Association of vaccine hesitancy with maternal influenza and Tdap vaccination coverage – United States, 2019–20 to 2022–23
Vaccinating pregnant women with influenza vaccine and tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) can reduce the risk of influenza and pertussis infection for themselves and their infants. However, during the 2022–23 influenza season, less than half of women received influenza vaccine (47.2%) and only 55.4% received Tdap during pregnancy [1]. Vaccine hesitancy has been found to be negatively associated with vaccination, leaving pregnant women and their infants at increased risk of influenza and pertussis [2-3]. CDC analyzed data from Internet panel surveys of pregnant women conducted in April 2020, March-April 2021, March-April 2022, and March-April 2023 to examine the association between vaccine hesitancy and vaccination coverage among pregnant women and any differences among demographic subgroups during this time period. Women who were not hesitant towards influenza vaccine were approximately twice as likely to be vaccinated against influenza compared with hesitant women, and women not hesitant towards Tdap were approximately 2.5 times more likely to receive Tdap across the study period. While self-reported hesitancy towards influenza and Tdap vaccination during pregnancy increased among pregnant women from 2019–20 to 2022–23, Tdap vaccination coverage in 2022–23 was similar to coverage in 2019–20; the increase in hesitancy may have been offset by the increase in coverage among non-hesitant women. Influenza vaccination coverage decreased from 2019–20 to 2022–23 among women both hesitant and non-hesitant towards influenza vaccine, suggesting factors in addition to hesitancy contributed to the decrease. Although hesitant women were less likely to be vaccinated, provider offers or referrals for vaccination are associated with greater likelihood of vaccination and could decrease the effect of hesitancy on vaccination coverage.
Data from Internet panel surveys of pregnant and recently pregnant women aged 18–49 years conducted in April 2020, March-April 2021, March-April 2022, and March-April 2023 were analyzed. Survey methodology has been previously described [4]. For influenza vaccination hesitancy and coverage assessment, data were limited to women who were pregnant at any time during the peak influenza vaccination period of a given influenza season, from October 1 to January 31, and had known influenza vaccination status. Women who received an influenza vaccine before or during pregnancy since July 1 of the season of interest were considered vaccinated. Tdap hesitancy and vaccination coverage assessment were restricted to women who were pregnant at any time since August 1, had a live birth by their survey date, and were aware of their Tdap vaccination status. Tdap vaccination was defined as receipt of Tdap at any time during a respondent’s recent pregnancy.
Hesitancy towards influenza and Tdap vaccination was assessed for all survey participants by the questions “Overall, how hesitant are you about flu vaccination during your pregnancy?” and “Overall, how hesitant are you about Tdap vaccination during your pregnancy?” For bivariate analyses, those who responded “Very hesitant” and “Somewhat hesitant” were considered “Hesitant” and those who responded “Not that hesitant” and “Not at all hesitant” were considered “Not hesitant.” Proportions were calculated for influenza and Tdap vaccination coverage among hesitant and non-hesitant pregnant women. Differences between groups and between survey years were determined using pairwise comparisons and t-tests with significance set at p<0.05. Prevalence ratios were calculated to measure the association of vaccine hesitancy and vaccination coverage overall and within groups. Proportions were also calculated for receipt of a provider offer or referral for influenza and Tdap vaccination by hesitancy status. SAS-callable SUDAAN software (version 11.0.4; RTI International) was used to conduct all analyses.
Results
- Influenza vaccination coverage decreased from 57.5% in 2019–20 to 47.2% in 2022–23, while the percent of women reporting hesitancy towards influenza vaccination increased from 46.7% in 2019–20 to 59.5% in 2022–23 (Figure 1).
- Influenza vaccination coverage decreased among both hesitant and non-hesitant women.
- Tdap vaccination coverage was similar in 2019–20 (53.8%) and 2022–23 (55.4%), though coverage decreased between 2020–21 and 2021–22, while the percent of women reporting hesitancy towards Tdap increased from 31.1% in 2019–20 to 43.1% in 2022–23.
- Tdap vaccination coverage increased among non-hesitant women from 2019–20 to 2022–23; Tdap vaccination coverage among hesitant women was similar in 2019–20 and 2022–23.
Figure 1. Trends in influenza vaccine* and tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap)† hesitancy§ and coverage among pregnant women – Internet panel survey, United States, 2019–20 through 2022–23 influenza seasons
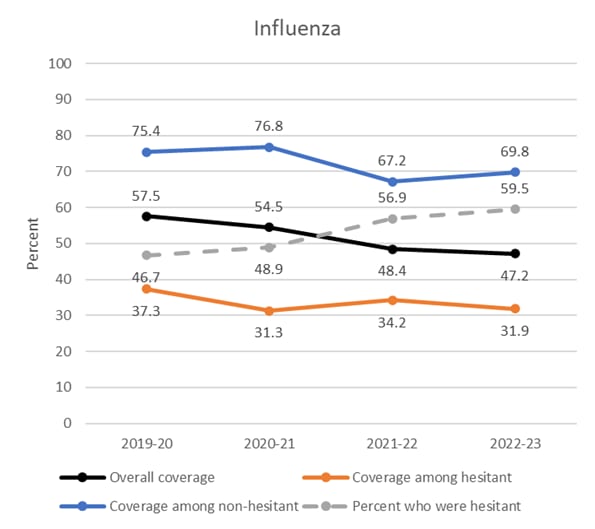
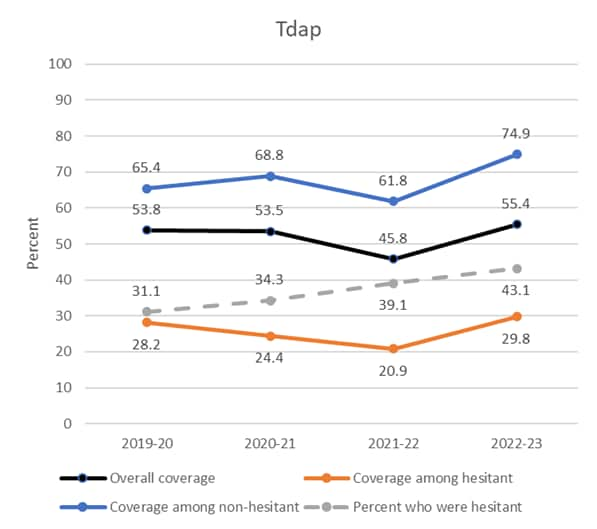
* Respondents pregnant anytime during October–January of the influenza season at the time of interview (April 2020, March-April 2021, March-April 2022, or March-April 2023) and with known influenza vaccination status were included in the analyses to assess influenza vaccination hesitancy and coverage for the 2019–20, 2020–21, 2021–22, and 2022–23 influenza seasons (N=1,841 in 2019-20, N=1,795 in 2020-21, N=2,015 in 2021-22, and N=1,814 in 2022-23). Women who reported receiving an influenza vaccination since July 1st of the year prior to their interview, before or during their pregnancy, were considered vaccinated. The reported percent of women hesitant about influenza vaccination is different from previously reported estimates [1] because this analysis was limited to the sample used for coverage assessment rather than all women who responded to the hesitancy question.
