaccination provider, and documenting vaccines administered in the immunization information system (IIS) [7]. CDC has resources to assist providers in effectively communicating the importance of vaccination, such as sharing specific reasons why the recommended vaccines are right for the patient and highlighting positive experiences with vaccines (personally or in their practice) [7]. Another available resource is the ACOG immunization toolkit, which includes communication strategies for providers, as well as extensive information on vaccine financing and coding that could address perceived financial barriers, a commonly reported barrier to stocking vaccines in provider offices [8, 9].
Examination of reasons for non-vaccination provides important insight into what is driving vaccine hesitancy among pregnant women and further highlights the importance of effective provider recommendations for vaccination. Provider awareness of maternal concerns about the safety of both flu and Tdap vaccines during pregnancy, particularly with regard to safety risks to the baby, and lack of knowledge about the recommendation to receive Tdap during every pregnancy can help providers tailor patient communications and education, thus strengthening their recommendations for vaccination. ACIP recommendations for maternal flu and Tdap vaccination are well established, and studies have consistently affirmed the safety and effectiveness of maternal vaccination for women and infants, which providers can share with their pregnant patients [1, 3, 10].
Consistent with prior reports, disparities in maternal vaccination coverage were observed [4]. Flu vaccination coverage was lowest among Black women, and Tdap coverage was lowest among Black and Hispanic women, compared with White women. Factors including knowledge, attitudes and beliefs about vaccines, including mistrust as a result of past medical racism and experimentation, and structural barriers related to accessing vaccines such as not having regular access have been shown to contribute to lower vaccination rates in Black adults generally [11-13]. Previous results have shown that receipt of a provider offer or referral for flu vaccination was similar among Black and White women, but Black women were less likely to report a provider offer or referral for Tdap [4]; results were similar this year. Provider offers or referrals for vaccination, in combination with patient-centered and respectful conversations with patients, could increase vaccination coverage and reduce disparities among pregnant women across racial/ethnic groups [7].
Despite longstanding ACIP recommendations, maternal vaccination with flu and Tdap vaccines is suboptimal, and missed opportunities to vaccinate are common. Findings in this report reinforce the strong association between provider recommendation and offer of or referral for vaccination, and maternal vaccination. During the COVID-19 pandemic, it is more important than ever for pregnant women to receive recommended vaccines, as pregnant women are at increased risk for severe illness not only from flu but also COVID-19 (https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html), and health care resources could become limited as both flu and SARS-CoV-2 (the virus that causes COVID-19) viruses may be circulating simultaneously this fall. In addition, CDC, ACOG, and the Society for Maternal Fetal Medicine recommend COVID-19 vaccination for all people ≥12 years, including pregnant women [14-17]. Providers should take the opportunity to ensure that pregnant women are vaccinated against flu and Tdap when they give a recommendation for COVID-19 vaccine. Vaccination coverage of pregnant women with all recommended vaccines can be increased through implementation of patient education about ACIP vaccination recommendations and safety and benefits of maternal vaccination in combination with evidence-based practices, such as screening patients for recommended vaccinations at every opportunity, reminders to notify providers that their patients need vaccinations, and system-level changes that make vaccinations part of the routine workflow, as well as having a culture of vaccination in the office. [6, 7, 18]. Racial disparities in vaccination coverage could decrease with consistent provider offers or referrals for vaccination, in combination with multicomponent health system and community based interventions [7, 18-20].
Limitations
Interpretation of the results in this report should take into account several limitations of the estimates produced from the Internet panel survey. First, the sample may not be representative of all pregnant women in the United States because the survey was conducted among a smaller group of volunteers who were already enrolled in a preexisting, national, opt-in, general-population Internet panel rather than a randomly selected sample of all pregnant women in the United States. Some bias might remain after weighting adjustments, for example, due to the exclusion of women with no Internet access and/or the self-selection processes for entry into the panel and participation in the survey. Estimates might be biased if the selection processes for entry into the Internet panel and a woman’s decision to participate in this survey were related to receipt of vaccination. Second, we were not able to assess vaccination coverage separately among some racial/ethnic groups such as American Indian/Alaska Native persons, who are less likely to receive recommended vaccinations, due to small sample size [21]. Third, all results are based on self-report and not validated by medical record review; therefore, coverage estimates might be subject to recall or social desirability bias and could be over- or underestimates. However, vaccination coverage estimates from our Internet panel survey have been similar to estimates based on provider-reported data from the Vaccine Safety Datalink (VSD) and the Birth Defects Study [22, 23]. Fourth, although Internet panel surveys of pregnant women have been conducted since the 2010–11 flu season, a change in the computation of the sample weights was introduced for the 2020-21 study and has the potential to affect comparisons to estimates from previous seasons; additional details on this sample weight change are noted below. Fifth, for Tdap, coverage estimates might be subject to uncertainty, given the exclusion of 14.9% of women with unknown Tdap vaccination status. Sensitivity analysis showed that actual Tdap coverage could have ranged from 45.7% to 60.2% in 2021. Finally, formal statistics were used to determine differences in vaccination coverage between groups in this non-probability sample and results should be interpreted with caution [24]. Despite these limitations, Internet panel surveys are considered a useful assessment tool for timely evaluation of flu and Tdap vaccination coverage among pregnant women.
