Flu Vaccination Coverage, United States, 2022–23 Influenza Season
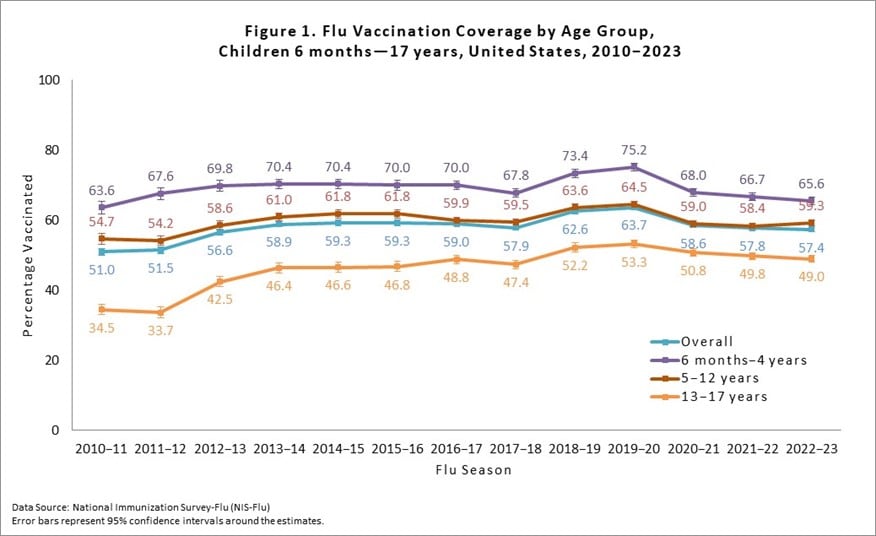
The Centers for Disease Control and Prevention (CDC) recommends annual influenza (flu) vaccination for all people ≥6 months who do not have contraindications [1]. To assess flu vaccination coverage for the 2022–23 flu season among children and adults in the United States, CDC analyzed data from two large, nationally representative surveys, the National Immunization Survey-Flu (NIS-Flu) and the Behavioral Risk Factor Surveillance System (BRFSS). This report contains CDC’s final flu vaccination coverage estimates for the 2022–23 flu season [2]. In the 2022–23 flu season, vaccination coverage with ≥1 dose of flu vaccine was 57.4% among children 6 months through 17 years, similar to the 2021–22 flu season (57.8%), and flu vaccination coverage among adults ≥18 years was 46.9%, a decrease of 2.5 percentage points from the prior season (49.4%). For children, while flu vaccination coverage had increased during the two seasons prior to the COVID-19 pandemic (2018–19 and 2019–20 seasons), coverage declined during the pandemic (2020–21 and 2021–22 seasons) and has not yet reached the immediate pre-pandemic levels. Flu vaccination coverage for children for the 2022–23 season, while showing no additional decrease from the 2021–22 season, is near the levels of the 2017–18 and prior seasons during which vaccination coverage was plateaued. For adults, after an initial increase in flu vaccination coverage in the season immediately following the start of the COVID-19 pandemic, coverage has steadily declined since the 2020–21 season and now appears similar to the 2019-20 season. Interpretation of the estimates in this report should take into consideration survey limitations.
An annual seasonal flu vaccine is the best way to help reduce the risk of getting flu and any of its potentially serious complications. For most people, September and October are ideal times to get vaccinated; however, vaccination should continue after October as long as flu viruses are circulating and unexpired vaccine is available. CDC expects flu viruses to spread along with other viruses this fall and winter, including respiratory syncytial virus (RSV) and the virus that causes COVID-19, and recommends that people stay up-to-date on all vaccinations.
Methods
For this report, CDC analyzed data from the NIS-Flu for children 6 months through 17 years and the BRFSS for adults ≥18 years to estimate national- and state-level flu vaccination coverage for the 2022–23 flu season. The analyses included data collected from interviews completed from September 2022 for BRFSS and October 2022 for NIS-Flu through June 2023 for vaccinations received between July 1, 2022, and the time of interview or by May 31, 2023, for those interviewed in June 2023.