† Respondents who delivered a live birth since August 1st of the year prior to their interview and had known Tdap vaccination status were included in the analyses to assess Tdap vaccination hesitancy and coverage during the 2019–20, 2020–21, 2021–22, and 2022–23 influenza seasons (N=463 in 2019-20, N=729 in 2020-21, N=838 in 2021-22, and N=776 in 2022-23). Women who reported receiving a Tdap vaccination during their pregnancy were considered vaccinated. The reported percent of women hesitant about Tdap vaccination is different from estimates reported elsewhere [1] because this analysis was limited to the sample used for coverage assessment rather than all women who responded to the hesitancy question.
§ Respondents were asked the following questions, “Overall, how hesitant are you about flu vaccination during your pregnancy?” and “Overall, how hesitant are you about Tdap vaccination during your pregnancy?” [1. Not at all hesitant, 2. Not that hesitant, 3. Somewhat hesitant, 4. Very hesitant]. “Very hesitant” and “Somewhat hesitant” were considered “Hesitant” and “Not that hesitant” and “Not at all hesitant” were considered “Not hesitant.”
- Women who were not hesitant towards influenza vaccine were approximately 2 to 2.5 times as likely to be vaccinated against influenza compared with hesitant women (Prevalence Ratio (PR) =2.18 in 2022–23) (Table 1).
- This relationship remained consistent across the study period and in most demographic subgroups (e.g., White non-Hispanic and Black non-Hispanic adults, those with public or private insurance).
- However, even among women hesitant towards influenza vaccination, 45%–53% were vaccinated if they received an offer or referral for vaccination from a healthcare provider. In comparison, only 5.6–9.4% of hesitant women were vaccinated if they did not receive an offer, referral, or recommendation for vaccination from a healthcare provider.
- Among women hesitant about influenza vaccination, vaccination coverage decreased from 2019–20 through 2022–23 among women aged 35–49 years, those living in rural areas or the South, Hispanic women, women who received an offer or referral from a provider for influenza vaccination, those with at least one high-risk condition for influenza, and those with more than ten provider visits since July of the respective influenza season.
- The decrease in coverage among non-hesitant women occurred primarily in non-Hispanic White women.
Table 1. Influenza* vaccination coverage among pregnant women, by hesitancy† and selected characteristics – Internet panel survey, United States, 2019–20 through 2022–23 influenza seasons
| 2019–20 | 2020–21 | 2021–22 | 2022–23 | |||||||||
| Vaccine hesitant
(N=883)§ |
Not vaccine hesitant
(N=956)§ |
Vaccine hesitant
(N=911)§ |
Not vaccine hesitant
(N=882)§ |
Vaccine hesitant
(N=1,145)§ |
Not vaccine hesitant
(N=870)§ |
Vaccine hesitant
(N=1,063)§ |
Not vaccine hesitant
(N=749)§ |
|||||
| Weighted % Vaccinated (95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Prevalence Ratio
(95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Prevalence Ratio
(95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Prevalence Ratio
(95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Prevalence Ratio
(95% CI)¶ |
|
| Overall | 37.3
(33.5–41.3) |
75.4
(71.5–79.0) |
2.02
(1.80–2.26) |
31.3
(27.6–35.2)** |
76.8
(71.4–81.7) |
2.45
(2.14–2.81) |
34.2
(30.0–38.5) |
67.2
(62.8–71.4)** |
1.97
(1.72–2.25) |
31.9
(28.4–35.6)** |
69.8
(65.2–74.1) |
2.18
(1.92–2.48) |
| Age group (years) | ||||||||||||
| 18–24 | 29.9
(23.6–36.8) |
64.2
(55.7–72.1) |
2.15
(1.67–2.75) |
29.2
(23.4–35.6) |
70.1
(58.8–79.8) |
2.40
(1.87–3.08) |
37.7
(26.7–49.7) |
57.4
(47.2–67.2) |
1.52
(1.09–2.13) |
31.0
(22.6–40.4) |
55.2
(42.9–67.2) |
1.78
(1.26–2.53) |
| 25–34 | 35.7
(30.2–41.5) |
78.8
(73.6–83.5) |
2.21
(1.87–2.61) |
30.6
(25.3–36.2) |
79.5
(71.0–86.4) |
2.60
(2.14–3.17) |
31.7
(27.4–36.4) |
71.1
(65.5–76.3)** |
2.24
(1.91–2.62) |
32.5
(27.7–37.4) |
71.7
(66.0–76.9) |
2.21
(1.87–2.60) |
| 35–49 | 50.6
(42.0–59.1) |
77.9
(68.3–85.7) |
1.54
(1.27–1.87) |
36.2
(25.5–48.0)** |
76.6
(67.7–84.0) |
2.12
(1.56–2.86) |
38.4
(29.2–48.3) |
68.7
(59.6–76.9) |
1.79
(1.37–2.34) |
31.8
(26.3–37.6)** |
79.9
(72.6–86.0) |
2.52
(2.08–3.05) |
| Race and ethnicity†† | ||||||||||||
| White, non-Hispanic | 32.3
(27.3–37.6) |
80.5
(76.1–84.4) |
2.49
(2.12–2.93) |
27.5
(22.3–33.3) |
76.9
(69.9–82.9) |
2.80
(2.26–3.46) |
30.7
(26.4–35.3) |
66.4
(60.5–71.9)** |
2.16
(1.83–2.55) |
30.6
(26.4–35.1) |
67.8
(61.3–73.9)** |
2.21
(1.87–2.62) |
| Black, non-Hispanic | 30.4
(22.7–39.0) |
60.0
(46.5–72.5) |
1.97
(1.40–2.77) |
24.7
(17.5–33.0) |
—§§ | —§§ | —§§ | 63.5
(49.9–75.6) |
—§§ | 29.2
(18.8–41.5) |
62.0
(48.9–74.0) |
2.12
(1.40–3.23) |
| Hispanic | 51.0
(41.4–60.6) |
73.0
