Flu Vaccination Coverage, United States, 2016-17 Influenza Season
Data sources: National Immunization Survey-Flu (NIS-Flu) and Behavioral Risk Factor Surveillance System (BRFSS)
Key Findings
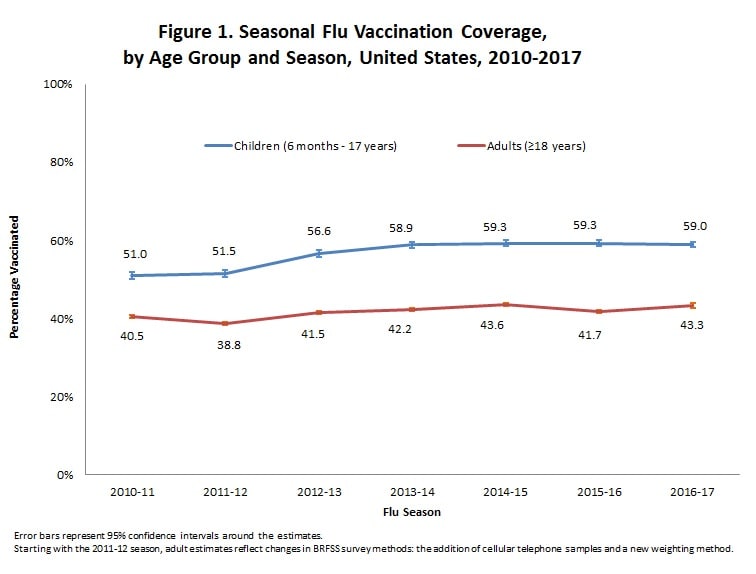
- Parent-reported flu vaccination coverage among children 6 months through 17 years for the 2016–17 season did not change compared with the 2015–16 season.
- Self-reported flu vaccination coverage among adults increased by 1.6 percentage points for the 2016–17 season compared with the 2015–16 season.
- State-by-state variability in child and adult flu vaccination coverage continues to be large.
Influenza (flu) is a contagious respiratory illness that can cause mild to severe illnesses resulting in hospitalization or even death. Some people are more likely to develop severe illness from flu, especially people 65 years and older, children younger than 5 years, people with certain long-term health conditions, and pregnant women. Many people do not receive an annual flu vaccination, even though an annual flu vaccination is recommended by the Advisory Committee on Immunization Practices (ACIP) for all persons aged ≥6 months who do not have contraindications to vaccination and is the primary way to prevent sickness and death caused by flu.(1) Health care providers can use the information in this report to identify people who may be at risk of not getting vaccinated and ensure measures are in place to recommend and offer flu vaccination as early as possible to protect the greatest number of people.
Additional vaccination coverage estimates for the 2016–17 and earlier flu seasons for each state, Health and Human Services (HHS) region, and overall for the United States are provided on FluVaxView as interactive maps, figures, and tables. Coverage estimates for health care personnel and pregnant women are reported in the Morbidity and Mortality Weekly Report (MMWR).
Who Was Vaccinated?
- Adults (18 years and older)
- Coverage by Sex
- Children (6 months through 17 years)
- Adults (18 years and older)
- Children (6 months through 17 years)
- Adults (18 years and older)
- All Ages (6 months and older)
- Children (6 months through 17 years)
- Adults (18 years and older)
- Children (6 months through 17 years)
- Adults (18 years and older)
- Coverage by Race/Ethnicity
- All Ages (6 months and older)
- Children (6 months through 17 years)
- Adults (18 years and older)
- Coverage by Month
- Children (6 months through 17 years)
- Adults (18 years and older)
- Estimated Number of Persons Vaccinated
- All Ages (6 months and older)
- Children (6 months through 17 years)
- Adults (18 years and older)
- Children (6 months through 17 years)
- Adults (18 years and older)
Coverage by Age Group
- Among all people ≥6 months, flu vaccination coverage during the 2016–17 flu season was 46.8%, which is 1.2 percentage points higher than coverage during the 2015–16 season (45.6%).
