Global Health Security Investments Prepare Guinea and Uganda for COVID-19
December 8, 2020
Uganda FETP residents review records after testing truck drivers during the COVID-19 pandemic in Kampala, Uganda. Photo: Edger Ampaire, AFENET
CDC’s technical and financial investments to build global health security capacity through the Global Health Security Agenda (GHSA), National Public Health Institutes (NPHI), and other programs have prepared countries such as Guinea and Uganda to quickly respond to public health threats. In recent years, the world has seen the social and economic effects of highly infectious diseases, such as the Ebola epidemics in Africa and now COVID-19. As public health threats increase globally, every country needs core public health capacities to prevent, detect, and respond effectively to disease threats.
Ebola Helped Guinea Move Toward Public Health Preparedness

During the 2014-2015 Ebola outbreak, Guinea needed help to manage the outbreak and established Ebola Treatment Centers to care for patients. Photo: Idrissa Balde, TEPHINET
When the Ebola outbreak was declared in West Africa in 2014, Guinea’s public health system was inadequately prepared to respond to the threat. Guinea had no formal emergency management system before 2015, and no skilled disease detective workforce to manage the outbreak. Ebola eventually spread across borders into Sierra Leone and Liberia, and then spread into Guinea’s capital city of Conakry.
Since the Ebola outbreak, CDC has worked with the Guinea Ministry of Health (MOH) and other partners to use GHSA investments in four critical areas of public health—surveillance, workforce development, laboratories, and emergency management and response—to build capacity and improve outbreak response. For example, CDC and its partners developed a nationally coordinated network of emergency operations centers (EOCs) including one national and 38 district-level EOCs. Members of Guinea’s MOH received CDC emergency management training and with CDC assistance were able to train network staff.
In July 2016, Guinea’s NPHI, called the National Agency for Health Security (ANSS), was created to oversee critical public health functions, working in coordination with the EOC. The ANSS has provided strong leadership and management skills to the COVID-19 response.
Another GHSA investment, Guinea’s Field Epidemiology Training Program (FETP), established in 2017, trains “disease detectives” who serve as boots on the ground during outbreaks. For the COVID-19 pandemic, they quickly responded and used their expertise in outbreak management and response to play leading roles, including surveillance and contact tracing. GHSA funding also helped improve Guinea’s national and regional laboratory capacity, making it possible for Guinea to test in-country for COVID-19. Through GHSA resources, CDC supported the rollout of District Health Information Software 2 (DHIS2) as the key surveillance data platform. These improvements positioned Guinea to better manage the pandemic throughout the country.
GHSA Investments in Uganda Improve the COVID-19 Response
Uganda, a “hot zone” for infectious diseases, is no stranger to public health outbreaks. In 2013, the Ugandan MOH began to discuss creating what is now the Uganda NPHI. CDC provided technical assistance to help develop the NPHI and assisted Uganda in organizing its response activities.
Through GHSA funding, CDC has provided over $40 million since 2016 to help Uganda respond to Ebola and other infectious disease outbreaks. This funding, coupled with other financial support from CDC, has helped Uganda improve its health systems.
With CDC’s assistance, Uganda’s EOC activated its national task force to prepare for the COVID-19 pandemic and established an incident management structure before any cases were detected in the country. On March 21, 2020, the country’s preparedness was put to the test when the first COVID-19 case was confirmed. Uganda’s EOC, which was already responding to Ebola as well as five other outbreaks, quickly confronted the new threat.