(63.8–81.0) |
1.43
(1.15–1.77) |
47.4
(39.3–55.6) |
78.9
(70.0–86.2) |
1.67
(1.37–2.02) |
43.6
(36.1–51.4) |
69.7
(61.3–77.2) |
1.60
(1.30–1.96) |
36.5
(29.6–43.9)** |
74.5
(65.5–82.2) |
2.04
(1.64–2.54) |
| Other, non-Hispanic | 50.5
(35.4–65.4) |
78.9
(66.2–88.5) |
1.56
(1.15–2.13) |
—§§ | 87.1
(76.4–94.1) |
—§§ | —§§ | —§§ | —§§ | 33.7
(21.0–48.5) |
—§§ | —§§ |
| Education | ||||||||||||
| High school diploma or less | 23.9
(17.6–31.2) |
64.1
(54.9–72.6) |
2.68
(1.98–3.63) |
30.2
(23.2–38.0) |
71.5
(60.7–80.7) |
2.37
(1.81–3.10) |
35.8
(26.8–45.5)** |
61.6
(52.4–70.2) |
1.72
(1.29–2.30) |
25.8
(19.5–32.9) |
59.5
(50.2–68.4) |
2.31
(1.73–3.09) |
| Some college, no degree | 26.8
(18.8–36.1) |
63.5
(52.5–73.6) |
2.3
(1.67–3.36) |
18.4
(11.6–26.9) |
—§§ | —§§ | 33.1
(24.2–43.0) |
68.3
(60.1–75.7) |
2.06
(1.54–2.77) |
25.4
(19.4–32.2) |
60.2
(49.8–70.0) |
2.37
(1.77–3.17) |
| College degree | 44.2
(37.7–51.0) |
81.9
(75.5–87.3) |
1.85
(1.58–2.18) |
37.5
(30.4–45.0) |
78.2
(70.3–84.8) |
2.09
(1.69–2.58) |
29.7
(24.5–35.2)** |
65.6
(58.1–72.7)** |
2.21
(1.80–2.72) |
37.6
(31.0–44.6) |
76.2
(67.7–83.4) |
2.02
(1.65–2.48) |
| Greater than college degree | 54.5
(43.7–64.9) |
82.6
(74.9–88.7) |
1.52
(1.24–1.86) |
31.9
(23.0–41.9)** |
86.4
(79.6–91.6) |
2.71
(2.03–3.62) |
47.2
(34.5–60.3) |
79.6
(65.3–89.9) |
1.68
(1.25–2.27) |
48.9
(39.3–58.6) |
85.3
(77.5–91.2) |
1.74
(1.42–2.14) |
| Employment status | ||||||||||||
| Working | 44.0
(38.8–49.3) |
78.5
(73.4–83.0) |
1.78
(1.56–2.03) |
39.4
(34.1–44.9) |
79.9
(72.4–86.1) |
2.03
(1.74–2.37) |
38.0
(33.0–43.2) |
69.4
(64.2–74.2)** |
1.83
(1.57–2.12) |
37.7
(33.1–42.3) |
72.1
(66.8–77.0) |
1.92
(1.67–2.20) |
| Not working | 26.5
(20.9–32.6) |
69.5
(63.0–75.5) |
2.63
(2.08–3.32) |
20.8
(15.7–26.7) |
70.6
(62.5–77.9) |
3.40
(2.58–4.47) |
26.1
(19.1–34.1) |
62.0
(53.1–70.4) |
2.38
(1.75–3.23) |
21.9
(16.4–28.2) |
63.4
(53.7–72.4) |
2.90
(2.16–3.89) |
| Poverty status¶¶ | ||||||||||||
| At or above poverty | 40.9
(36.3–45.6) |
79.4
(75.3–83.1) |
1.94
(1.72–2.19) |
35.4
(30.7–40.3) |
78.0
(71.7–83.5) |
2.20
(1.90–2.56) |
35.9
(31.7–40.3) |
69.1
(64.2–73.6)** |
1.92
(1.68–2.20) |
38.5
(34.1–43.0) |
73.3
(68.2–78.0) |
1.91
(1.67–2.18) |
| Below poverty | 27.2
(20.0–35.4) |
60.0
(49.6–69.7) |
2.21
(1.61–3.02) |
18.8
(12.9–26.0) |
72.0
(58.5–83.1) |
3.83
(2.64–5.54) |
29.3
(19.4–41.0) |
58.5
(47.4–68.9) |
1.99
(1.34–2.95) |
20.5
(15.1–26.8) |
57.4
(47.0–67.4) |
2.80
(2.03–3.87) |
| Area of residence*** | ||||||||||||
| Rural | 34.6
(25.3–44.9) |
78.4
(68.4–86.5) |
2.27
(1.69–3.04) |
26.4
(17.0–37.8) |
82.6
(70.8–91.1) |
3.13
(2.12–4.61) |
23.7
(15.5–33.6) |
60.4
(48.5–71.4)** |
2.55
(1.70–3.83) |
22.3
(16.6–28.8)** |
68.4
(56.9–78.5) |
3.07
(2.26–4.16) |
| Non-rural | 37.9
(33.7–42.2) |
75.0
(70.7–78.9) |
1.98
(1.75–2.24) |
32.1
(28.1–36.4) |
76.0
(69.9–81.3) |
2.36
(2.04–2.74) |
36.1
(31.4–40.9) |
68.3
(63.5–72.8)** |
1.90
(1.64–2.19) |
34.3
(30.2–38.6) |
70.0
(64.9–74.8) |
2.04
(1.77–2.35) |
| Region††† | ||||||||||||
| Northeast | 38.9
(30.1–48.2) |
73.8
(64.6–81.6) |
1.90
(1.48–2.44) |
42.8
(32.7–53.4) |
81.4
(72.7–88.3) |
1.90
(1.48–2.44) |
43.5
(31.5–56.1) |
72.4
(61.8–81.4) |
1.66
(1.23–2.25) |
35.7
(26.5–45.7) |
75.8
(65.9–84.0) |
2.12
(1.60–2.82) |
| Midwest | 28.8
(20.9–37.9) |
78.4
(69.1–85.9) |
2.72
(2.01–3.68) |
28.1
(20.1–37.3) |
85.7
(77.2–92.0) |
3.05
(2.25–4.13) |
29.0
(21.1–37.9) |
68.3
(57.7–77.6) |
2.35
(1.73–3.21) |
32.7
(25.1–41.2) |
68.4
(58.5–77.1) |
2.09
(1.59–2.74) |
| South | 39.8
(33.6–46.2) |
72.0
(65.1–78.2) |
1.81
(1.51–2.16) |
28.1
(22.6–34.1)** |
66.9
(56.7–76.0) |
2.38
(1.87–3.03) |
29.7
(24.3–35.4)** |
66.5
(59.6–72.9) |
2.24
(1.82–2.75) |
30.8
(25.2–36.9)** |
67.6
(59.8–74.7) |
2.19
(1.77–2.71) |
| West | 39.7
(30.8–49.0) |
79.3
(70.6–86.4) |
2.00
(1.57–2.54) |
32.4
(23.8–41.9) |
82.9
(70.5–91.6) |
2.56
(1.90–3.45) |
39.4
(31.0–48.3) |
64.5
(54.6–73.6)** |
1.64
(1.27–2.11) |
30.4
(23.2–38.4) |
69.6
(58.6–79.2) |
2.29
(1.73–3.04) |
| Prenatal insurance coverage§§§ | ||||||||||||
| Private/military insurance only | 39.3
(33.3–45.6) |
81.9
(76.3–86.6) |
2.08
(1.77–2.46) |
33.2
(26.9–40.0) |
78.9
(70.6–85.7) |
2.38
(1.93–2.93) |
31.5
(26.1–37.3) |
73.5
(66.7–79.6)** |
2.33
(1.93–2.82) |
34.5
(29.3–39.9) |
78.1
(71.4–84.0) |
2.27
(1.91–2.69) |
| Any public insurance | 37.3
(31.8–43.0) |
67.5
(61.2–73.5) |
1.81
(1.52–2.15) |
30.6
(25.5–36.0) |
77.3
(69.2–84.0)** |
2.53
(2.09–3.06) |
36.7
(30.6–43.0) |
62.2
(56.0–68.2) |
1.70
(1.40–2.05) |
30.0
(25.1–35.2) |
64.6
(58.0–70.8) |
2.15
(1.78–2.60) |
| No insurance | 27.5
(15.1–43.1) |
—§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ |
| Provider vaccination recommendation/ offer¶¶¶ | ||||||||||||
| Offered or referred | 52.5
(47.2–57.8) |
84.0
(79.9–87.6) |
1.60
(1.44–1.78) |
45.6
(40.2–51.1) |
85.1
