HIV Services Branch
CDC has supported the HIV Care and Treatment program in Zimbabwe since its inception in 2004, and currently implements these activities across 20 districts in the provinces of Mashonaland West, Mashonaland Central, Mashonaland East, Matabeleland North, and Harare. With President’s Emergency Plan for AIDS Relief (PEPFAR) support, ART coverage has been increasing within CDC districts and nationally. By the end of 2019, ART coverage among all HIV positive adults was 82% for adult men and 88% for adult women. Coverage for children was slightly lower at 78%.
The Zimbabwe HIV Care and Treatment program continues to provide comprehensive HIV testing and treatment services for People Living with HIV/AIDS (PLHIV) through two clinical implementing partners who work across 442 sites.
- HIV Testing and Linkage to Care
- Success Story: Site Improvement with Zimbabwe Intensive Monitoring and Support
- Cervical Cancer Screening and Treatment
- Prep Success Story in Mazowe
- Success Story- Improving Access and Optimizing Client-Centered and Friendly Services for Key Populations in Harare District
- Reaching for Epidemic Control with Zach’s Community Peer Mentors
HIV Testing and Linkage to Care
During 2019, the MoHCC has specifically highlighted human resource challenges in meeting the needs of a maturing HIV program throughout the HIV clinical cascade, a trend which continues through doctors and nurses strikes. As Zimbabwe has adopted the ambitious Joint United Nations Programme on HIV and AIDS (UNAIDS) Fast Track strategy for ending the AIDS epidemic by 2030, differentiated service delivery models have become increasingly necessary to increase convenience and access for patients, reduce out-of-pocket expenditure, and decongest clinical facilities. The integrated HIV Testing Services (iHTS) strategy was developed in response to changing needs for differentiated testing models.
The iHTS strategy was fully implemented in 2019, which included scale up of index testing for newly diagnosed PLHIV and roll out of HIV self-testing. Districts were classified into high, medium and low gap based on the Spectrum generated number of PLHIV needing treatment. Throughout FY19, the proportion of new positives identified through index testing increased over time and a higher proportion of new positives came from index testing in low gap districts compared to high and medium gap districts. Targeted testing strategies will remain important towards finding the remaining undiagnosed PLHIV to achieve 95-95-95 targets (95% of people living with HIV knowing their status; 95% of people who know their status on treatment; and 95% of people on treatment with suppressed viral load).
Figure 1: Review of the iHTS Strategy
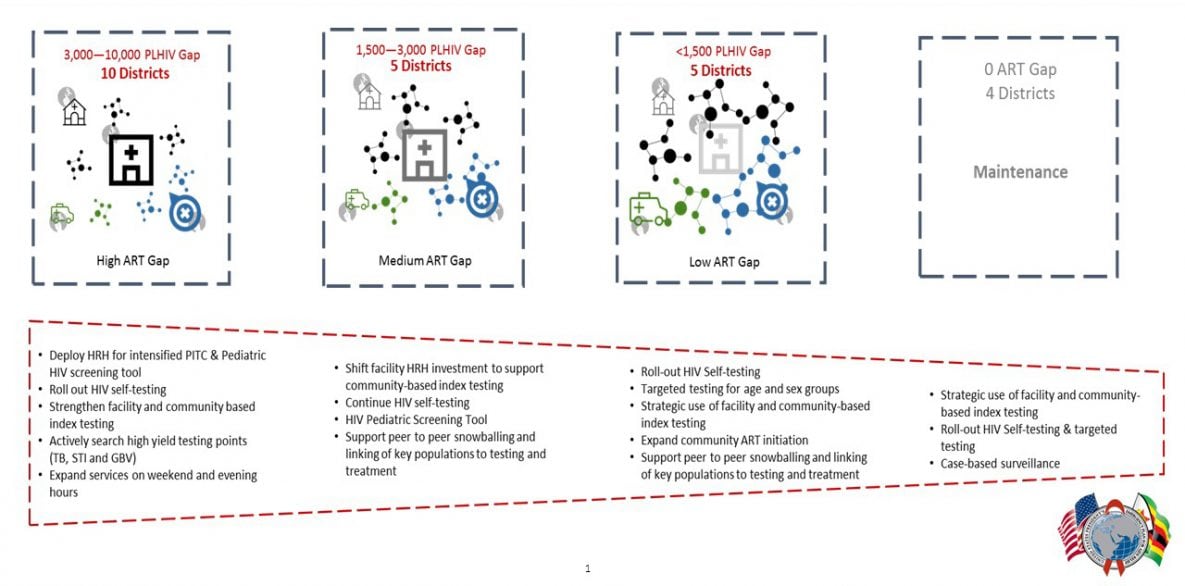
The iHTS strategy was fully implemented in 2019, which included scale up of index testing for newly diagnosed PLHIV and roll out of HIV self-testing. Districts were classified into high, medium and low gap based on the Spectrum generated number of PLHIV needing treatment. Throughout FY19, the proportion of new positives identified through index testing increased over time and a higher proportion of new positives came from index testing in low gap districts compared to high and medium gap districts. Targeted testing strategies will remain important towards finding the remaining undiagnosed PLHIV to achieve 95-95-95 targets (95% of people living with HIV knowing their status; 95% of people who know their status on treatment; and 95% of people on treatment with suppressed viral load).