- State-specific flu vaccination coverage among all people ≥6 months ranged from 36.1% (Nevada) to 55.4% (Rhode Island).
| Age Group | Unweighted Sample Size | %‡ ± 95% CI§ | Difference from the 2015–16 Season ± 95% CI |
|---|---|---|---|
| All People ≥6 months | 468,970 | 46.8 ± 0.5 | 1.2 ± 0.6|| |
| Children (6 months–17 years) | 143,169 | 59.0 ± 0.7 | -0.3 ± 1.1 |
| Adults (≥18 years) | 325,801 | 43.3 ± 0.6 | 1.6 ± 0.7|| |
Children (6 months through 17 years)
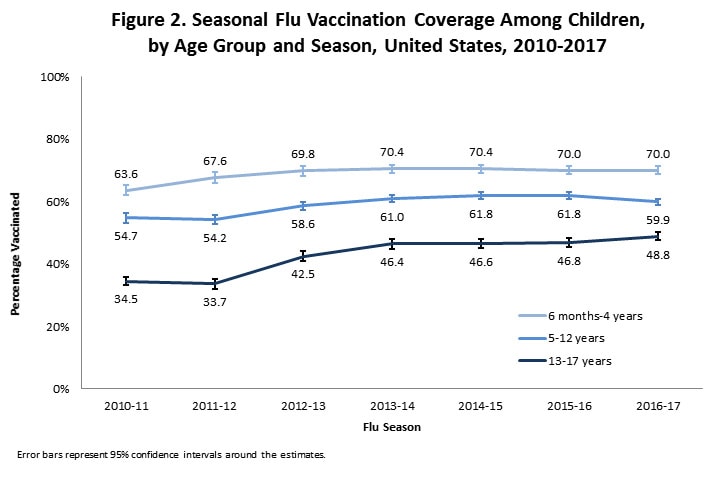
- Among children 6 months through 17 years, coverage with one or more doses of flu vaccine was 59.0%, similar to the 2015–16 season (59.3%).
- Flu vaccination coverage among children 6 months through 17 years decreased with increasing age:
- 6–23 months: 76.3%
- 2–4 years: 66.2%
- 5–12 years: 59.9%
- 13–17 years: 48.8%
- This trend has been observed previously.
- Among children 5–12 years, coverage for the 2016–17 season was 1.9 percentage points lower than coverage for the 2015–16 season.
- Among children 13–17 years, coverage for the 2016–17 season was 2.0 percentage points higher than coverage for the 2015–16 season.
- State-specific flu vaccination coverage for children 6 months through 17 years ranged from 43.0% (Wyoming) to 74.2% (Rhode Island).
| Age Group | Unweighted Sample Size | %‡ ± 95% CI§ | Difference from the 2015–16 Season ± 95% CI |
|---|---|---|---|
| 6 months−17 years | 143,169 | 59.0 ± 0.7 | -0.3 ± 1.1 |
| 6 months−4 years | 44,094 | 70.0 ± 1.3 | 0.0 ± 1.9 |
| 6−23 months | 16,374 | 76.3 ± 2.0 | 1.0 ± 2.6 |
| 2–4 years | 27,720 | 66.2 ± 1.6 | -0.6 ± 2.4 |
| 5−17 years | 99,075 | 55.6 ± 0.8 | -0.3 ± 1.2 |
| 5–12 years | 63,130 | 59.9 ± 1.0 | -1.9 ± 1.6|| |
| 13–17 years | 35,945 | 48.8 ± 1.3 | 2.0 ± 1.9|| |
Estimates of the reported place of flu vaccination by age group are also available.
- Among adults ≥18 years, coverage was 43.3%, which was 1.6 percentage points higher than coverage during the 2015–16 season (41.7%).
- Coverage among adults 18 years and older increased with increasing age:
- 18–49 years: 33.6%
- 50–64 years: 45.4%
- ≥65 years: 65.3%
- This trend has been observed previously.
- Adults 50−64 years had an increase in coverage of 1.8 percentage points compared to the 2015–16 season, while adults 65 years and older had an increase in coverage of 1.9 percentage points. Adults 18−49 years did not have a statistically significant change in coverage.