(81.5–88.2) |
1.87
(1.65–2.11) |
48.1
(42.6–53.6) |
77.6
(72.9–81.8)** |
1.61
(1.43–1.83) |
45.1
(40.3–50.0)** |
81.0
(76.6–84.9) |
1.79
(1.60–2.02) |
| Recommended, no offer or referral | 25.4
(13.8–40.2) |
72.2
(56.0–85.0) |
2.85
(1.68–4.83) |
—§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ |
| No recommendation | 9.4
(5.5–14.9) |
31.2
(20.5–43.5) |
3.30
(1.85–5.91) |
5.6
(2.9–9.5) |
—§§ | —§§ | 9.2
(5.2–14.7) |
20.2
(12.8–29.4) |
2.20
(1.18–4.09) |
7.8
(4.7–11.9) |
19.3
(10.6–31.0) |
2.48
(1.28–4.80) |
| Number of provider visits since July 1st | ||||||||||||
| None | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ | —§§ |
| 1–5 | 28.1
(21.2–35.8) |
64.5
(54.7–73.5) |
2.30
(1.73–3.06) |
25.4
(17.7–34.4) |
—§§ | —§§ | 35.9
(25.4–47.5) |
52.4
(42.0–62.6) |
1.46
(1.03–2.08) |
33.3
(27.9–39.1) |
65.8
(57.9–73.2) |
1.97
(1.62–2.41) |
| 6–10 | 40.3
(33.9–47.0) |
79.1
(73.1–84.3) |
1.96
(1.65–2.33) |
32.5
(26.0–39.5) |
79.6
(73.2–85.1) |
2.45
(1.98–3.03) |
36.0
(30.2–42.1) |
66.8
(59.6–73.4)** |
1.86
(1.54–2.24) |
36.2
(28.1–45.0) |
75.2
(65.7–83.2) |
2.08
(1.61–2.67) |
| >10 | 43.2
(36.2–50.3) |
78.4
(72.1–83.9) |
1.82
(1.52–2.16) |
33.3
(27.5–39.5)** |
79.9
(73.3–85.5) |
2.40
(1.99–2.90) |
32.5
(26.7–38.6)** |
75.2
(68.7–81.0) |
2.32
(1.91–2.82) |
27.6
(22.0–33.8)** |
71.4
(63.6–78.4) |
2.58
(2.05–3.25) |
| High-risk condition for influenza**** | ||||||||||||
| Yes | 44.4
(38.1–50.9) |
76.9
(70.9–82.2) |
1.73
(1.48–2.03) |
38.4
(31.3–45.8) |
75.8
(67.3–83.0) |
1.97
(1.60–2.44) |
39.8
(32.7–47.2) |
69.4
(62.6–75.7) |
1.75
(1.43–2.13) |
36.0
(30.8–41.5)** |
69.0
(62.4–75.0) |
1.91
(1.61–2.27) |
| No | 31.7
(26.3–37.5) |
75.4
(69.4–80.8) |
2.38
(1.98–2.86) |
27.0
(22.0–32.4) |
77.5
(67.9–85.3) |
2.87
(2.31–3.57) |
31.1
(25.8–36.8) |
65.7
(59.6–71.4)** |
2.11
(1.74–2.56) |
25.6
(21.4–30.1) |
69.9
(62.9–76.2) |
2.73
(2.26–3.31) |
Abbreviations: CI: Confidence Interval.
* Respondents pregnant anytime during October–January of the influenza season at the time of interview (April 2020, March-April 2021, March-April 2022, or March-April 2023) and with known influenza vaccination status were included in the analyses to assess influenza vaccination coverage for the 2019–20, 2020–21, 2021–22, and 2022–23 influenza seasons. Women who reported receiving an influenza vaccination since July 1st of the year prior to their interview, before or during their pregnancy, were considered vaccinated.
† Respondents were asked the following question, “Overall, how hesitant are you about flu vaccination during your pregnancy?” [1. Not at all hesitant, 2. Not that hesitant, 3. Somewhat hesitant, 4. Very hesitant]. “Very hesitant” and “Somewhat hesitant” were considered “Hesitant” and “Not that hesitant” and “Not at all hesitant” were considered “Not hesitant.”
§ The total unweighted number of respondents in the sample.
¶ Korn-Graubard 95% confidence interval.
** Estimate is statistically different from 2019–20.
†† Race and ethnicity was self-reported. Respondents identified as Hispanic might be of any race. The “Other” race category included Asians, American Indians/Alaska Natives, Native Hawaiians or other Pacific Islanders, and women who selected “other” or multiple races; the “other” response option was removed from the survey in 2023.
§ Estimate does not meet the NCHS standards of reliability. https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf
¶¶ Poverty status was defined based on the reported number of persons living in the household and annual household income, according to U.S. Census poverty thresholds. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html
*** Rurality was defined using ZIP codes where >50% of the population resides in a nonmetropolitan county, a rural U.S. Census tract, or both, according to the Health Resources and Services Administration’s definition of rural population. https://www.hrsa.gov/rural-health/about-us/definition/index.html
††† Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin. South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
§§ Respondents pregnant on their survey date were asked what medical insurance or medical care coverage they had; respondents who had already delivered were asked what they had during their most recent pregnancy. Women considered to have public insurance selected at least one of the following: Medicaid, Medicare, state-sponsored medical plan, or other government plan. Respondents considered to have private/military insurance selected private medical insurance and/or military medical care and did not select any type of public insurance.
¶¶¶ Excluded women from influenza vaccination analyses who did not report having a provider visit since July in the year prior to the interview (n=24 in 2020, n=7 in 2021, n=12 in 2022, and n=27 in 2023).