The NIS-Flu is a national random-digit-dialed cellular telephone survey of households [3]. Respondents ≥18 years knowledgeable about the child’s vaccinations (hereafter referred to as “parent” in this report) were asked if their child received a flu vaccination since July 1, 2022, and the month of vaccination; this information was not verified by medical records. Month of vaccination was missing for 19.3% of respondents who indicated their child was vaccinated. For these children, month was imputed using the hot-deck imputation method from other survey respondents who matched the week of interview, age group, state of residence, and race/ethnicity of the child with missing data. Respondents who indicated the child received a flu vaccination were asked the place where the child was vaccinated. The range of the Council of American Survey and Research Organizations (CASRO) response rates for the NIS-Flu for the 2022–23 season was 23.4%–25.6%. The estimates for children are based on n=131,255 completed NIS-Flu interviews.
The BRFSS is a state-based random-digit-dialed cellular and landline telephone survey that collects information on various health conditions and risk behaviors from one randomly selected adult ≥18 years in a household. The BRFSS survey asks if the respondent has received a flu vaccine in the past 12 months and, if so, the month and year of vaccination [4]. For 9.5% of BRFSS participants who were vaccinated but had a missing month or year of vaccination, month and year were imputed using the hot-deck imputation method from other survey respondents who matched the week of the interview, age group, state of residence, and race/ethnicity of the respondent with missing data. Estimates are not available for the entire 2022–23 flu season for Kentucky, North Dakota, and Pennsylvania because interview data for January–June 2023 from these states were not available; therefore, estimates for Kentucky, North Dakota, and Pennsylvania represent vaccinations received only through November 2022 and not through May 2023 as for other states. The median state BRFSS response rate for a complete or partially complete interview was 44.5% for September–December 2022 and 45.4% for January–June 2023. The estimates for adults are based on n=297,255 completed BRFSS interviews.
Flu vaccination coverage estimates from both surveys were calculated using Kaplan-Meier survival analysis using the month of the reported flu vaccination to determine cumulative flu vaccination coverage. Coverage estimates for all persons ≥6 months were determined by combining the state-level monthly NIS-Flu and BRFSS estimates weighted by the age-specific populations of each state [5]. All estimates were weighted and analyzed using SAS and SAS-callable SUDAAN statistical software to account for the complex survey designs. Differences between groups and between 2022–23 and prior season (2021–22) estimates were determined using t-tests with significance at p<0.05. Increases or decreases noted in this report were statistically significant differences.
Results
Children aged 6 months through 17 years
Overall, the percentage of children receiving ≥1 dose of flu vaccine during the 2022–23 season was 57.4%. This was not a change from coverage in the 2021–22 season (57.8%; Figure 1). Flu vaccination coverage among children aged 6 months–4 years (65.6%), 5–12 years (59.3%), and 13–17 years (49.0%) did not differ from coverage in the previous season (Figure 1). Compared to the 2019-20 flu season (63.7%), the most recent pre-pandemic season, the percentage of children receiving ≥1 dose of flu vaccine during the 2022–23 season (57.4%) was 6.3 percentage points lower. For additional results by age group, see “Additional Flu Vaccination Coverage Estimates” at the end of this report.