To further minimize bias in estimates derived from the nonprobability panel data, a change in the weighting methodology was employed beginning with the 2020–21 survey. As in previous iterations of this study, sample weights for the 2020–21 survey were created so that the distribution of the weighted sample matched population control totals by region, age group, race/ethnicity and age group by race/ethnicity. Beginning with the 2020–21 survey, the sample weights were constructed to additionally match population control totals by current pregnancy status at the time of the survey as well as all two-way interactions between region, age group, race/ethnicity and current pregnancy status. Control totals were derived by combining data from multiple sources [25-28]. Supplement Table [XLS – 21 KB] shows the effect of the new weighting methodology when applied to data from the 2019–20 study. The new weighting methodology has a minimal effect for most of the characteristics displayed in this table. Overall, 2020–21 estimates for flu and Tdap vaccination coverage were similar to 2019–20 estimates when the same weighting methodology was used in both surveys.
Authors
Katherine E. Kahn, MPH1,2; Hilda Razzaghi, PhD2; Tara C. Jatlaoui, MD2; Amy Parker Fiebelkorn, MSN, MPH2; Tami H. Skoff, MS3; Ada Dieke, DrPH4; Jazmin Duque, MPH5; Michael Witt, MA5; Carla L. Black, PhD2
1Leidos, Inc., Atlanta, GA; 2Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC; 3Division of Bacterial Disease, National Center for Immunization and Respiratory Diseases; 4 Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC; 5Abt Associates, Inc., Atlanta, GA
| Table. Flu* and Tdap† Vaccination Coverage* among Pregnant Women, by Selected Characteristics — Internet Panel Survey, United States, April 2021 | ||||||
| Characteristic | Flu | Tdap | Both vaccines (full vaccination) | |||
| N (weighted %) | Vaccinated, weighted % (95% CI)‡ |
N (weighted %) | Vaccinated, weighted % (95% CI) |
N (weighted %) | Vaccinated, weighted % (95% CI) |
|
| Overall | 1795(100.0) | 54.5(50.8–58.2) | 729(100.0) | 53.5(49.5–57.4) | 729(100.0) | 30.7(27.0–34.5) |
| Age group (years) | ||||||
| 18–24 | 560(23.0) | 49.0(42.6–55.5) | 175(20.9) | 42.7(34.9–50.8) | 175(20.9) | 24.5(18.0–31.9) |
| 25–34 | 779(56.8) | 55.6(50.3–60.8) | 374(60.9) | 58.5(53.1–63.7) | 374(60.9) | 32.5(27.6–37.8) |
| 35–49 (Ref) | 456(20.2) | 57.8(48.4–66.9) | 180(18.3) | 49.2(40.3–58.2) | 180(18.3) | 31.5(23.5–40.4) |
| Race/ethnicity§ | ||||||
| White, non-Hispanic (Ref) | 788(48.9) | 54.2(49.4–59.0) | 431(52.4) | 60.3(55.3–65.2) | 431(52.4) | 33.3(28.7–38.3) |
| Black, non-Hispanic | 298(18.1) | 41.4(31.7–51.6)|| | 81(14.4) | 27.3(17.0–39.9)|| | 81(14.4) | 17.7(9.3–29.2)|| |
| Hispanic | 550(22.5) | 62.6(55.7–69.1)|| | 141(23.4) | 48.4(39.1–57.6)|| | 141(23.4) | 25.0(17.5–33.8) |
| Other, non-Hispanic | 157(10.5) | —¶ | 75(9.7) | 67.4(53.1–79.6) | 75(9.7) | 48.4(34.3–62.8)|| |
| Education | ||||||
| High school degree or less | 456(23.7) | 49.3(42.4–56.1)|| | 176(23.9) | 45.5(37.6–53.6) | 176(23.9) | 23.0(16.7–30.4) |
| Some college, no degree | 267(16.8) | 41.1(31.3–51.3)|| | 163(24.5) | 58.3(49.7–66.6) | 163(24.5) | 30.2(22.6–38.7) |
| College degree | 682(38.6) | 59.1(53.0–64.9) | 261(36.2) | 56.0(49.1–62.7) | 261(36.2) | 35.4(29.1–42.1) |
| Greater than college degree (Ref) | 388(20.9) | 62.6(54.0–70.7) | 129(15.4) | 52.3(42.2–62.3) | 129(15.4) | 32.2(23.3–42.2) |
