This Year's Work
Our Work - 2017
Updated guidelines for responding to pandemic flu
On April 21, HHS/CDC released a set of updated pre-pandemic planning guidelines entitled Community Mitigation Guidelines to Prevent Pandemic Influenza – United States, 2017. These guidelines replace the 2007 Interim Pre-pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States – Early, Targeted, Layered Use of Nonpharmaceutical Interventions (NPIs). The 2017 updated guidelines summarize key lessons learned from the 2009 H1N1 pandemic response, describe new or updated pandemic assessment and planning tools, and incorporate the latest scientific findings on the use of NPIs. In addition, six plain-language, pre-pandemic NPI planning guides are available online for different audiences and community settings. The supplemental guides can help states and localities operationalize the 2017 guidelines and assist them with pre-pandemic flu planning and decision-making. To access the updated guidelines, planning guides, and additional NPI communication, education, and training materials, please visit www.cdc.gov/npi.
New challenges in monitoring and preventing foodborne disease

Recent changes in the use of tests that diagnose foodborne illness pose challenges to monitoring illnesses and progress toward preventing foodborne disease, according to a report published April 20 in CDC’s Morbidity and Mortality Weekly Report. The MMWR article includes the most recent data from CDC’s Foodborne Diseases Active Surveillance Network, or FoodNet, which collects data on 15% of the US population. It summarizes preliminary 2016 data on nine germs spread commonly through food. In 2016, FoodNet reported 24,029 infections, 5,512 hospitalizations, and 98 deaths related to foodborne illness. Campylobacter and Salmonella caused the most reported bacterial foodborne illnesses in 2016.
New test to detect smallpox

In February, CDC’s Poxvirus and Rabies Branch received US Food and Drug Administration clearance for a diagnostic test to detect variola virus, the agent that causes smallpox. The new Variola Virus Real-time PCR Assay was designed to increase sensitivity and specificity and will replace the variola virus-specific test previously deployed to Laboratory Response Network (LRN) laboratories. The assay reagents and verification panels have been sent to qualified laboratories through the LRN. The deployment of the variola test enhances US government preparedness efforts to quickly detect and respond to a biological attack.
Dentists prescribe 10% of all antibiotic prescriptions in outpatient settings
Recent CDC study published in the Journal of the American Dental Association reported information about antibiotic prescribing among general dentists in the United States. The study found that although dentists usually prescribe within recommended guidelines, they sometimes prescribe antibiotics not indicated for dental conditions, such as fluoroquinolones and others used to treat urinary tract infections.
CDC’s Safe Healthcare Blog published Dr. Marie Fluent’s tips for supporting responsible antibiotic prescribing practices in dentistry. She is a dentist and educational consultant at the Organization for Safety, Asepsis, and Prevention.
Multistate outbreak linked to soy nut butter
CDC, FDA, and several states are investigating a multistate outbreak of 29 Shiga toxin-producing E. coli (STEC) O157:H7 infections reported from 12 states. Most of the sick people are children. The investigation has identified I.M. Healthy brand SoyNut Butter as the likely source of this outbreak. The SoyNut Butter Company recalled this product, as well as I.M. Healthy granola and Dixie Diner’s Club brand Carb Not Beanit Butter. CDC recommends that people not eat or serve these products. This investigation is ongoing.
Zika Update

Thirteen months into CDC’s Zika response, CDC continues to focus its efforts on reducing the risk of infections. CDC launched a series of eight 1-hour webinars to help state and local jurisdictions prepare for the 2017 Zika mosquito season. CDC also has updated its Zika travel guidance for pregnant women. CDC recommends that pregnant women not travel to areas where Zika virus has been newly introduced or reintroduced and mosquito-borne transmission is ongoing; areas where the virus was present before 2015 and there is no evidence transmission has stopped; and areas where the virus is likely to be circulating but has not been documented. This recommendation comes with a new World Map of Areas with Risk of Zika that allows users to search for location-specific Zika information and travel recommendations, and an interactive “Know Your Zika Risk” tool that offers tailored risk and prevention messages based on information provided by travelers.
A new analysis of Zika cases in Florida’s Miami-Dade County led CDC to alert residents of Broward and Palm Beach counties of a small potential increased risk of Zika virus transmission starting June 15, 2016. CDC recognized that people who regularly move between Miami-Dade, Broward, and Palm Beach counties may not realize they were traveling to an area with active mosquito-borne Zika virus transmission, and this movement between counties may pose a small but increased risk for Zika transmission. This increased risk is particularly relevant for Zika transmission via semen, because of evidence regarding the persistence of Zika virus in this reproductive tissue. Although blood donations in the United States are tested for Zika, there are no tests for tissue donors, including semen donors. CDC encourages women and their partners, in consultation with their healthcare providers, to consider this potential risk when trying to conceive.
Vaccine study to prevent monkeypox in DRC