- State-specific coverage for adults 18 years and older ranged from 33.4% (Nevada) to 51.1% (South Dakota).
| Age Group | Unweighted Sample Size | %‡ ± 95% CI§ | Difference from the 2015–16 Season ± 95% CI |
|---|---|---|---|
| ≥18 years | 325,801 | 43.3 ± 0.6 | 1.6 ± 0.7|| |
| 18−64 years | 206,532 | 37.5 ± 0.6 | 1.2 ± 0.8|| |
| 18−64 years with high risk conditions¶ | 54,748 | 46.4 ± 1.2 | 0.4 ± 1.7 |
| 18−64 years without high risk conditions | 149,533 | 34.9 ± 0.8 | 1.4 ± 1.0|| |
| 18−49 years | 107,527 | 33.6 ± 0.8 | 0.9 ± 1.1 |
| 18−49 years with high risk conditions | 19,092 | 39.3 ± 1.8 | -0.2 ± 2.7 |
| 18−49 years without high risk conditions | 87,094 | 32.6 ± 0.8 | 1.1 ± 1.1 |
| 50−64 years | 99,005 | 45.4 ± 1.0 | 1.8 ± 1.3|| |
| ≥65 years | 119,269 | 65.3 ± 1.0 | 1.9 ± 1.3|| |

Coverage by Sex
Children (6 months through 17 years)
- There were no differences in flu vaccination coverage between male and female children.
- For adults, flu vaccination coverage was higher among females than males for every age group except age ≥65 years.
| Male | Female | |||
|---|---|---|---|---|
| Age Group | Unweighted Sample Size | %‡ ± 95% CI§ | Unweighted Sample Size | % ± 95% CI |
| All Ages | ||||
| ≥6 months | 215,954 | 43.8 ± 0.6 | 252,937 | 49.6 ± 0.7 |
| Children | ||||
| 6 months−17 years | 74,533 | 58.9 ± 1.0 | 68,636 | 59.2 ± 1.0 |
| 6 months−4 years | 22,901 | 69.3 ± 1.8 | 21,193 | 70.8 ± 1.8 |
| 6−23 months | 8,508 | 76.5 ± 2.6 | 7,866 | 76.1 ± 2.8 |
| 2−4 years | 14,393 | 64.8 ± 2.2 | 13,327 | 67.6 ± 2.2 |
| 5−17 years | 51,632 | 55.6 ± 1.2 | 47,443 | 55.5 ± 1.2 |
| 5−12 years | 32,814 | 59.9 ± 1.5 | 30,316 | 59.9 ± 1.5 |
| 13−17 years | 18,818 | 49.0 ± 1.8 | 17,127 | 48.6 ± 2.0 |
| Adults | ||||
| ≥18 years | 141,421 | 39.3 ± 0.8** | 184,301 | 47.0 ± 0.8** |
| 18−64 years | 94,212 | 33.5 ± 1.0** | 112,264 | 41.4 ± 1.0** |
| 18−64 years with high risk conditions¶ | 22,049 | 43.4 ± 2.0** | 32,685 | 48.7 ± 1.8** |
| 18−64 years without high risk conditions | 70,961 | 31.2 ± 1.0** | 78,535 | 38.8 ± 1.0** |
| 18−49 years | 51,037 | 29.5 ± 1.0** | 56,453 | 37.9 ± 1.2** |
| 18−49 years with high risk conditions | 7,243 | 34.9 ± 2.7** | 11,840 | 42.5 ± 2.4** |
| 18−49 years without high risk conditions | 43,049 | 28.9 ± 1.2** | 44,019 | 36.8 ± 1.4** |
| 50−64 years | 43,175 | 42.5 ± 1.6** | 55,811 | 48.0 ± 1.4** |
| ≥65 years | 47,209 | 65.1 ± 1.8 | 72,037 | 65.4 ± 1.2 |
Coverage by Race/Ethnicity
- Estimates for children and adults combined (all people ≥6 months) are presented here even though the patterns of racial/ethnic differences in flu vaccination coverage estimates differ for children and adults.
- Among people ≥6 months, coverage for non-Hispanic whites (47.5%) was higher than that for non-Hispanic blacks (43.0%) and AI/ANs (41.8%).