Children – By State
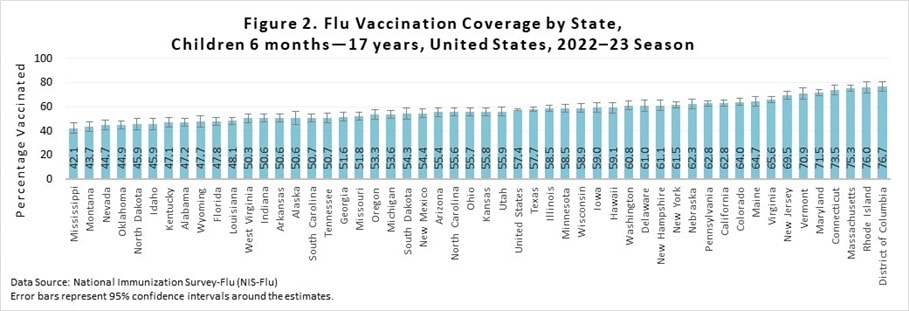
As is seen each flu season, there was wide (>34 percentage points) variability between states in flu vaccination coverage for children, ranging from 42.1% (Mississippi) to 76.7% (District of Columbia), (Figure 2). To view additional state-level final, end of flu season vaccination coverage estimates using the same methods described in this report, see the interactive application at FluVaxView Interactive.
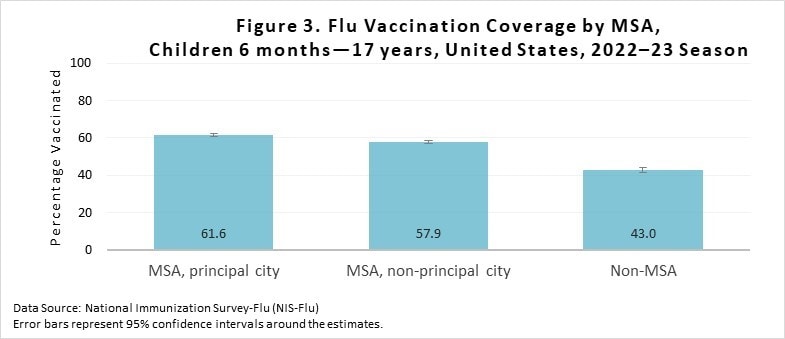
Vaccination coverage was higher for children living in a metropolitan statistical area (MSA) principal city (61.6%) compared to children living in a MSA non-principal city (57.9%) and children living in a non-MSA (43.0%) (Figure 3). Vaccination coverage was also higher for children living in a MSA non-principal city (57.9%) compared with children living in a non-MSA (43.0%). Additional results by MSA status are included in the “Additional Flu Vaccination Coverage Estimates” section of this report.
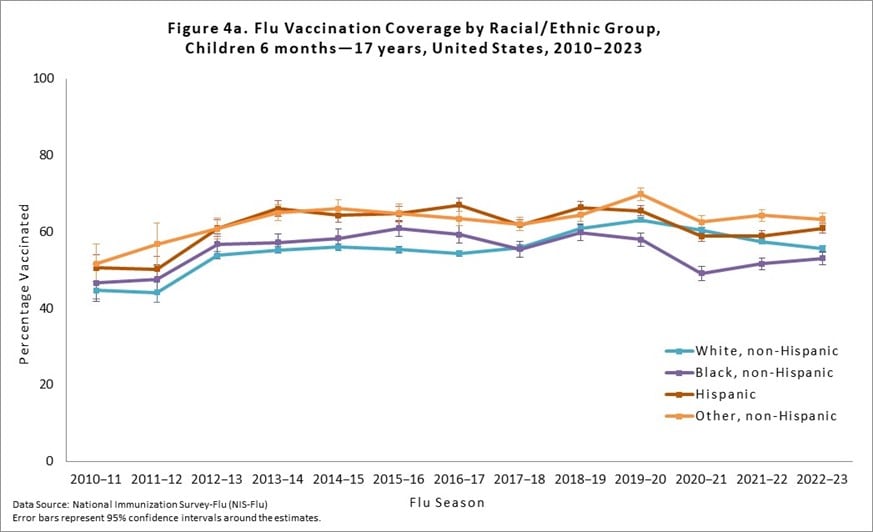
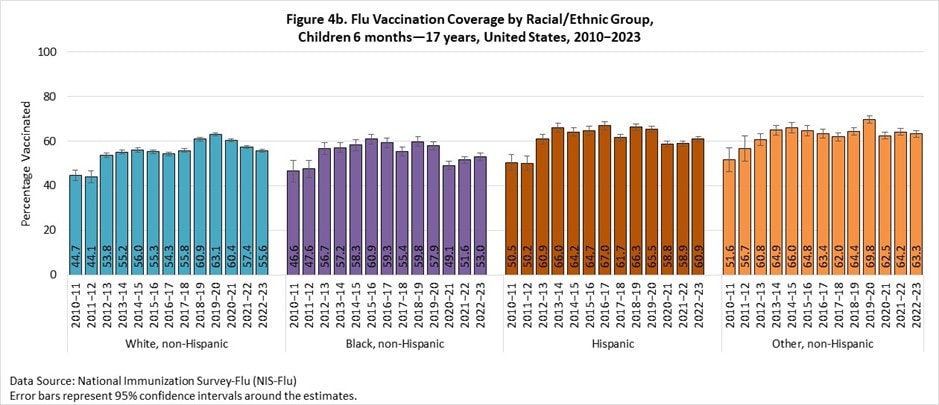
Flu vaccination coverage for the 2022–23 season was 1.8 percentage points lower among non-Hispanic White (White) children compared with the 2021–22 season and was 2.0 percentage points higher for Hispanic children. Coverage for non-Hispanic Black (Black) children