**** Conditions other than pregnancy associated with increased risk for serious medical complications of influenza include chronic asthma, a lung condition other than asthma, a heart condition, diabetes, a kidney condition, a liver condition, obesity, sickle cell or other anemia, a neurological or neuromuscular condition, or a weakened immune system. Women who were missing information were excluded from analysis (n=233 in 2020, n=274 in 2021, n=63 in 2022, n=78 in 2023).
- Women who were not hesitant towards Tdap were approximately 2.5 to 3 times as likely to be vaccinated with Tdap compared with hesitant women (PR=2.51 in 2022–23) (Table 2).
- This relationship remained consistent across the study period.
- The relationship was similar in most demographic subgroups, but for most years the association between hesitancy and Tdap vaccination was smallest among women who received an offer or referral for Tdap vaccination from a provider (PR=1.76 in 2022–23).
- 37%–46% of hesitant women who received a provider offer or referral were vaccinated.
- Among non-hesitant women, Tdap vaccination coverage increased from 2019–20 to 2022–23 among women ages 35–49 years, those living below the poverty line, those living in the South, and those with private or public insurance.
- No changes in Tdap coverage were observed among demographic subgroups of hesitant women.
Table 2. Tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap)* vaccination coverage among pregnant women, by hesitancy† and selected characteristics – Internet panel survey, United States, 2019-20 through 2022–23 influenza seasons
| 2019–20 | 2020–21 | 2021–22 | 2022–23 | |||||||||
| Vaccine hesitant
(N=143)§ |
Not vaccine hesitant
(N=320)§ |
Vaccine hesitant
(N=250)§ |
Not vaccine hesitant
(N=478)§ |
Vaccine hesitant
(N=346)§ |
Not vaccine hesitant
(N=492)§ |
Vaccine hesitant
(N=332)§ |
Not vaccine hesitant
(N=444)§ |
|||||
| Weighted % Vaccinated (95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Prevalence Ratio
(95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Prevalence Ratio
(95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Prevalence Ratio
(95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Weighted % Vaccinated (95% CI)¶ |
Prevalence Ratio
(95% CI)¶ |
|
| Overall | 28.2
(20.5–37.0) |
65.4
(59.3–71.1) |
2.32
(1.72–3.12) |
24.4
(18.7–30.7) |
68.8
(64.0–73.3) |
2.82
(2.21–3.62) |
20.9
(16.3–26.3) |
61.8
(56.8–66.6) |
2.95
(2.31–3.77) |
29.8
(24.1–35.9) |
74.9
(69.9–79.5)** |
2.51
(2.05–3.08) |
| Age group (years) | ||||||||||||
| 18–24 | —†† | 63.4
(49.3–76.0) |
—†† | 20.4
(11.4–32.2) |
59.1
(48.4–69.3) |
2.90
(1.74–4.83) |
26.9
(15.7–40.8) |
48.6
(37.1–60.3) |
1.81
(1.10–2.98) |
—†† | 62.1
(48.2–74.7) |
—†† |
| 25–34 | 34.7
(23.4–47.5) |
68.0
(59.8–75.5) |
1.96
(1.38–2.78) |
25.8
(18.1–34.7) |
74.6
(68.2–80.2) |
2.89
(2.10–3.98) |
20.4
(14.2–27.9)** |
69.0
(62.4–75.0) |
3.38
(2.42–4.73) |
28.0
(20.5–36.5) |
75.4
(68.7–81.3) |
2.70
(2.02–3.59) |
| 35–49 (Ref) | —†† | 58.6
(45.4–71.1) |
—†† | —†† | 59.6
(48.5–70.0) |
—†† | 15.7
(9.5–23.7) |
51.7
(41.1–62.3) |
3.30
(2.06–5.30) |
25.9
(17.5–36.0) |
87.3
(79.7–92.9)** |
3.37
(2.38–4.77) |
| Race and ethnicity§§ | ||||||||||||
| White, non-Hispanic (Ref) | 36.8
(25.8–48.8) |
76.2
(69.8–81.9) |
2.07
(1.52–2.83) |
24.3
(16.9–33.0) |
77.0
(71.7–81.8) |
3.17
(2.30–4.38) |
23.9
(17.7–31.1)** |
61.8
(55.6–67.8)** |
2.59
(1.94–3.45) |
31.8
(25.2–39.0) |
82.2
(77.3–86.5) |
2.59
(2.08–3.22) |
| Black, non-Hispanic | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† |
| Hispanic | —†† | —†† | —†† | 31.8
(18.7–47.4) |
57.6
(45.6–68.9) |
1.81
(1.13–2.90) |
19.8
(9.8–33.6) |
64.2
(53.3–74.2) |
3.25
(1.81–5.83) |
29.1
(16.9–43.9) |
70.6
(57.2–81.7) |
2.43
(1.52–3.89) |
| Other, non-Hispanic | —†† | —†† | —†† | —†† | 77.9
(63.3–88.7) |
—†† | —†† | —†† | —†† | —†† | —†† | —†† |
| Education | ||||||||||||
| High school diploma or less | —†† | 52.0
(39.7–64.1) |
—†† | 22.9
(13.9–34.2) |
65.4
(54.3–75.3) |
2.85
(1.82–4.48) |
27.6
(18.2–38.7) |
54.9
(44.7–64.9) |
1.99
(1.34–2.96) |
26.7
(18.4–36.5) |
62.8
(52.5–72.2) |
2.35
(1.64–3.36) |
| Some college, no degree | —†† | 71.6
(55.1–84.8) |
—†† | 32.5
(19.9–47.2) |
71.5
(60.9–80.6) |
2.20
(1.44–3.36) |
20.5
(11.6–32.0) |
70.1
(60.2–78.7) |
3.43
(2.10–5.58) |
24.1
(13.7–37.4) |
85.0
(75.6–91.8) |
3.52
(2.19–5.65) |
| College degree | 31.4
(19.2–45.9) |
72.9
(62.9–81.4) |
2.32
(1.52–3.55) |
16.4
(8.6–27.3) |
73.2
(65.4–80.0) |
4.45
(2.60–7.63) |
15.9
(8.8–25.4)** |
60.7
(51.8–69.1)** |
3.82
(2.29–6.37) |
37.8
(27.3–49.2) |
75.1
(65.3–83.3) |