| Employment status | ||||||
| Working (Ref) | 1130(61.9) | 61.7(56.6–66.6) | 374(49.7) | 50.7(45.1–56.3) | 374(49.7) | 32.5(27.3–38.1) |
| Not working | 663(38.1) | 43.0(37.7–48.4)|| | 354(50.3) | 56.5(50.6–62.1) | 354(50.3) | 28.9(23.9–34.4) |
| Poverty status** | ||||||
| At or above poverty (Ref) | 1413(77.4) | 57.9(53.6–62.1) | 560(75.8) | 55.8(51.2–60.3) | 560(75.8) | 32.4(28.2–36.9) |
| Below poverty | 361(22.6) | 43.1(34.5–52.1)|| | 167(24.2) | 45.9(37.6–54.4)|| | 167(24.2) | 24.7(17.8–32.6) |
| Area of residence†† | ||||||
| Rural | 225(13.7) | 53.5(44.1–62.8) | 113(16.0) | 54.5(44.2–64.5) | 113(16.0) | 31.5(22.7–41.3) |
| Non-rural (Ref) | 1570(86.3) | 54.7(50.6–58.7) | 616(84.0) | 53.3(48.9–57.6) | 616(84.0) | 30.5(26.5–34.7) |
| Region‡‡ | ||||||
| Northeast (Ref) | 366(15.8) | 63.2(55.7–70.2) | 137(17.0) | 57.5(47.8–66.7) | 137(17.0) | 33.0(24.6–42.4) |
| Midwest | 332(19.9) | 56.5(47.8–64.8) | 149(19.7) | 60.1(51.3–68.5) | 149(19.7) | 40.8(32.4–49.7) |
| South | 732(40.9) | 47.3(41.5–53.3)|| | 292(38.6) | 44.0(37.8–50.3)|| | 292(38.6) | 21.6(16.7–27.0)|| |
| West | 365(23.4) | 59.6(51.4–67.4) | 151(24.6) | 60.4(51.3–69.0) | 151(24.6) | 35.2(26.6–44.5) |
| Prenatal insurance coverage§§ | ||||||
| Private/military insurance only (Ref) | 820(46.0) | 58.7(52.8–64.3) | 372(48.8) | 60.6(54.9–66.0) | 372(48.8) | 35.9(30.6–41.4) |
| Any public insurance | 875(48.5) | 53.2(47.8–58.5) | 321(46.4) | 48.6(42.5–54.7)|| | 321(46.4) | 26.4(21.2–32.2)|| |
| No insurance | 99(5.5) | 32.0(19.7–46.4)|| | 36(4.8) | —¶ | 36(4.8) | —¶ |
| Provider vaccination recommendation/offer|||| | ||||||
| Offered or referred (Ref) | 1364(71.6) | 68.1(64.2–71.8) | 531(73.8) | 69.9(65.4–74.1) | 430(59.9)¶¶ | 46.6(41.3–51.9) |
| Recommended, no offer or referral | 111(8.5) | 29.1(17.6–43.0)|| | 46(5.8) | 24.7(12.1–41.4)|| | 236(32.0)*** | 8.7(5.3–13.2)|| |
| No recommendation | 313(20.0) | 17.4(11.4–24.9)|| | 152(20.4) | —¶ | 63(8.1)††† | 0.0(0.0–5.7)|| |
| No. of provider visits since July 1st | ||||||
| None | 7(0.2) | —¶ | N/A | N/A | N/A | N/A |
| 1–5 | 322(21.2) | 47.4(37.2–57.7) | N/A | N/A | N/A | N/A |
| 6–10 | 649(34.4) | 56.8(51.0–62.5) | N/A | N/A | N/A | N/A |
| >10 (Ref) | 817(44.1) | 56.5(51.2–61.6) | N/A | N/A | N/A | N/A |
| High-risk condition for influenza‡‡‡ | ||||||
| Yes (Ref) | 614(34.7) | 59.2(51.9–66.2) | N/A | N/A | N/A | N/A |
| No | 1149(65.3) | 51.8(47.3–56.4) | N/A | N/A | N/A | N/A |
| * Respondents pregnant anytime during October 2020–January 2021 were included in the analyses to assess influenza vaccination coverage for the 2020–21 season. Women who reported receiving a flu vaccination since July 1, 2020, before or during their pregnancy, were considered vaccinated. | ||||||
| † Respondents pregnant since August 1, 2020 and had recently delivered a live birth were included in the analyses to assess Tdap coverage. Women who reported receiving a dose of Tdap vaccine during their pregnancy were considered vaccinated. | ||||||
| ‡ Korn-Graubard 95% confidence interval. | ||||||
| § Race/ethnicity was self-reported. Respondents identified as Hispanic might be of any race. The “Other” race category included Asians, American Indians/Alaska Natives, Native Hawaiians or other Pacific Islanders, and women who selected “other” or multiple races. | ||||||
| || Statistically significant difference compared with referent group | ||||||