and children of other or multiple races did not change compared with the previous season (Figures 4a and 4b). Compared with the pre-pandemic 2019–20 season, flu vaccination coverage for the 2022–23 season was 7.5 percentage points lower among White children, 4.9 percentage points lower for Black children, 4.6 percentage points lower for Hispanic children, and 6.5 percentage points lower for children of other or multiple races. Children of other/multiple races had higher flu vaccination coverage than Black, White, and Hispanic children. Hispanic children had higher coverage than White and Black children. Black children had lower coverage than White children. No other statistically significant pair-wise differences were observed. Flu vaccination coverage estimates for more detailed racial/ethnic groups (Asian, American Indian/Alaska Native) are provided as a table weblink in the “Additional Flu Vaccination Coverage Estimates” section of this report.
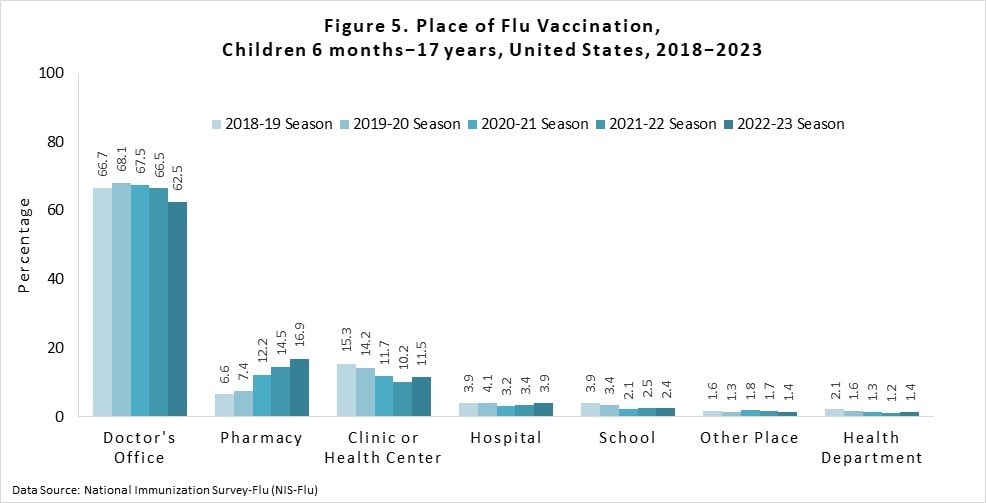
Place of flu vaccination among vaccinated children 6 months through 17 years for the 2022–23 season was most often a doctor’s office (63%), followed by a pharmacy (17%), and clinic/health center (12%) (Figure 5). Place of flu vaccination by child age groups can be found in the “Additional Flu Vaccination Coverage Estimates” section of this report.