- In addition to the previously mentioned differences, coverage for Asians (52.8%) was higher than coverage for non-Hispanic whites (47.5%), non-Hispanic blacks (43.0%), Hispanics (46.2%), AI/ANs (41.8%), and people of other or multiple races (46.7%). Additionally, Hispanics (46.2%) had higher coverage than blacks (43.0%) and AI/ANs (41.8%), and persons of other or multiple races (46.7%) had higher coverage than blacks (43.0%) and AI/ANs (41.8%). For all other racial/ethnic group comparisons, there were no statistically significant differences.
| Race/Ethnicity†† | Unweighted Sample Size | %‡ ± 95% CI§ | Difference from the 2015–16 Season ± 95% CI |
|---|---|---|---|
| Overall | 468,970 | 46.8 ± 0.5 | 1.2 ± 0.6|| |
| White only, non-Hispanic | 335,532 | 47.5 ± 0.5 | 0.9 ± 0.7|| |
| Black only, non-Hispanic | 39,263 | 43.0 ± 1.3 | 0.2 ± 1.8 |
| Hispanic | 49,486 | 46.2 ± 1.5 | 2.3 ± 2.1|| |
| Other, non-Hispanic (Total) | 39,092 | 48.8 ± 1.9 | 1.7 ± 2.7 |
| Asian | 13,559 | 52.8 ± 3.3 | 1.5 ± 4.3 |
| American Indian/Alaska Native (AI/AN) | 7,081 | 41.8 ± 3.3 | -4.2± 4.9 |
| Other or multiple races‡‡ | 18,452 | 46.7 ± 2.7 | 4.3 ± 4.0|| |
Additional race/ethnicity estimates by age group are also available Cdc-excel[Excel – 16 KB].
- Among adults, flu vaccination coverage for non-Hispanic whites (45.9%) was higher than for non-Hispanic blacks (37.4%), Hispanics (36.9%), AI/ANs (37.5%) and adults of other or multiple races (41.7%).
- Additionally, Asian adults (47.1%) reported higher flu vaccination coverage than non-Hispanic blacks (37.4%), Hispanics (36.9%), and AI/ANs (37.5%). Adults of other or multiple races (41.7%) had higher coverage than black adults (37.4%) and Hispanics (36.9%). For all other racial/ethnic group comparisons, there were no statistically significant differences.
- Among adults, coverage during the 2016–17 season increased by 1.4 percentage points for non-Hispanic white adults compared with the 2015–16 season; there were no statistically significant changes in the other racial/ethnic groups.
| Race/Ethnicity†† | Unweighted Sample Size | %‡ ± 95% CI§ | Difference from the 2015–16 Season ± 95% CI |
|---|---|---|---|
| Overall | 325,801 | 43.3 ± 0.6 | 1.6 ± 0.7|| |
| White only, non-Hispanic | 253,191 | 45.9 ± 0.6 | 1.4 ± 0.8|| |
| Black only, non-Hispanic | 25,067 | 37.4 ± 1.6 | 0.8 ± 2.3 |
| Hispanic | 21,680 | 36.9 ± 2.0 | 2.5 ± 2.7 |
| Other, non-Hispanic (Total) | 20,266 | 43.6 ± 2.5 | 2.6 ± 3.5 |
| Asian | 6,440 | 47.1 ± 4.3 | 3.1 ± 5.4 |
| American Indian/Alaska Native (AI/AN) | 5,024 | 37.5 ± 3.7 | -5.4 ± 5.5 |
| Other or multiple race‡‡ | 8,802 | 41.7 ± 3.7 | 5.3 ± 5.4 |
Additional race/ethnicity estimates by age group are also available Cdc-excel[Excel – 17 KB].
Coverage by Month
Children (6 months through 17 years)
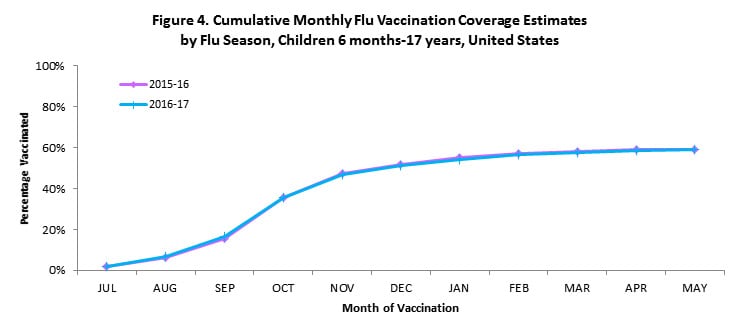
- Among children 6 months through 17 years, cumulative flu vaccination coverage across the months of vaccination for the 2016–17 season was similar to the 2015–16 season (Figure 4).