Figure 2: Distribution of HTS_TST_POS by Testing Modality, FY19 Q1 – Q4
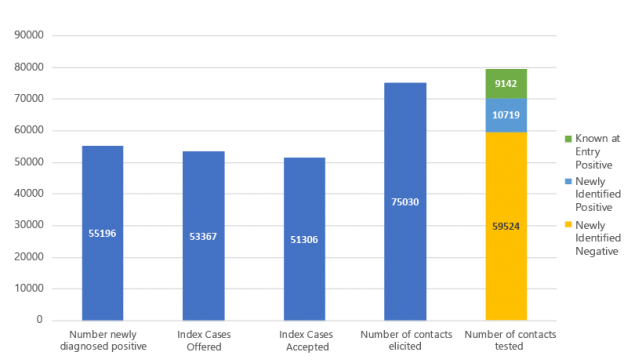
CDC supported HIV programs offered index testing to 53,367 PLHIV during FY19. Of those, 51,306 (96%) accepted index testing and 75,030 contacts were elicited. Through index testing efforts, 10,719 new positives were identified.
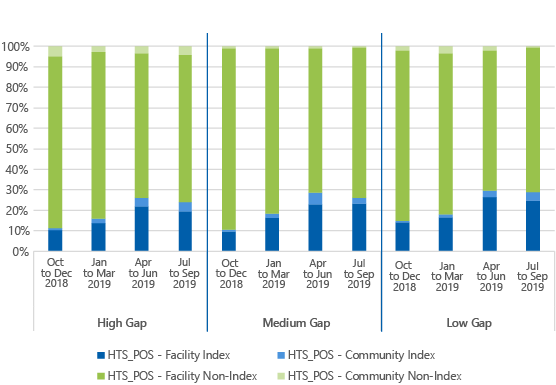
Figure 3: COP18 Index Case Testing Cascade
In addition, linkage to HIV care and treatment for clients at CDC-supported sites has increased over time to over 90%. This reflects PEPFAR support for training as well as additional staff supporting testing and linkage activities in Zimbabwe.
Figure 4: Linkage Trends
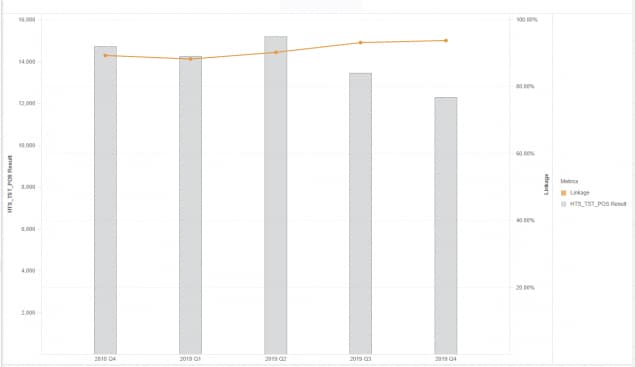
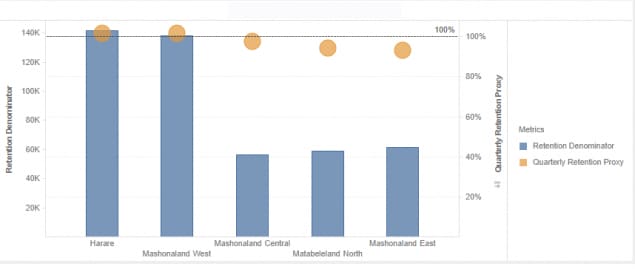
Figure 5: Retention Proxy and TX_CURR
Figure 5 shows the proxy retention estimates from Quarter 3 to Quarter 4 at CDC supported sites in five provinces. This retention measure exceeds 90% in all five provinces and exceeds 95% in Harare, Mashonaland West, and Mashonaland Central.