Adults (≥18 years)
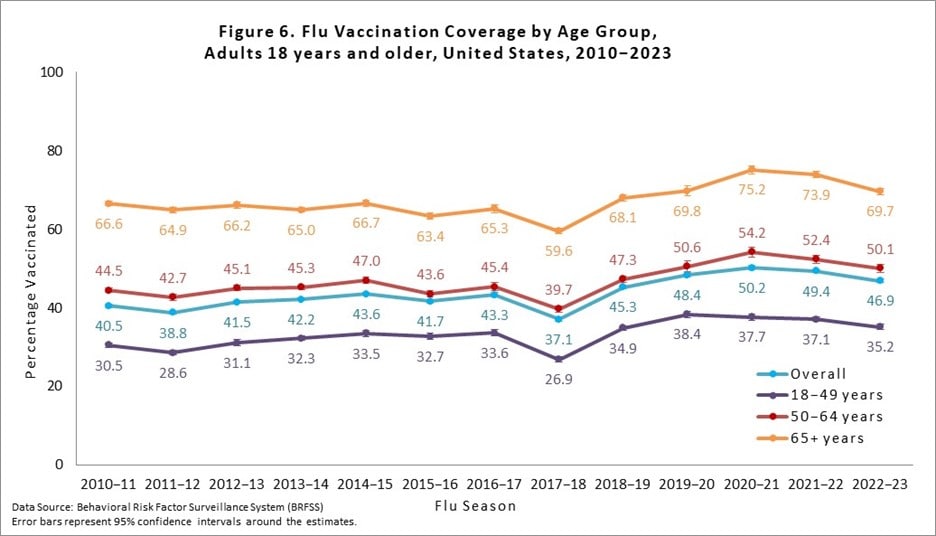
Overall, among adults ≥18 years, flu vaccination coverage was 46.9%, 2.5 percentage points lower than coverage during the 2021–22 season (49.4%; Figure 6). Flu vaccination coverage for 2022–23 was 1.9 percentage points lower among adults 18–49 years, 2.3 percentage points lower among adults 50–64 years, and 4.2 percentage points lower among adults ≥65 years compared to coverage during the 2021–22 season (Figure 6).
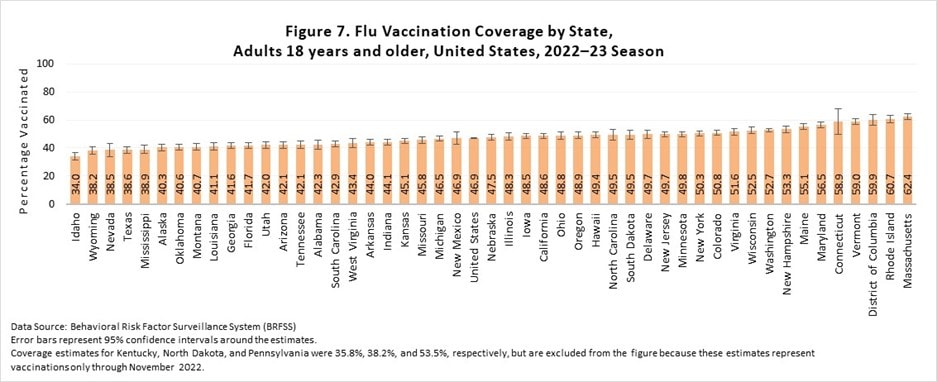
There was wide between-state variability in flu vaccination coverage among adults, ranging from 34.0% in Idaho to 62.4% in Massachusetts (Figure 7). See FluVaxView Interactive General Population for additional state-level estimates by age-groups and multiple flu seasons.