1.99
(1.47–2.68) |
| Greater than college degree (Ref) | —†† | 65.3
(50.3–78.3) |
—†† | —†† | 59.2
(46.8–70.8) |
—†† | —†† | 62.4
(48.4–75.0) |
—†† | —†† | 81.1
(68.2–90.4) |
—†† |
| Employment status | ||||||||||||
| Working (Ref) | 28.5
(18.2–40.7) |
62.9
(54.8–70.6) |
2.21
(1.48–3.29) |
20.1
(12.9–28.9) |
65.7
(58.7–72.2) |
3.27
(2.21–4.85) |
19.3
(13.8–25.9) |
56.0
(49.6–62.3) |
2.90
(2.10–4.00) |
28.4
(21.2–36.4) |
72.2
(65.1–78.5) |
2.54
(1.93–3.34) |
| Not working | 27.9
(16.7–41.5) |
69.1
(59.5–77.7) |
2.48
(1.59–3.86) |
28.3
(20.0–37.8) |
72.0
(65.1–78.2) |
2.55
(1.86–3.49) |
24.5
(16.1–34.5) |
72.0
(64.0–79.0) |
2.94
(2.03–4.27) |
32.2
(23.0–42.4) |
79.3
(72.0–85.4) |
2.46
(1.83–3.33) |
| Poverty status¶¶ | ||||||||||||
| At or above poverty (Ref) | 25.3
(17.1–35.1) |
69.9
(63.1–76.1) |
2.76
(1.94–3.93) |
24.1
(17.2–32.1) |
70.1
(64.7–75.0) |
2.91
(2.14–3.95) |
20.7
(15.5–26.6) |
63.0
(57.2–68.5) |
3.05
(2.32–4.01) |
31.8
(24.6–39.7) |
75.6
(69.6–81.0) |
2.38
(1.87–3.02) |
| Below poverty | —†† | 50.6
(36.9–64.3) |
—†† | 24.5
(15.1–36.0) |
63.6
(51.7–74.3) |
2.60
(1.67–4.04) |
21.8
(11.7–35.1) |
59.7
(48.9–69.9) |
2.74
(1.61–4.66) |
25.3
(17.0–35.3) |
72.7
(62.1–81.8)** |
2.87
(1.98–4.15) |
| Area of residence*** | ||||||||||||
| Rural | —†† | 65.6
(51.9–77.6) |
—†† | —†† | 71.4
(58.9–81.9) |
—†† | —†† | 62.3
(50.1–73.5) |
—†† | 34.2
(24.1–45.5) |
80.2
(70.0–88.2) |
2.34
(1.70–3.23) |
| Non-rural (Ref) | 25.6
(17.4–35.3) |
65.3
(58.4–71.8) |
2.55
(1.80–3.63) |
24.7
(18.6–31.6) |
68.3
(63.0–73.3) |
2.77
(2.13–3.61) |
21.7
(16.5–27.7) |
61.7
(56.1–67.0) |
2.84
(2.18–3.70) |
28.4
(21.7–35.9) |
73.4
(67.5–78.8) |
2.59
(2.01–3.33) |
| Region††† | ||||||||||||
| Northeast (Ref) | —†† | 69.6
(54.9–81.9) |
—†† | —†† | 71.0
(59.7–80.7) |
—†† | 22.6
(10.5–39.2) |
64.3
(51.0–76.1) |
2.85
(1.53–5.33) |
27.1
(14.3–43.5) |
73.7
(60.7–84.3) |
2.72
(1.60–4.63) |
| Midwest | —†† | 76.5
(64.2–86.2) |
—†† | 26.3
(14.2–41.8) |
76.5
(66.7–84.6) |
2.91
(1.75–4.83) |
23.4
(14.0–35.3) |
60.2
(49.8–69.9)** |
2.57
(1.62–4.08) |
34.0
(22.6–47.0) |
77.7
(68.3–85.4) |
2.29
(1.59–3.28) |
| South | 26.8
(15.3–41.2) |
58.2
(48.0–67.9) |
2.17
(1.33–3.53) |
21.9
(14.3–31.1) |
60.7
(52.2–68.8) |
2.78
(1.88–4.10) |
19.7
(12.6–28.4) |
58.9
(50.9–66.6) |
3.00
(2.00–4.49) |
30.5
(22.7–39.1) |
73.7
(65.6–80.8)** |
2.42
(1.83–3.20) |
| West | —†† | 62.6
(47.8–75.9) |
—†† | —†† | 71.5
(60.9–80.6) |
—†† | 20.2
(10.9–32.6) |
65.9
(54.0–76.5) |
3.26
(1.92–5.55) |
—†† | 75.1
(60.2–86.6) |
—†† |
| Prenatal insurance coverage§§§ | ||||||||||||
| Private/military insurance only (Ref) | 26.8
(16.1–39.9) |
73.1
(65.0–80.2) |
2.73
(1.77–4.22) |
29.3
(20.1–39.9) |
73.4
(66.9–79.2) |
2.50
(1.79–3.50) |
17.9
(11.1–26.7) |
62.3
(55.2–69.2)** |
3.48
(2.27–5.33) |
29.6
(20.7–39.8) |
83.8
(77.8–88.8)** |
2.83
(2.06–3.89) |
| Any public insurance | 33.0
(21.1–46.8) |
55.2
(45.1–64.9) |
1.67
(1.11–2.52) |
22.4
(15.0–31.3) |
65.6
(57.7–72.9) |
2.93
(2.03–4.21) |
21.0
(14.9–28.2) |
60.8
(53.2–68.1) |
2.90
(2.09–4.02) |
29.7
(22.3–37.9) |
67.5
(59.5–74.9)** |
2.27
(1.72–3.00) |
| No insurance | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† |
| Provider vaccination recommendation/ offer | ||||||||||||
| Offered or referred (Ref) | 44.9
(33.1–57.3) |
77.0
(70.8–82.5) |
1.71
(1.31–2.25) |
43.8
(34.4–53.7) |
78.0
(73.0–82.3) |
1.78
(1.43–2.22) |
37.4
(29.5–45.8) |
74.4
(69.3–79.1) |
1.99
(1.60–2.48) |
46.1
(38.3–54.1) |
81.2
(76.7–85.2) |
1.76
(1.48–2.10) |
| Recommended, no offer or referral | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† |
| No recommendation | —†† | —†† | —†† | 0.0
(0.0–3.5) |
—†† | —†† | —†† | —†† | —†† | —†† | —†† | —†† |
Abbreviations: CI: Confidence Interval.
* Respondents who delivered a live birth since August 1st of the year prior to their interview (April 2020, March-April 2021, March-April 2022, or March-April 2023) and had known Tdap vaccination status were included in the analyses to assess Tdap vaccination coverage during the 2019–20, 2020–21, 2021–22, and 2022–23 influenza seasons. Women who reported receiving a Tdap vaccination during their pregnancy were considered vaccinated.
† Respondents were asked the following question, “Overall, how hesitant are you about Tdap vaccination during your pregnancy?” [1. Not at all hesitant, 2. Not that hesitant, 3. Somewhat hesitant, 4. Very hesitant]. “Very hesitant” and “Somewhat hesitant” were considered “Hesitant” and “Not that hesitant” and “Not at all hesitant” were considered “Not hesitant.”
§ The total unweighted number of respondents in the sample.