| ¶ Estimates do not meet the NCHS standards of reliability. https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf | ||||||
| ** Poverty status was defined based on the reported number of persons living in the household and annual household income, according to U.S. Census poverty thresholds. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html | ||||||
| †† Rurality was defined using ZIP codes where >50% of the population resides in a nonmetropolitan county, a rural U.S. Census tract, or both, according to the Health Resources and Services Administration’s definition of rural population. https://www.hrsa.gov/rural-health/about-us/definition/index.html | ||||||
| ‡‡ Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin. South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming. | ||||||
| §§ Respondents pregnant on their survey date were asked what medical insurance or medical care coverage they had; respondents who had already delivered were asked what they had during their most recent pregnancy. Women considered to have public insurance selected at least one of the following: Medicaid, Medicare, state-sponsored medical plan, or other government plan. Respondents considered to have private/military insurance selected private medical insurance and/or military medical care and did not select any type of public insurance. | ||||||
| |||| Excluded women who did not report having a provider visit since July 2020 (n=7). | ||||||
| ¶¶ Received provider offer/referral for both flu and Tdap vaccines. | ||||||
| *** Received a combination of provider offer/referral, recommendation with no referral, or no recommendation for flu or Tdap vaccines that does not include receipt of offer/referral for both vaccines or no recommendation received for both vaccines. For example, the respondent might have received an offer/referral for flu vaccine and a recommendation with no referral for Tdap. | ||||||
| ††† Did not receive a provider recommendation for flu or Tdap vaccine. | ||||||
| ‡‡‡ Conditions other than pregnancy associated with increased risk for serious medical complications of flu include chronic asthma, a lung condition other than asthma, a heart condition, diabetes, a kidney condition, a liver condition, obesity, or a weakened immune system caused by a chronic illness or by medicines taken for a chronic illness. Women who were missing information were excluded from analysis (n=32). | ||||||
References
- Grohskopf, L.A., et al., Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices, United States, 2021–22 Influenza Season. MMWR Recomm Rep, 2021. 70(No. RR-5): p. 1–28.
- Havers, F.P., et al., Use of Tetanus Toxoid, Reduced Diphtheria Toxoid, and Acellular Pertussis Vaccines: Updated Recommendations of the Advisory Committee on Immunization Practices – United States, 2019. MMWR Morb Mortal Wkly Rep, 2020. 69(3): p. 77-83.
- Liang, J.L., et al., Prevention of Pertussis, Tetanus, and Diphtheria with Vaccines in the United States: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep, 2018. 67(2): p. 1-44.
- Razzaghi, H., et al., Influenza and Tdap Vaccination Coverage Among Pregnant Women – United States, April 2020. MMWR Morb Mortal Wkly Rep, 2020. 69(39): p. 1391-1397.
- Lindley, M.C., et al., Vital Signs: Burden and Prevention of Influenza and Pertussis Among Pregnant Women and Infants – United States. MMWR Morb Mortal Wkly Rep, 2019. 68(40): p. 885-892.