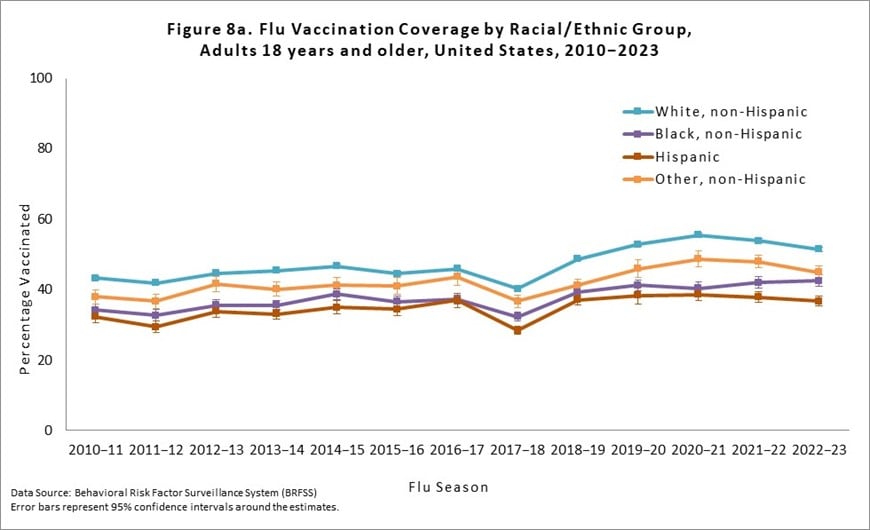
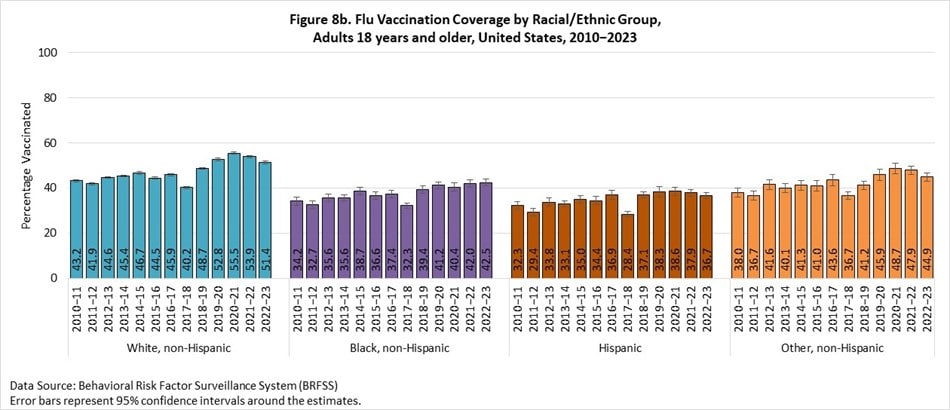
Flu vaccination coverage during the 2022–23 season for Non-Hispanic (NH) Black adults and Hispanic adults did not differ compared with the 2021–22 season, while White adults had a 2.5 percentage point decrease in coverage and adults of other or multiple races had a 3.0 percentage point decrease in coverage (Figures 8a and 8b). White adults had higher flu vaccination coverage than NH Black, Hispanic, and NH adults of other or multiple races. Additionally, Hispanic adults had lower flu vaccination coverage than adults of other or multiple races and NH Black adults had higher coverage than Hispanic adults. No other differences were observed. Flu vaccination coverage estimates for more detailed racial/ethnic groups (NH Asian, American Indian/Alaska Native) are provided as a table weblink in the “Additional Flu Vaccination Coverage Estimates” section at the end of this report.