¶ Korn-Graubard 95% confidence interval.
** Estimate is statistically different from 2019–20.
†† Estimate does not meet the NCHS standards of reliability. https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf
§ Race and ethnicity was self-reported. Respondents identified as Hispanic might be of any race. The “Other” race category included Asians, American Indians/Alaska Natives, Native Hawaiians or other Pacific Islanders, and women who selected “other” or multiple races; the “other” response option was removed from the survey in 2023.
¶¶ Poverty status was defined based on the reported number of persons living in the household and annual household income, according to U.S. Census poverty thresholds. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html
*** Rurality was defined using ZIP codes where >50% of the population resides in a nonmetropolitan county, a rural U.S. Census tract, or both, according to the Health Resources and Services Administration’s definition of rural population. https://www.hrsa.gov/rural-health/about-us/definition/index.html
††† Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin. South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
§§ Respondents who had delivered by their survey date were asked what medical insurance or medical care coverage they had during their most recent pregnancy. Women considered to have public insurance selected at least one of the following: Medicaid, Medicare, state-sponsored medical plan, or other government plan. §§§ Respondents considered to have private/military insurance selected private medical insurance and/or military medical care and did not select any type of public insurance.
- For influenza and Tdap, vaccination coverage decreases as the degree of reported hesitancy increases (Table 3).
Table 3. Influenza and tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccination coverage among pregnant women, by hesitancy* – Internet panel survey, United States, 2019–20 through 2022–23 influenza seasons
| 2019–20 Weighted % Vaccinated (95% CI)† |
2020–21 Weighted % Vaccinated (95% CI)† |
2021–22 Weighted % Vaccinated (95% CI)† |
2022–23 Weighted % Vaccinated (95% CI)† |
|
| Influenza | N=1,839 | N=1,793 | N=2,015 | N=1,812 |
| Not at all hesitant | 82.3 (77.0–86.8) | 84.2 (76.6–90.1) | 81.1 (75.1–86.2) | 77.8 (70.0–84.5) |
| Not that hesitant | 69.1 (63.2–74.6) | 70.5 (62.3–77.8) | 59.4 (53.6–65.0)§, ¶ | 64.3 (58.4–69.9) |
| Somewhat hesitant | 46.0 (40.7–51.3) | 39.1 (33.4–45.0) | 39.5 (34.5–44.6) | 41.5 (36.3–46.9) |
| Very hesitant | 22.0 (17.5–27.0) | 19.7 (15.2–24.8) | 21.6 (15.8–28.2) | 18.7 (14.5–23.4) |
| Tdap | N=463 | N=728 | N=838 | N=776 |
| Not at all hesitant | 78.7 (71.5–84.9) | 78.0 (71.9–83.3) | 72.2 (65.2–78.5) | 82.0 (75.8–87.1)§ |
| Not that hesitant | 49.1 (39.8–58.5) | 56.3 (48.7–63.8) | 51.5 (44.3–58.7) | 67.1 (59.0–74.6)§,¶ |
| Somewhat hesitant | 38.6 (28.3–49.9) | 37.0 (28.6–46.2) | 25.8 (20.0–32.3)§,¶ | 39.9 (32.1–48.1) § |
| Very hesitant | —** | —** | —** | 13.2 (7.6–20.8) |
Abbreviations: CI: Confidence Interval.
* Respondents were asked the following questions, “Overall, how hesitant are you about flu vaccination during your pregnancy?” and “Overall, how hesitant are you about Tdap vaccination during your pregnancy?” [1. Not at all hesitant, 2. Not that hesitant, 3. Somewhat hesitant, 4. Very hesitant].
† Korn-Graubard 95% confidence interval.
§ Estimate is statistically different from the prior year.
¶ Estimate is statistically different from 2019–20.
** Estimate does not meet the NCHS standards of reliability. https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf
- The percent of women who reported receiving a provider offer or referral for Tdap vaccination increased from 2019–20 to 2022–23 among women ‘not at all hesitant’ and ‘not that hesitant’ (Figure 2). No significant changes were observed in provider offer or referral for influenza vaccination.
- For influenza vaccine and Tdap, the likelihood of reporting receipt of a provider offer or referral for vaccination decreases as the degree of hesitancy increases.
Figure 2. Receipt of a provider offer or referral for influenza* and tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap)† vaccination by hesitancy§ status – Internet panel survey, United States, 2019–20 through 2022–23 influenza seasons
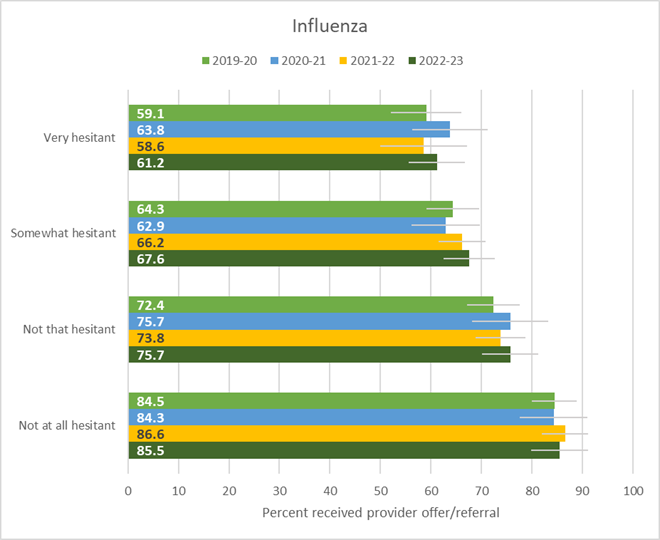
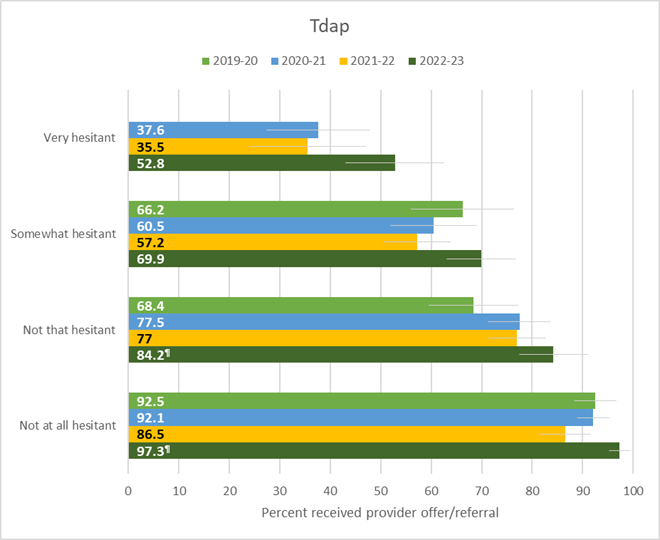
*Respondents pregnant anytime during October–January during the influenza season at the time of interview, with known influenza vaccination status and at least one provider visit since July 1st of the year prior to their interview, were included in the analysis for influenza (N=1,811 in 2019–20, N=1,784 in 2020–21, N=1,999 in 2021–22, and N=1,786 in 2022–23).