A CDC-sponsored study to evaluate the effectiveness of Imvamune, a third-generation vaccine against smallpox, has begun. The study focuses on preventing infections from monkeypox virus, which is related to smallpox virus, in at-risk health care workers and laboratorians in Democratic Republic of Congo (DRC). The study has so far enrolled 24 participants in Kinshasa. In June, the second phase of the study will begin in Tshuapa, an area with a high risk of monkeypox infections among community members, placing healthcare workers at risk for infection. After smallpox eradication in 1980, countries around the world stopped regular vaccinations against the disease. Waning immunity to smallpox is thought to have contributed to the increased reports of monkeypox in Central and West Africa.
Investigating group A strep in Alaska

Teams from CDC’s Arctic Investigations Program partnered with state and local health officials in Anchorage, AK, to investigate and treat outbreaks of group A Streptococcus (group A strep) infection occurring in the homeless population there. CDC epidemiologists traveled to Anchorage in February to assist the Alaska Department of Health and Social Services with identification of risk factors for group A strep in the city’s homeless population. The CDC team helped implement and evaluate mass antibiotic treatment and infection control measures. An increase in the number of infections began in 2016 and has continued through the beginning of this year.
Outbreaks associated with imported foods

A small but increasing percentage of foodborne outbreaks in the United States is associated with imported food, according to an article authored by CDC scientists and published in a recent journal Emerging Infectious Diseases. From 1996 to 2000, imported food was linked to 1% of foodborne outbreaks, or about 3 outbreaks each year. From 2009 to 2014, imported food was linked to 5% of foodborne outbreaks, or about 18 outbreaks each year. Approximately 19% of food consumed in the United States is imported, including ≈97% of fish and shellfish, ≈50% of fresh fruits, and ≈20% of fresh vegetables. Knowing what imported foods are most often linked to outbreaks can help focus efforts to improve food safety and prevent future illnesses.
Learn about Salmonella and live poultry
It’s spring, which means that many people are buying chicks and ducklings for backyard flocks. Yet backyard flocks can make their owners sick if proper precautions aren’t followed, as shown by the record number of Salmonella infections linked to backyard flocks in 2016. Before the spring selling season started, CDC distributed educational materials on preventing live-poultry-associated Salmonella illnesses to agricultural retail stores, hatcheries, and state agriculture department and health department collaborators.
CDC assists with cholera vaccination campaign

CDC is working with Cameroon’s ministry of health, the World Health Organization, and other partners on a cholera vaccination campaign targeting an estimated 130,000 people who live in Mogode District, bordering Nigeria in the Far North Region. This district has had multiple cholera outbreaks and has been the source of nationwide cholera epidemics in the past. The vaccine campaign is scheduled to take place in March and April, before the onset of the rainy season. CDC also assists Cameroon with other activities related to cholera preparedness, detection, and response through the Global Health Security Agenda.
Ebola virus detected in Ebola survivor 565 days after recovery

A team of CDC researchers recently published a study detailing the persistence of Ebola virus in the semen of a male survivor of Ebola virus disease. On August 27, 2014, Ebola virus was detected in the semen of a 48-year-old Ebola survivor in Liberia 565 days after his recovery from the Ebola. The patient also had a pre-existing HIV infection, which he was managing with treatment. While being treated for Ebola he continued his antiretroviral therapy regimen and was discharged from the Ebola treatment unit after his test came back negative for active Ebola virus infection. CDC researchers believe that the patient’s favorable response to the Ebola treatment despite being HIV positive could be linked to the patient’s compliance with his antiretroviral therapy regimen and adequate CD4 count. This emphasizes the importance of patients’ continuing their HIV treatment during an outbreak. The case highlights the need to continue researching the role that co-infections such as HIV and other causes of immunosuppression might play in the persistence of Ebola virus in male survivors of Ebola.
CDC assisting in Seoul virus outbreak investigation

CDC is working with the Illinois Department of Public Health and the Wisconsin Department of Health Services to investigate cases of Seoul virus infections among 10 people who were exposed to rats in several rat-breeding facilities in the 13 states. Seoul virus is not commonly found in the United States, although there have been several reported outbreaks in wild rats. This is the first known US outbreak associated with pet rats.
A home-based rodent breeder in Wisconsin was hospitalized in December 2016 with fever, headache, and other symptoms. CDC tested a blood specimen and confirmed that the infection was caused by Seoul virus, a member of the hantavirus family of rodent-borne viruses. A close family member who worked with rodents also tested positive for Seoul virus. Both people have recovered. A follow-up investigation at several rat-breeding facilities that supplied the initial patient’s rats revealed an additional six cases of Seoul virus at two Illinois rat-breeding facilities.
CDC has deployed two epidemiologists to work with local and state health authorities to determine if any customers who bought rats have become ill. Human and animal health officials are working together to make sure infected rats are not distributed further. CDC and its state and local health partners are reaching out to rodent suppliers to learn more about suppliers for the Wisconsin rat breeder. These efforts will help determine how the two individuals in Wisconsin were initially exposed to Seoul virus and allow public health officials to take actions to prevent future spread of the virus. CDC staff will also provide laboratory testing for blood samples from people who may have come in contact with rats from the affected rat breeders.
2016 NCEZID accomplishments now online!