CDC, MoHCC health facility, district, provincial and implementing partner staff conduct a ZIMS visit.

CDC, MoHCC health facility, district, provincial and implementing partner staff after a ZIMS visit
In the past year, CDC developed a novel strategy for site improvement. Built upon Site Improvement Through Monitoring System (SIMS), we began implementing Zimbabwe Intensive Monitoring Support (ZIMS). This site monitoring model involves half day site visits to health facilities by CDC staff to work with teams including facility, district, provincial and implementing partner staff. During this visit, 11 technical areas are assessed including those assessed through SIMS with deeper dives into the index testing cascade, Tuberculosis (TB) preventive therapy (TPT) cascade, and additional modules related to case-based surveillance and receny testing. ZIMS focuses on monitoring, supportive supervision, and capacity building exercises using medical registers and records routinely collected at HIV service delivery facilities to both assess the program and provide capacity building during the visit. The exercises allow the entire team to look at the quality of care in a group setting and facilitate on-the-spot mentorship to make corrections and address challenges in HIV case-finding and patient care. So far, ZIMS visits have been conducted in Matabeleland North, Mashonaland West, and Harare.
When a health facility is found to need improvement across multiple program areas, the site is revisited after about two months. Two facilities in need of improvement were identified in the first round of ZIMS. The revisits showed marked improvement including a focus on improved and optimized staffing and improved performance across HIV program areas. At one site, the facility staff had been unable to locate the patient files requested. As part of the remediation process, the site involved the full staff (including drivers) to redo their patient filing system. During the revisit, all files requested were located as a result of this effort. These sites also saw dramatic improvement in TPT coverage, VL coverage, HIV index testing for patients not virally suppressed (and more likely to transmit HIV), elicitation of sexual contacts so they could be followed up with HIV testing services, and documentation. Most importantly, staff at these facilities were proud of their work and accomplishments and were further motivated to offer improved patient care that will save lives.
Cervical Cancer Screening and Treatment
HIV remains an important risk factor for cervical cancer, with HIV-positive women 4-5 times more likely to develop cervical cancer compared to HIV-negative women. The Zimbabwe Demographic and Health Survey (ZDHS) 2015 reported 79% of women had heard of cervical cancer but only 13% ever had a cervical examination. Many women were therefore surviving HIV but dying from cervical cancer, a condition that is both preventable and curable. In order to address this critical need and associated gaps, CDC Zimbabwe introduced cervical screening using visual inspection with acetic acid and cervicography (VIAC) and treatment with cryotherapy, thermal coagulation or Loop Electrosurgical Excision Procedure (LEEP) in a see and treat approach in FY19.
CDC Zimbabwe and its clinical implementing partners introduced and scaled up cervical screening across all CDC supported districts thereby preventing women from developing cervical cancer. This was done through the integration of cervical cancer screening into existing HIV services, extensive technical support and revitalization of existing VIAC sites, recruitment and training of nurses and doctors who conduct cervical cancer screening and treatment, setting up of new VIAC sites to increase coverage and access, and demand creation among HIV positive women.
During FY19, CDC supported the revitalization of 39 VIAC sites and set up 12 new VIAC sites. To build human resource capacity, 72 nurses, 5 doctors, 3 clinical officers and 13 mentors/coordinators were trained quality quality cervical screening and treatment in CDC supported districts and facilities.
CDC and its clinical implementing partners International Training & Education Center for Health (ITECH) and Zimbabwe Association of Church-related Hospitals (ZACH) rapidly scaled up VIAC over FY19, achieving a remarkable 75% of the annual target as illustrated in Figure 6 below.