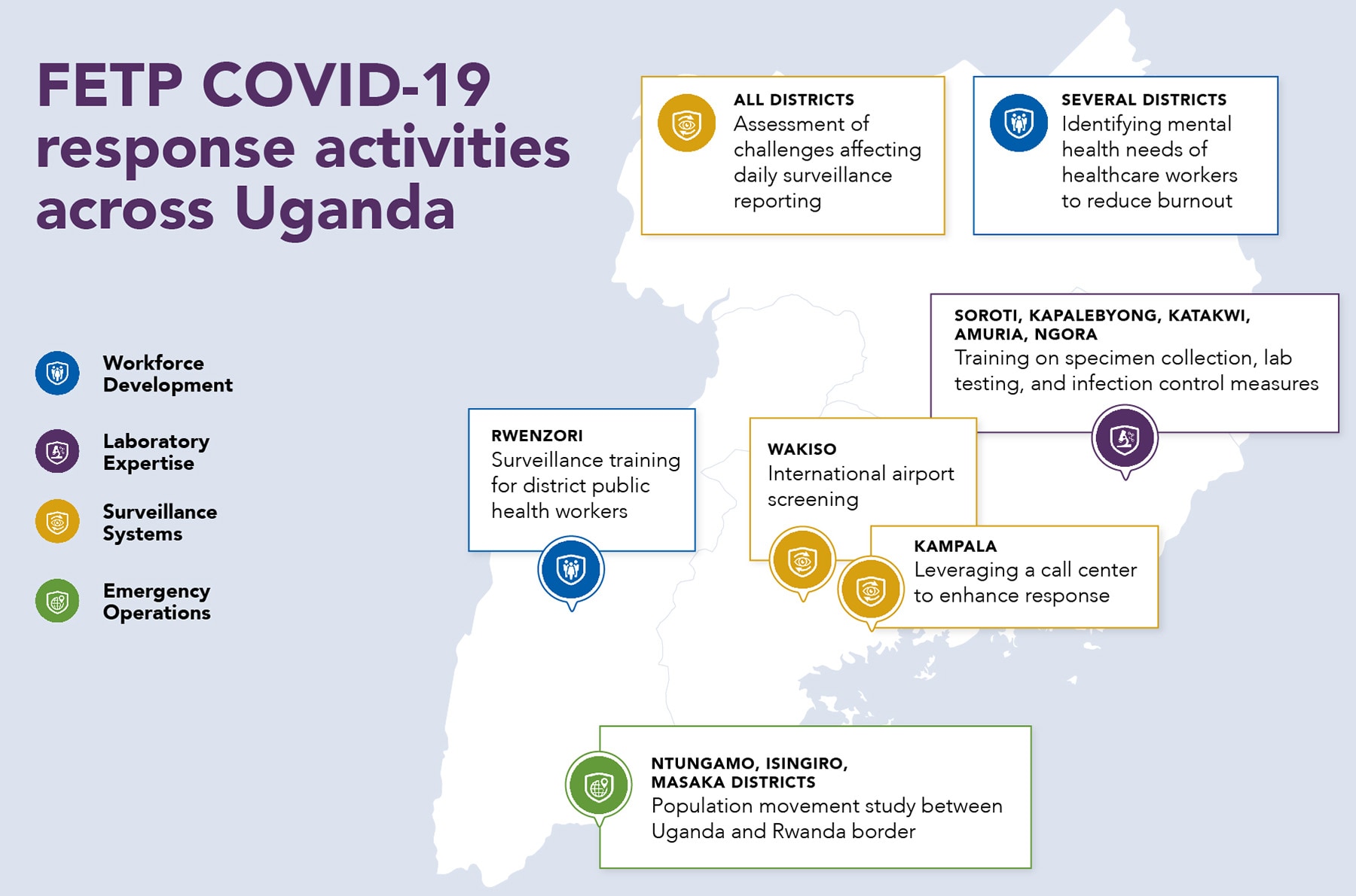
Like Guinea, Ugandan FETP disease detectives leapt into action and harnessed their outbreak response expertise at the start of the COVID-19 pandemic. They led key response activities across the country, including managing data collection and laboratory processes, setting up and carrying out 24/7 airport screening, and coordinating COVID-19 trainings in the districts.
GHSA investments also improved Ugandan laboratory capacity and helped Uganda set up two mobile testing laboratories along with a new team to support increased COVID-19 testing. Through December 1, 2020, Uganda has processed 625,752 COVID-19 samples using CDC-supported in-country labs. Countrywide testing for COVID-19 was made possible by the CDC-established sample-and-result-return network that allows sample movement from collection facilities to testing labs and return of results through the electronic results download system.
Additionally, CDC supported the reconfiguration of Uganda’s electronic Integrated Disease Surveillance and Response (IDSR) system, previously used for tracking and reporting other outbreaks, for the COVID-19 pandemic. IDSR handled case reporting in high-traffic points of entry such as airports and border crossings.
These GHSA-supported advancements helped curb the spread of COVID-19 for months after other countries felt its impact. The Lancetexternal icon Journal rated Uganda in the top ten for countries suppressing COVID-19 within their borders in August.
“Uganda’s continued commitment to data and science-backed decision-making is really key. CDC’s position as a trusted partner — a position built through years of technical and financial support — is the most important thing for us.”
– Dr. Amy Boore, Division of Global Health Protection Uganda Program Director
The Future of GHSA
Previous GHSA and NPHI investments helped countries be better prepared to respond to COVID-19. But even with these investments, the COVID-19 pandemic has shown there is much more work to be done. Today, more than two-thirds of the world remains underprepared to prevent, detect, and respond to a public health emergency. CDC investments in global health security strengthen the health systems that keep us all safe. To ensure that countries are better prepared to effectively manage current and future disease outbreaks before they become pandemics, investments in global health security must continue.