All people 6 months and older
Flu vaccination coverage among all people ≥6 months during the 2022–23 season was 49.3%, 2.1 percentage points lower than coverage in the 2021–22 season (Table 1). Flu vaccination coverage during the 2022–23 season for Black people ≥6 months and Hispanic people ≥6 months did not differ compared with the 2021–22 season, while White people ≥6 months had a 2.4 percentage point decrease in coverage and people ≥6 months of other or multiple races had a 2.9 percentage point decrease in coverage (Table 1). NH White people had higher flu coverage than NH Black, Hispanic, and NH people of other or multiple races. Additionally, people of other or multiple races had higher coverage than NH Black and Hispanic people. No other differences were observed.
* Estimates of the percentage vaccinated are based on interviews conducted September (BRFSS) or October (NIS-Flu) 2022 through June 2023 and reported vaccinations from July 2022 through May 2023.
† Excludes U.S. territories.
‡ Race is self-reported; people of Hispanic ethnicity may be of any race.
§ Percentage vaccinated. Percentages are weighted to the U.S. population. Month of vaccination was imputed for respondents with missing month of vaccination data.
|| Confidence interval (CI) half-widths.
¶ Statistically significant difference between the 2022–23 season and the 2021–22 season by t-test (p<0.05).
** Includes Asian, American Indian/Alaska Native, Native Hawaiian or other Pacific Islander, multiracial, and other races.
- Flu Vaccination Coverage, by Age Group, Children, United States, 2022–23 Season [XLS – 12 KB]
- Flu Vaccination Coverage by Sex, Children, United States, 2022–23 Season [XLS – 14 KB]
- Flu Vaccination Coverage by Race/Ethnicity and Age Group, Children, United States, 2022–23 Season [XLS – 16 KB]
- Flu Vaccination Coverage for Local Areas and Territories, Children, 2022–23 Season [XLS – 65 KB]
- Place of Flu Vaccination by Age Group, Children, United States, 2022–23 Season [XLS – 16 KB]
Adults:
- Flu Vaccination Coverage, by Age Group and High Risk Status, Adults, United States, 2022–23 Season [XLS – 12 KB]
- Flu Vaccination Coverage by Sex, Adults, United States, 2022–23 Season [XLS – 14 KB]
- Flu Vaccination Coverage by Race/Ethnicity and Age Group, Adults, United States, 2022–23 Season [XLS – 16 KB]
- Flu Vaccination Coverage for Local Areas and Territories, Adults, 2022–23 Season [XLS – 45 KB]
Limitations
Several limitations of the estimates produced from the NIS-Flu and BRFSS surveys should be considered when interpreting the results in this report. First, survey weighting adjustments may not eliminate all the possible bias from incomplete sample frames; both surveys exclude households with no telephones, and NIS-Flu excludes households with only landline telephones. Second, response rates for both surveys were low, and flu vaccination coverage may differ between survey respondents and non-respondents; survey weighting adjustments may not adequately control these differences. Third, there may be misclassification of flu vaccination status due to recall errors of parents for NIS-Flu and of respondents for BRFSS [6, 7]. A study published in 2020 found that parents over-reported flu vaccination by approximately 9 percentage points.[8] Fourth, errors from incomplete sample frame, nonresponse, and accuracy of reported flu vaccination status might change over time, leading to inaccurate assessment of trends in flu vaccination coverage. Fifth, due to BRFSS interview data not being available for all months from Kentucky, North Dakota, and Pennsylvania, estimates for these three states represent vaccination coverage through November rather than through May. However, projected coverage (43.6% to 55.2%) for 2022–23 flu season using the relative increase in coverage during December-May from 2021-22 flu season for these states indicates it would not affect national coverage (46.9%). Sixth, estimates based on the sources in this report have differed from National Health Interview Survey (NHIS) estimates [9]. NHIS, the data source for evaluating progress toward the Healthy People 2030 flu vaccination coverage objectives, uses a different sampling method than the NIS-Flu and BRFSS, and uses in-person interviews but also relies on self or parental report. A recent study found that NIS-Flu estimates were generally higher than NHIS estimates over several flu seasons for children [9]. The final estimates in this report will differ from the preliminary, in-season, estimates on CDC’s FluVaxView Dashboard because of different surveys (BRFSS vs NIS-Adult Covid Module), different analytic approaches, and because more data are used for final estimates. The dashboard estimate for children was 56.1% whereas the final estimate included in this report is 57.4%; and for adults the dashboard estimate was 46.6% whereas the final included in this report is 46.9%. CDC continues to assess consistency between flu vaccination coverage estimates from different surveys and other data sources and to evaluate the accuracy of estimates from these data sources.