Figure 6: Number of Clients Screened for Cervical Cancer Using VIAC by Month Showing an Upward Trend
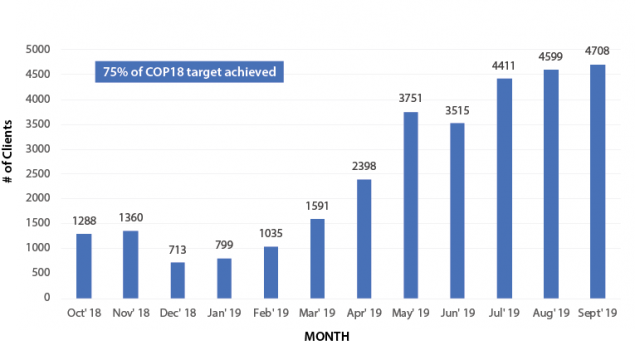
A total of 36,127 HIV positive women aged 25-49 years were screened. Service provision started at only 33 high volume sites in early Country Operation Plan (COP) 18. At the end of COP18, 48 facilities were providing VIAC, supported by direct service delivery (DSD) health care workers recruited and/or trained and deployed by CDC partners. The successful introduction and implementation of the program was a result of close collaboration between CDC and its Implementing Partners (IPs) and the MoHCC, recruitment and training of additional health care workers (HCWs) with a focus on VIAC, setting up VIAC sites within Opportunistic Infections (OI)/ART clinics, demand creation through integrated treatment literacy health education talks, and intensive site support and supervision to monitor implementation fidelity and provide on-site mentorship.
However, while encouraging screening numbers were achieved, treatments rates for eligible women were lower than expected as illustrated in Figure 7 below.
Figure 7: CDC FY18 Cervical Cancer Cascade: Overall
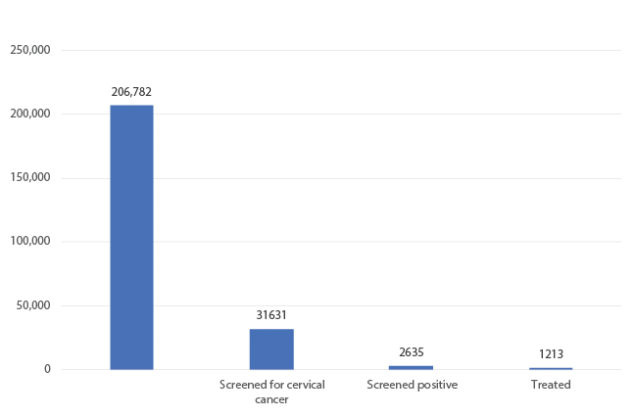
Although the positivity rate of 8% is within the expected range, the treatment rate falls short of the expected minimum of 70%. In the coming year, CDC will prioritize efforts to increase coverage of access to treatment services for all eligible women while strengthening the referral system for those women requiring advanced treatment procedures that may not be available locally.

CDC, ZimTTECH and MOHCC cadres review HIV program registers at Mdutshane Clinic in Bubi District.

ZIMS assessment at Siganda Clinic in Bubi District of Matabeleland North Province.

CDC, district, provincial and partner teams meet with Nkayi leadership during a ZIMS visit.
Mazowe district is using the Peer-to-Peer model to raise oral Pre-Exposure Prophylaxis (PrEP) awareness and create demand for service uptake amongst adolescent girls and young women (AGYW) at risk of contracting HIV. Through the model, a total of 523 AGYW were reached with PrEP messages between January and December 2019. Amongst the AGYW reached is a 21 year old sex worker who was introduced to sex work at 19 by her two sisters in the same profession. She has had sex with men from all walks of life. We will call her Hope in this story.

Most of the time, Hope uses protection during sex but occasionally, some partners pressure her into having unprotected sex with them by offering large sums of cash. All her sexual partners were of unknown HIV status. Hope has been physically and sexually abused more than twice by some of her clients. Hope has contracted and has been treated for Sexually Transmitted Infections (STIs) several times but does not have HIV.
After hearing about PrEP through a PrEP Champion at Bare Clinic in February 2019, Hope decided to be initiated that month as she considered herself to be at significant risk of contracting HIV. During initiation, she consented to follow-ups through phone calls and physical visits to her place of residence by community health workers.
Two weeks after starting PrEP, Hope failed to turn up for her month one visit. In person follow-ups to her place of residence were made by PrEP Champions and Hope had this to say:
“Taking pills daily is proving to be more work than I anticipated. Yes, I am at risk, yes, I want to remain HIV negative for the rest of my life, but the pill burden is way too much for me. What should I do?”
After noting her concerns, Hope was referred to her local clinic for further counselling. She was re-sensitised on the benefits of combination HIV prevention and was given adherence counselling. Hope decided to be re-initiated on PrEP in April 2019 and since then, she has been consistently taking her drugs. She continues getting adherence support from PrEP Champions. To date, Hope remains HIV negative. She last tested for HIV in September 2019 and her results came out negative. Through using oral PrEP, Hope remains a role model sex worker who refuses to let her lifestyle determine her HIV status.