Our annual recap of NCEZID’s work in 2016 to prevent infections and save lives has just been released. Although it is no surprise which topic made Number 1, topics 2 through 10 are equally engaging. It’s a good representation of the center’s work—from responding to the first-ever outbreak linked to E. coli bacteria in flour to the urgent efforts taken to contain the emerging fungus Candida auris that is spreading in healthcare settings. High-priority programs, like antibiotic resistance and advanced molecular detection, are also featured as is the Epidemiology and Laboratory Capacity for Infectious Diseases (ELC) Cooperative Agreement, which dispersed the largest award to states since the cooperative agreement started in 1995.
Zika update
As we turn the calendar to February, CDC continues to move forward with the Zika response. There is still much work to do as we prepare for this year’s mosquito season and support efforts to prevent Zika-related birth defects. Furthermore, local Zika virus transmission continues in Puerto Rico, where more than 34,500 cases have been reported as of January 25.
CDC continues to work with local and state health officials in Brownsville, Texas, where cases of locally transmitted Zika virus infection have been confirmed. On November 28, 2016, the Texas Department of State Health Services reported the state’s first case of local mosquito-borne Zika virus infection in a resident of Brownsville, Texas. Since then, five additional cases have been reported in people living close to the first case-patient CDC also continues to support local and state health officials in Miami-Dade County, Florida. Specific advice for people living in or traveling to South Florida and Brownsville, Texas can be found on the Zika website.
CDC recently awarded nearly $184 million to help states, territories, and local jurisdictions fight Zika. On January 6, CDC published the MMWR report that highlights the top 10 public health achievements and future priorities in relation to the Zika virus. Additionally, responders have compiled stories from staff members who have worked on the Zika response into a small book titled Zika: A Year of Firsts, which will be posted online soon.
Broad Agency Announcement awards to support Zika-related research
CDC will award almost $10 million to academic and industry partners to promote scientific research and innovation to enhance the United States’ ability to respond to Zika and other exotic and endemic vector-borne diseases. These funds will allow states and territories to develop the next generation of Zika virus diagnostic and vector-control tools and to evaluate the effectiveness of existing control methods.
Zika text messaging program
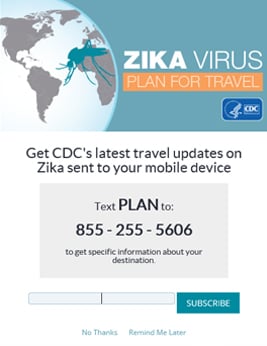
In an effort to explore mobile technology as a communication tool to better reach travelers in multiple languages and at various stages of travel, such as planning, during travel, and after travel, CDC launched the Zika text message program in August 2016. The program was initially promoted through limited unpaid social media posting and saw immediate uptake, indicating a clear audience interest in this communication channel.
Paid advertising of the program began in mid-November 2016, targeting travelers on a variety of digital platforms. In the first 5 months since launching, over 17,000 users across the US have opted in to the program, and nearly 64,000 text messages have been sent. The top destinations queried were Mexico, Puerto Rico, Bahamas, and Costa Rica, all of which are areas affected by Zika in which prevention messages are key.
CDC map of investments to combat AR
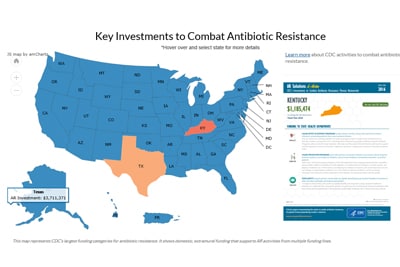
The CDC AR Investment Map launched in January. The tool is an interactive web app with printable state- and city-specific fact sheets describing CDC’s work to tackle antibiotic resistance (AR) using fiscal year 2016 funds.
Users can see how CDC supports AR activities by state and activity, including investments in:
- State and local public health partners to fight AR in healthcare facilities, the community, and food.
- Innovations and investigations to implement new ways to prevent antibiotic-resistant infections and contain their spread.
- Public health laboratories to boost state and local testing capacity and technology to detect and contain, support response to, and prevent AR threats nationwide. The AR Investment Map is one of the first tools at CDC to combine database-driven visuals and funding data to showcase CDC’s work.
- Page last reviewed: March 7, 2017
- Page last updated: March 7, 2017
- Content source:
Centers for Disease Control and Prevention
National Center for Emerging and Zoonotic Infectious Diseases (NCEZID)


 ShareCompartir
ShareCompartir