†Respondents pregnant since August 1st of the year prior to their interview, had recently delivered a live birth, and had known Tdap vaccination status were included in the analysis for Tdap (N=463 in 2019–20, N=728 in 2020–21, N=838 in 2021–22, and N=776 in 2022–23). For 2019–20, the estimate among the ‘Very hesitant’ is suppressed because it does not meet the NCHS standards of reliability (https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf).
§Respondents were asked the following questions, “Overall, how hesitant are you about flu vaccination during your pregnancy?” and “Overall, how hesitant are you about Tdap vaccination during your pregnancy?” [1. Not at all hesitant, 2. Not that hesitant, 3. Somewhat hesitant, 4. Very hesitant].
¶ Estimate is statistically different from 2019–20.
Vaccine hesitancy is associated with lower vaccination coverage among pregnant women for both influenza and Tdap vaccines. Increases in hesitancy about both vaccines have been observed since the start of the COVID-19 pandemic, particularly after the 2020–21 influenza season when a vaccine for COVID-19 became available [5]. Continued increases in vaccine hesitancy threaten to further adversely impact maternal vaccination coverage, which has historically been low [6]. A decrease in influenza vaccination among both hesitant and non-hesitant pregnant women was observed from 2019–20 through 2022–23, suggesting factors in addition to vaccine hesitancy contributed to this decline. While the increase in Tdap hesitancy did not correspond with an overall decline in Tdap vaccination coverage, this increase in hesitancy was likely offset by an increase in vaccination coverage among non-hesitant women.
A provider offer or referral for vaccination has previously been shown to be associated with increased uptake of maternal influenza and Tdap vaccination [4,7]. The increase in reported receipt of a provider offer or referral for Tdap vaccination since 2019–20 among women “not that hesitant” about vaccination may have contributed to the increase in Tdap coverage observed among these women. Even among hesitant women, a substantial percentage were vaccinated for influenza and Tdap in 2022–23 if they reported receiving an offer or referral for vaccination from their provider. Moreover, while hesitancy was associated with non-vaccination, this association was weaker among women who received a provider offer or referral for vaccination. These findings reinforce that a provider offer or referral for vaccination is an important tool to help overcome vaccine hesitancy. In 2022–23, approximately 40% of those very hesitant and >30% of those somewhat hesitant did not report receiving an offer or referral for influenza vaccination, and approximately half of those very hesitant and 30% of those somewhat hesitant did not receive an offer or referral for Tdap vaccination. Reducing missed opportunities for provider engagement could increase maternal vaccination coverage. Providers treating pregnant patients are encouraged to follow the Standards for Adult Immunization Practice by assessing vaccination status at every clinical encounter, strongly recommending vaccines that their patients need, administering needed vaccines or referring patients to a vaccination provider, and documenting vaccines administered in their jurisdiction’s immunization information system [8]. Because many pregnant women have multiple healthcare visits during pregnancy, including during the third trimester when Tdap vaccination is specifically recommended, prenatal care providers can consider repeatedly offering influenza and Tdap vaccination or referrals to patients who remain unvaccinated. Research on COVID-19 vaccination in non-pregnant people demonstrated that repeatedly offering vaccination to persons who had initially declined it resulted in higher vaccination uptake overall [9].
Findings in this report are subject to at least six limitations of the survey. First, this was a nonprobability sample, and results might not be generalizable to all pregnant women in the United States. Second, vaccination status was self-reported and may be subject to recall or social desirability bias. Third, due to small sample size, vaccination coverage could not be assessed separately among some groups. Fourth, Tdap coverage estimates might be subject to uncertainty given the small sample size and exclusion of 12.2%–14.9% of women with unknown Tdap vaccination status. Fifth, causality or direction of the association between provider offer or referral and lower hesitancy cannot be assessed with these cross-sectional data. Finally, statistical tests based on the assumption of probability were used to determine differences between groups in this non-probability sample, and results should be interpreted with caution. Despite these limitations, Internet panel surveys are a useful assessment tool for timely evaluation of influenza and Tdap vaccination coverage and attitudes towards vaccination among pregnant women.
Authors
Kayla Calhoun, MS1; Katherine E. Kahn, MPH1,2; Hilda Razzaghi, PhD1; Emma Garacci, MS1,3; Megan Lindley, MPH1; Carla L. Black, PhD1
1Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC; 2Leidos, Atlanta, Georgia; 3Cherokee Nation Operational Solutions, Tulsa, Oklahoma
- Razzaghi, H, Kahn, KE, et al. Influenza, Tdap, and COVID-19 Vaccination Coverage and Hesitancy Among Pregnant Women — United States, April 2023. MMWR. 2023; 72(39);1065–1071.
- Santibanez TA, Nguyen KH, Greby SM, Fisher A, Scanlon P, Bhatt A, Srivastav A, Singleton JA. Parental Vaccine Hesitancy and Childhood Influenza Vaccination. Pediatrics. 2020 Dec;146(6):e2020007609. PMID: 33168671.
- Srivastav A, Lu PJ, Amaya A, Dever JA, Stanley M, Franks JL, Scanlon PJ, Fisher AM, Greby SM, Nguyen KH, Black CL. Prevalence of influenza-specific vaccination hesitancy among adults in the United States, 2018. Vaccine. 2023 Apr 6;41(15):2572-2581. PMID: 36907734.
- Kahn, K.E., et al.. Flu, Tdap, and COVID-19 Vaccination Coverage Among Pregnant Women – United States, April 2022. 2022; Available from: https://www.cdc.gov/flu/fluvaxview/pregnant-women-apr2022.htm.
- Fortner A, Schumacher D. First COVID-19 Vaccines Receiving the US FDA and EMA Emergency Use Authorization. Discoveries (Craiova). 2021 Mar 5;9(1):e122. PMID: 33969180.
- CDC. FluVaxView Interactive. Vaccination Coverage among Pregnant Women. 2023; Available from: https://www.cdc.gov/flu/fluvaxview/interactive-pregnant-women.htm.
- Razzaghi H, Kahn KE, Black CL, et al. Influenza and Tdap Vaccination Coverage Among Pregnant Women — United States, April 2020. MMWR Morb Mortal Wkly Rep 2020;69:1391–1397. PMID: 33001873.
- Orenstein, W.A., et al., Recommendations from the National Vaccine Advisory committee: standards for adult immunization practice. Public Health Rep, 2014. 129(2): p. 115-23. PMID: 24587544.
- Gregory B, Franks A, Morales L, et al. System Interventions to Reduce Disparities in Covid-19 Vaccine Offer Rates. NEJM Catal Innov Care Deliv 2022;3(7).