Antimicrobial Resistance, Food, and Food Animals
Antimicrobial Resistance
Antimicrobial resistance happens when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. That means the germs are not killed and continue to grow. Some food poisoning is caused by antimicrobial-resistant bacteria.

Antimicrobial Resistance and Food Poisoning
The American food supply is among the safest in the world, but people can still get food poisoning by eating contaminated foods. Some of the bacteria that cause food poisoning are antimicrobial resistant—meaning certain medicines do not work against the bacteria.
Antibiotic and antifungal drugs save lives, but their use can contribute to the development of resistant germs. Antimicrobial resistance spreads between people, animals, and the environment (for example, in water and soil). Stopping the development and spread of antimicrobial resistance is a key action to protect people, along with preventing infections and improving antibiotic and antifungal use.
Learn what CDC is doing to help stop antimicrobial-resistant foodborne infections and how you can protect yourself and your family.
Food Poisoning Symptoms
A person with a foodborne infection caused by antimicrobial-resistant bacteria will have similar symptoms to infections caused by bacteria that can be killed by antibiotics. Symptoms can be mild to life-threatening.
People with mild symptoms of food poisoning usually do not need antibiotics to get better.
Mild symptoms may include:
- Nausea
- Diarrhea
- Vomiting
- Stomach pain or cramps
- Fever
People with a severe infection may need to see a doctor, be prescribed antibiotics, or be hospitalized. Resistant infections can be difficult, and sometimes impossible, to treat. This can lead to more costly treatments and higher risks for side effects.
Severe symptoms include:
- Bloody diarrhea
- High fever (temperature over 102°F, measured by mouth)
- Frequent vomiting that prevents keeping liquids down (which can lead to dehydration)
- Signs of dehydration, including little or no urination, a very dry mouth and throat, or feeling dizzy when standing up
- Diarrhea that lasts more than 3 days
Who Is at Higher Risk for Food Poisoning
Anyone can get food poisoning, but certain groups of people are more likely to get very sick from food poisoning. If you have one of these factors, your body may not be able to fight germs and sickness as effectively: aged 65 or older, younger than 5, weakened immune system, or pregnancy. These groups are at risk for severe symptoms or complications from food poisoning, including infections caused by antimicrobial-resistant bacteria.
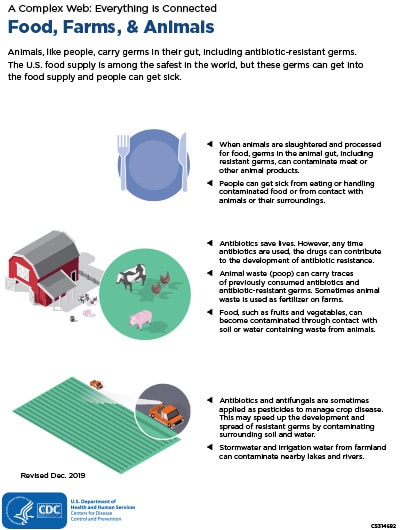
How Antimicrobial-Resistant Bacteria Can Spread to People Through Food or Animal Contact
Animals, like people, carry bacteria in their guts. This includes antimicrobial-resistant germs, which can get in food in several ways:
- When animals are slaughtered and processed for food, antimicrobial-resistant bacteria can contaminate meat or other animals products, for example, by spreading from contaminated processing equipment or storage bins.
- Animal feces/excrement (poop) can contain resistant bacteria and get into the surrounding environment.
- Fruits and vegetables can get contaminated through contact with soil, water, or fertilizer that contains animal feces/excrement.
People can get intestinal infections, including antimicrobial-resistant infections, by handling or eating contaminated food, or coming in contact with untreated or uncomposted animal poop. People can come in contact with animal poop either through direct contact with animals and animal environments or through contaminated drinking or swimming water. Infections can also spread between people.
In recent years, CDC has investigated many multistate outbreaks caused by antimicrobial-resistant bacteria. These outbreaks have been linked to contaminated food and contact with farm animals, pets, and pet food, and treats.
Protect Yourself and Your Family
When preparing food, follow the four steps to food safety:
- Clean. Wash your hands before and after touching raw meat, chicken and other poultry, seafood, or eggs. Wash your countertops, cutting boards, and utensils after preparing each food item.
- Separate. Germs from raw meat, poultry, seafood, and eggs can spread to fruits, vegetables, and other ready-to-eat foods unless you keep them separate. Use one cutting board or plate for raw meat and another for food that will not be cooked before it’s eaten. Don’t put cooked meat on a plate that had raw meat on it.
- Cook. Use a food thermometer to make sure food is cooked to a safe internal temperature:
- 145°F for whole cuts of beef, pork, lamb, and veal, such as steaks, chops, and roasts (then allow meat to rest for 3 minutes before carving or eating)
- 160°F for ground meats, such as beef and pork, and egg dishes
- 165°F for poultry, including ground chicken and turkey
- Get safe cooking temperatures for other foods
- Chill. Keep your refrigerator at 40°F or below and refrigerate food within 2 hours of cooking. Refrigerate within 1 hour if food is exposed to temperatures above 90°F (like a hot car or picnic).
When around pets and other animals:
- Wash your hands after touching them, their food, water, poop, belongings (such as toys and bowls), or habitats (such as beds, cages, tanks, coops, stalls, and barns).
If you think you got sick from food, report it to your local health department.
Review CDC’s Travelers’ Health recommendations when preparing for international travel.
Learn other steps you can take to reduce your risk of getting infections, help stop the spread of germs, and combat antimicrobial resistance.
What CDC Is Doing
CDC leads the U.S. public health response to combat antimicrobial resistance. CDC’s Antimicrobial Resistance (AR) Solutions Initiative invests in national infrastructure to detect, respond to, contain, and prevent resistant infections, including in the food supply. Efforts include:
- Tracking antimicrobial-resistant infections and studying how resistance emerges and spreads.
- Detecting and investigating outbreaks of antimicrobial-resistant infections quickly to identify their sources and stop their spread.
- Determining the sources of antimicrobial-resistant infections that are commonly spread through food and animals.
- Strengthening the ability of state and local health departments to detect, respond to, and report antimicrobial-resistant infections.
- Educating the public and food workers on prevention methods, including safe food handling, safe contact with animals, and proper handwashing.
- Ensuring veterinarians, livestock and poultry producers, and other animal industries such as aquaculture have tools, information, and training around the appropriate use of antibiotic and antifungal drugs.
- Supporting the important work that the U.S. Food and Drug Administration and U.S. Department of Agriculture are doing to improve antibiotic and antifungal drug use in veterinary medicine and agriculture.
- AMD and One Health: Responding to a Multistate, Multidrug-Resistant Disease Outbreak
- Sick Kids, Dairy Calves, and Antibiotics That Don’t Work: Dr. Megin Nichols’s Story
- Whole-genome Sequencing and the Race Against Antimicrobial Resistance
- National Antimicrobial Resistance Monitoring System (NARMS)
- Antibiotic Resistance Threats in the United States, 2019
- Video: Antibiotic Resistance and Food