- Mazzoni, S.E., et al., Effect of a multi-modal intervention on immunization rates in obstetrics and gynecology clinics. Am J Obstet Gynecol, 2016. 214(5): p. 617.e1-7.
- Orenstein WA, G.B., Beigi RH, et al., Recommendations from the National Vaccine Advisory committee: standards for adult immunization practice. Public Health Rep, 2014. 129(2): p. 115-23.
- ACOG. Immunization for Women, Physician Tools. 2021 [cited 08/23/2021]; Available from: https://www.acog.org/programs/immunization-for-women/physician-tools?utm_source=redirect&utm_medium=web&utm_campaign=int.
- O’Leary, S.T., et al., Immunization Practices of U.S. Obstetrician/Gynecologists for Pregnant Patients. Am J Prev Med, 2018. 54(2): p. 205-213.
- Nunes, M.C. and S.A. Madhi, Influenza vaccination during pregnancy for prevention of influenza confirmed illness in the infants: A systematic review and meta-analysis. Hum Vaccin Immunother, 2018. 14(3): p. 758-766.
- Brewer, L.I., et al., Structural inequities in seasonal influenza vaccination rates. BMC Public Health, 2021. 21(1): p. 1166.
- Lu, P.J., et al., Trends in racial/ethnic disparities in influenza vaccination coverage among adults during the 2007-08 through 2011-12 seasons. Am J Infect Control, 2014. 42(7): p. 763-9.
- Uscher-Pines, L., J. Maurer, and K.M. Harris, Racial and Ethnic Disparities in Uptake and Location of Vaccination for 2009-H1N1 and Seasonal Influenza. American Journal of Public Health, 2011. 101(7): p. 1252-1255.
- ACOG. COVID-19 Vaccination Considerations for Obstetric–Gynecologic Care. 2021 [cited 08/23/2021]; Available from: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetric-gynecologic-care.
- CDC. Interim Clinical Considerations for Use of COVID-19 Vaccines Currently Authorized in the United States. 2021 [cited 08/23/2021]; Available from: https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fvaccines%2Fcovid-19%2Finfo-by-product%2Fclinical-considerations.html.
- CDC. COVID-19 vaccines while pregnant or breastfeeding. 2021 [cited 08/23/2021; Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy.html.
- Society for Maternal Fetal Medicine COVID-19 vaccination if you are pregnant or breastfeeding. 2021 [cited 08/23/2021].
- Community Preventive Services Task Force. The Community Guide. 2016 [cited 08/23/2021]; Available from: https://www.thecommunityguide.org/topic/vaccination.
- Galea, S., S. Sisco, and D. Vlahov, Reducing disparities in vaccination rates between different racial/ethnic and socioeconomic groups: the potential of community-based multilevel interventions. J Ambul Care Manage, 2005. 28(1): p. 49-59.
- Jarrett, C., et al., Strategies for addressing vaccine hesitancy – A systematic review. Vaccine, 2015. 33(34): p. 4180-90.
- Office of Minority Health. Immunizations and American Indians/Alaska Natives. 2020 [cited 09/28/2021]; Available from: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlID=37.
- Kerr, S., et al., Tdap Vaccination Coverage During Pregnancy – Selected Sites, United States, 2006-2015. MMWR Morb Mortal Wkly Rep, 2017. 66(41): p. 1105-1108.
- Kharbanda, E.O., et al., Maternal Tdap vaccination: Coverage and acute safety outcomes in the vaccine safety datalink, 2007-2013. Vaccine, 2016. 34(7): p. 968-73.
- APORR, AAPOR Guidance on Reporting Precision for Nonprobability Samples. 2015.
- CDC. Natality public-use data on CDC WONDER Online Database, for years 2016-2019 (expanded). 2020; Available from: https://wonder.cdc.gov/controller/saved/D149/D147F671.
- Jatlaoui, T.C., et al., Abortion Surveillance – United States, 2016. MMWR Surveill Summ, 2019. 68(11): p. 1-41.
- Joseph, B.T. and S. Ghumman. Miscarriage Rates By Week And Age: Risks And Statistics. 2021 [cited 8/27/2021]; Available from: https://www.momjunction.com/articles/miscarriage-rates-by-week-and-age-risks-and-statistics_00633174/.
- Ventura, S.J., et al., Estimated pregnancy rates and rates of pregnancy outcomes for the United States, 1990-2008. Natl Vital Stat Rep, 2012. 60(7): p. 1-21.