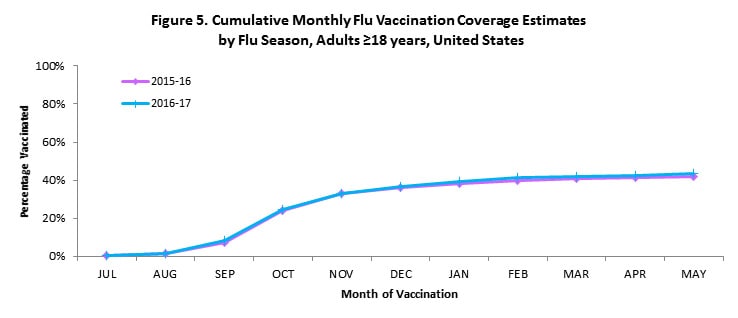
- Among adults ≥18 years, cumulative coverage across the months of vaccination was slightly higher for the 2016–17 season compared with the 2015–16 season (Figure 5).
Estimated Number of People Vaccinated
Based on reports of vaccination from survey respondents, the estimated number of persons who received one or more seasonal flu vaccinations was 41.8 million (95% Confidence Interval [CI]: 41.3–42.3 million) children (6 months through 17 years) and 107.4 million (95% CI: 105.9–108.9 million) adults (≥18 years), for an estimated 149.2 million (95% CI: 147.2–151.2 million) people vaccinated against seasonal flu during July 2016 through May 2017 among the U.S. population. These estimates do not include second doses given to children. The actual number of doses of flu vaccine distributed during the 2016–17 season was 145.9 million, indicating that the flu vaccination coverage estimates in this report may be high. Overestimates of vaccination coverage may be due to a combination of factors, including respondents having higher coverage than persons not surveyed (response bias), recall bias, or other factors. Examples of studies in which medical record validation has been compared with adult patient or parent report of vaccination estimated that coverage by parental report was seven percentage points too high for children 6–59 months and coverage by self-report was 5-11 percentage points too high for adults ≥65 years.(2;3) While the vaccination coverage estimates in this report were not validated with medical records, the NIS-Flu and BRFSS estimates do provide important information regarding yearly trends in reported vaccination over time.
What Can Be Done?
For children, flu vaccination coverage for the 2016–17 season was similar compared with the 2015–16 season while there was a small increase for adults. Differences in coverage among racial/ethnic populations by age group and variation in coverage by state were noted and consistent with findings from prior flu seasons. Flu vaccination coverage for the 2016–17 season for all groups except children 6–23 months remains below the Healthy People 2020 targetsExternal§§ of 70.0% vaccination coverage for persons 6 months through 17 years and ≥18 years.(4)
These findings can be used by health care providers to identify people who may be at risk of not receiving a flu vaccination. Optimally, people should receive their flu vaccinations before the influenza viruses begin to circulate in the community. If possible, health care providers should offer flu vaccinations by the end of October and continue to offer vaccinations as long as flu viruses are circulating.(1)
Strategies to increase flu vaccination coverage in the United States include:
- Encouraging use of evidence-based strategies at medical and non-medical sites to increase access to vaccination services (e.g., reducing client costs and vaccination programs in schools and Women, Infants, and Children [WIC] settings), increasing community demand for vaccinations (e.g., client reminder/recall systems), and ensuring that all those who visit a provider during the flu season receive a vaccination recommendation and offer from their provider (e.g., standing orders and provider reminders).(5)
- Expanding access through use of non-traditional settings (e.g., pharmacy, workplace, and school venues) to reach people in settings other than traditional physicians’ offices during the flu season.(6)
- Broadening use of interventions to remove barriers to accessing vaccination.(7)
- Encouraging multi-sector collaborations, including culturally relevant communications to reach specific target populations, and implementing effective interventions to reduce vaccination disparities in the United States.(8)
- Additional strategies are described in the Community Guide for Preventive ServicesExternal.(5)
Updated recommendations have been published for the 2017–18 flu season.(1) Updated information includes 1) the composition of U.S. seasonal flu vaccines; 2) the expected flu vaccine products available for the 2017–18 season; and 3) an extension of interim recommendation to not use the live, attenuated influenza vaccine (LAIV) for the 2017–18 season.(1)
Data Sources and Methods
For this report, the Centers for Disease Control and Prevention (CDC) analyzed data from the National Immunization Survey-Flu (NIS-Flu) for children 6 months through 17 years and the Behavioral Risk Factor Surveillance System (BRFSS) for adults ≥18 years to estimate national, state, and local flu vaccination coverage from the 2016–17 flu season.