Discussion
During the 2022–23 season fewer than half of adults received a flu vaccination and about three in five children did. Coverage among adults is still nearly 20 percentage points lower than the Healthy People 2030 national target of 70% for flu vaccination of persons ≥6 months; coverage among children is lagging by approximately 12 percentage points. Racial and ethnic disparities in flu vaccination persist, particularly among adults. Increases in flu vaccination uptake are needed to reduce the burden of flu virus infection. An annual seasonal flu vaccine is the best way to help reduce the risk of getting flu and any of its potentially serious complications. For most people, September and October are ideal times to get vaccinated; however, if flu viruses are circulating, vaccination should continue into November and throughout the flu season. To avoid missed opportunities for vaccination, the Standards for Adult Immunization Practice recommends that all providers routinely assess individuals’ vaccination status at every clinical encounter, that they strongly recommend approved vaccinations to their patients, either offer needed vaccines or refer their patients to another provider who can administer the needed vaccines, and document vaccinations received by their patients in an immunization information system [10]. CDC expects flu viruses to spread along with other viruses this fall and winter, including respiratory syncytial virus (RSV) and the virus that causes COVID-19, and recommends that people stay up-to-date on all vaccinations.
References
- Grohskopf LA, Blanton LH, Ferdinands JM, Chung JR, Broder KR, Talbot HK. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices – United States, 2023-24 Influenza Season. MMWR Recomm Rep. 2023;72:1-25.
- CDC. FluVaxView, Influenza vaccination coverage by season. 2023.
- Wolter KK, Smith PJ, Khare M, Welch B, Copeland KR, Pineau VJ, et al. Statistical Methodology of the National Immunization Survey, 2005-2014. Vital and health statistics Ser 1, Programs and collection procedures. 2017:1-107.
- CDC. The BRFSS Data User Guide. 2013.
- Furlow-Parmley C, Singleton JA, Bardenheier B, Bryan L. Combining estimates from two surveys: an example from monitoring 2009 influenza A (H1N1) pandemic vaccination. Statistics in medicine. 2012;31:3285-94.
- Brown C, Clayton-Boswell H, Chaves SS, Prill MM, Iwane MK, Szilagyi PG, et al. Validity of parental report of influenza vaccination in young children seeking medical care. Vaccine. 2011;29:9488-92.
- Irving SA, Donahue JG, Shay DK, Ellis-Coyle TL, Belongia EA. Evaluation of self-reported and registry-based influenza vaccination status in a Wisconsin cohort. Vaccine. 2009;27:6546-9.
- Ogokeh CE, Campbell AP, Feldstein LR, Weinberg GA, Staat MA, McNeal MM, et al. Comparison of Parental Report of Influenza Vaccination to Documented Records in Children Hospitalized With Acute Respiratory Illness, 2015-2016. Journal of the Pediatric Infectious Diseases Society. 2021;10:389-97.
- Santibanez TA, Srivastav A, Zhai Y, Singleton JA. Trends in Childhood Influenza Vaccination Coverage, United States, 2012-2019. Public health reports (Washington, DC : 1974). 2020;135:640-9.
- Recommendations from the National Vaccine Advisory committee: standards for adult immunization practice. Public health reports (Washington, DC : 1974). 2014;129:115-23.