CDC analyzed NIS-Flu and BRFSS data collected September (BRFSS) or October (NIS-Flu) 2016 through June 2017 from all 50 states and the District of Columbia to estimate national- and state-level flu vaccination coverage for vaccines administered from July 2016 through May 2017 for the 2016–17 flu season. These findings were compared with 2015–16 flu season estimates. Estimates are also included as a supplemental table to this report for Guam, Puerto Rico, the U.S. Virgin Islands, and selected local areas.
The NIS-Flu has three components: the NIS, which includes households with children 19–35 months, the NIS-Teen, which includes households with children 13–17 years, and a short flu vaccination module, which is conducted for households with children 6–18 months and 3–12 years. The NIS-Flu is a national dual landline and cellular list-assisted random-digit-dialed telephone survey of households. Respondents ≥18 years were asked if their child had received a flu vaccination since July 1, 2016, and, if so, in which month and year; this information was parent-reported and not verified by medical records. The range of the Council of American Survey and Research Organizations (CASRO) response rates for the NIS-Flu across the components of the NIS-Flu were 50.8% to 53.1% for landline and 26.2% to 28.7% for cellular telephones.
BRFSS is an ongoing state-based monthly telephone survey which collects information on health conditions and risk behaviors from randomly selected people ≥18 years among the U.S. population. BRFSS respondents were asked if they had received a flu vaccine in the past 12 months, and if so, in which month and year; this information was self-reported and not verified by medical records. The median state BRFSS response rate was 47.4% for September–December 2016 and 45.5% for January–June 2017. Starting in 2011, BRFSS methods changed by adding persons in households with only cellular telephone service and improving weighting procedures; these changes were reflected in the 2011–12 and subsequent flu vaccination coverage estimates.(9)
Flu vaccination coverage estimates from both surveys were calculated using Kaplan-Meier survival analysis to determine the cumulative flu vaccination coverage (≥1 dose) July 2016 through May 2017 using monthly interview data collected September (BRFSS) or October (NIS-Flu) 2016 through June 2017. NIS-Flu data were used to estimate coverage for children 6 months through 17 years and BRFSS data were used to estimate coverage for adults ≥18 years. Coverage estimates for all persons ≥6 months were determined using combined state-level monthly estimates weighted by the age-specific populations of each state.(10) For the 21.8% of NIS-Flu and 6.6% of BRFSS participants who indicated they had been vaccinated but had a missing month and year of vaccination, information was imputed from donor pools matched for week of interview, age group, state of residence, and race/ethnicity. Information on high-risk conditions was missing for 1.1% of adults and race/ethnicity was missing for 1.7% of adults; adults with missing data were not included in the estimates by risk condition or race/ethnicity. Results from both surveys were weighted and analyzed using SAS and SUDAAN statistical software to account for the complex survey design. Differences between groups and between 2015–16 and 2016–17 seasons were determined using t-tests with significance at p<0.05. Differences mentioned in this report were statistically significant.
Limitations
The estimates in this report are subject to the following limitations. First, flu vaccination status was based on self or parental report and not validated with medical records and, thus, is subject to respondent recall bias.(2;3) A recent study of children 6–23 months included estimates of flu coverage with ≥1 doses based upon provider report; when these estimates were compared with the parent-reported estimates found on FluVaxView, the parent-reported estimates were between 12-17 percentage points higher than provider report for the 2010–11 through 2012–13 flu seasons.(11) Also in this study, racial/ethnic differences among children 6–23 months were identified based on provider-reported vaccination status, but the pattern of racial/ethnic vaccination differences was different than patterns found on FluVaxView based on parental report.(11) Incomplete records and reporting, however, might affect provider-reported vaccination histories.(11) Second, response rates for NIS-Flu and BRFSS surveys were low and nonresponse bias may remain even after weighting adjustments. A comparison of NIS-Flu estimates with those from National Health Interview Survey suggests that the NIS-Flu estimates have a slight upward nonresponse bias.(12;13) Third, combining NIS-Flu and BRFSS estimates allowed estimation of coverage for all persons ≥6 months; however, differences in survey methodology (e.g., different sampling frame, survey design, exact survey question wording, response rates, and weighting) may result in different levels of bias that are averaged for this group. Fourth, the number of persons vaccinated was overestimated, evidenced by a higher number vaccinated than doses distributed as has occurred previously.(14)
Authors
Tammy A. Santibanez, PhD; Yusheng Zhai, MSPH; Alissa O’Halloran, MSPH; Katherine E. Kahn, MPH; Anup Srivastav, DVM, PhD; Lin Liu, MS; Elizabeth Ormson, MS; Peng-Jun Lu, MD, PhD; Walter W. Williams, MD, MPH; Stacie M. Greby, DVM, MPH.
Related Links
National Immunization Survey-Flu (NIS-Flu):
Behavioral Risk Factor Surveillance System (BRFSS):
NIS-Flu/BRFSS vaccination coverage reports:
General information about flu:
Footnotes
* Estimates of the percentage of people vaccinated are based on interviews conducted beginning September (BRFSS) or October (NIS-Flu) 2016 through June 2017 and reported vaccinations from July 2016 through May 2017. † Excludes U.S territories. ‡ Percentage vaccinated. Percentages are weighted to the U.S. population. Month of vaccination was imputed for respondents with missing month of vaccination data. § Confidence interval (CI) half-widths. || Statistically significant difference between the 2016–17 season and the 2015–16 season by t-test (p<0.05). ¶ Selected high risk conditions includes people with asthma, diabetes, heart disease, chronic obstructive pulmonary disease, or cancers other than skin cancer. **Statistically significant difference between male and female estimates by t-test (p<0.05). ‡‡ Includes Native Hawaiian or other Pacific Islander, multiracial, and other races. §§ The National Health Interview Survey (NHIS) is the data source used to monitor the Healthy People objectives for flu vaccination (IID-12.11-14). Final NHIS estimates for the 2016–17 season will be available by September 2018. A comparison of estimates from NIS-Flu and BRFSS to NHIS is available.
References
(1) Grohskopf LA, Sokolow LZ, Broder KR et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices–United States, 2017-18 influenza season. MMWR Recomm Rep2017;66:1-21. (2) MacDonald R, Baken L, Nelson A, Nichol KL. Validation of self-report of influenza and pneumococcal vaccination status in elderly outpatients. Am J Prev Med 1999;16:173-177. (3) Brown C, Clayton-Boswell H, Chaves SS et al. Validity of parental report of influenza vaccination in young children seeking medical care. Vaccine 2011;29:9488-9492. (4) U.S.Department of Health and Human Services. Healthy People 2020. Topics & Objectives-Immunization and Infectious Diseases. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives [serial online] 2015; Accessed September 11, 2015. (5) Guide to Community Preventive Services. Increasing appropriate vaccination. www.thecommunityguide.org [serial online] 2013; Accessed July 30, 2013. (6) Murphy PA, Frazee SGCJP, Cohen E, Rosan JR, Harshburgher DE. Pharmacy provision of influenza vaccinations in medically underserved communities. J Am Pharm Assoc 2012;52:67-70. (7) Poland GA, Shefer AM, McCauley M, Webster PS, Whitley-Williams PN, Peter G. Standards for adult immunization practices. Am J Prev Med 2003;25:144-150. (8) CDC. CDC health disparities and inequalities report–United States, 2013. MMWR 2013;62:3-5. (9) CDC. Methodologic changes in the Behavioral Risk Factor Surveillance System in 2011 and potential effects on prevalence estimates. MMWR 2012;61:410-413. (10) Furlow-Parmley C, Singleton JA, Bardenheier B, Bryan L. Combining estimates from two surveys: an example from monitoring 2009 influenza A(H1N1) pandemic vaccination. Stat Med 2012;31:3285-3294. (11) Santibanez TA, Grohskopf LA, Zhai Y, Kahn KE. Complete influenza vaccination trends for children six to twenty-three months. Pediatrics 2016;137:e20153280. (12) Santibanez TA, Lu PJ, O’Halloran A, Meghani A, Grabowsky M, Singleton JA. Trends in Childhood Influenza Vaccination Coverage–U.S., 2004-2012. Public Health Rep 2014;129:417-427. (13) CDC. Surveillance of influenza vaccination coverage–United States, 2007-08 through 2011-12 influenza seasons. MMWR CDC Surveill Summ 2013;62:1-28. (14) CDC. Interim results: state-specific seasonal influenza vaccination coverage–United States, August 2009-January 2010. MMWR Morb Mortal Wkly Rep 2010;59:477-484.