During our last recent encounter with her, she had this to say:
“I am proud to be on PrEP. Though I still have unprotected sex once in a while, I feel safe because I know I have some level of protection. PrEP has given me control over my health. I am prepared”
The target population for the Key Populations (KP) program in Harare District is men who have sex with men (MSM) while other subpopulation groups within the KP category such as sex workers (SW), transgender persons and people who inject drugs (PWID) are also considered. The comprehensive and friendly Sexual and Reproductive Health (SRH) and HIV services for KPs are offered through 13 CDC-supported facilities. In FY19, COP18 was the increase in the number of KPs who accessed services, in particular, linkage to PrEP as a prevention method. Other services also saw an increase in uptake despite the challenges with Monitoring and Evaluation (M&E) tools in capturing the client data.
Figure 9: KPs accessing a Wide Range of Services in Public Sector Facilities in Harare, COP18
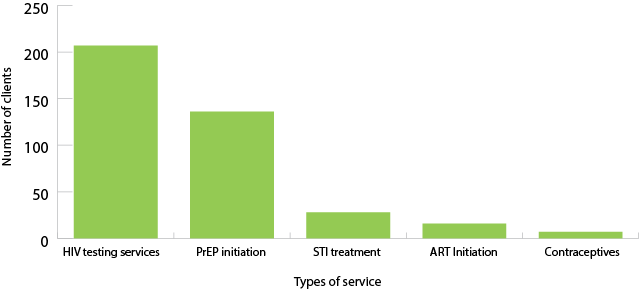
The most common service accessed in the 13 supported public sector facilities in Harare was HIV testing services (HTS) followed by PrEP initiation.
The following strategies were employed in order to achieve the project objectives as far as building capacity for public health facilities to offer KP friendly services, raising awareness among KP’s on comprehensive combination HIV prevention and treatment as well as improving access to client centred HIV services such as prevention and treatment literacy sessions and targeted KP moonlight outreach.
Stories of Change from two supported facilities
After attending the literacy session, I wanted to take up PrEP but I was afraid to get it from a public clinic. I was afraid of being stigmatized by the nurses and lack of privacy. Through the help of a community facilitator (CF) who escorted me through the process, I felt more comfortable and realized that the nurses were actually friendly. I have been on PrEP for over a month now and I am confident in sharing with my other colleagues who are afraid of visiting the public clinics”.
– Tambirai (MSM)
I was doing my routine facility visit walking through the hallway, some people sitting waiting for services started to look at me differently and making gestures because of my posture. I engaged the primary counsellor (PC) and took the opportunity to sensitize the people who were waiting for services about KPs and my role at the clinic and I told them I am representing many (KP community). The Nurse In Charge and PC weighed in on my role at the facility’’
– Mai Precious, Community Facilitator, Tariro Clinic.
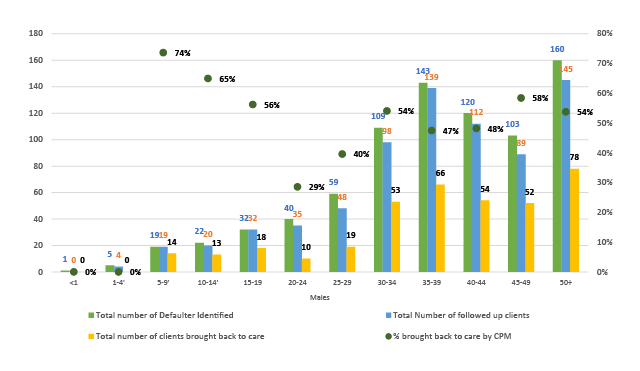
Reaching for Epidemic Control with ZACH’s Community Peer Mentors
Throughout FY19, a total of 239 Community Peer Mentors (CPMs) from 16 high volume sites have been active in offering psychosocial counselling, adherence counselling, defaulter tracking, demand creation for viral load collection to their peers. The CPMs have been instrumental in bringing defaulters back to care (Figure 10). A list of defaulters generated by the facilities are given to the CPMs monthly to conduct follow-up of all clients who have been considered to be defaulters. In addition to following up of defaulters, CPMs ensure that all followed up clients are given health education and counseling on the importance of adherence to treatment. During the period under review, tracking of defaulters continued for more than 90 days before being declared lost to follow up (LTFU).
Figure 10a: CPMs in Defaulter Tracking Among Females
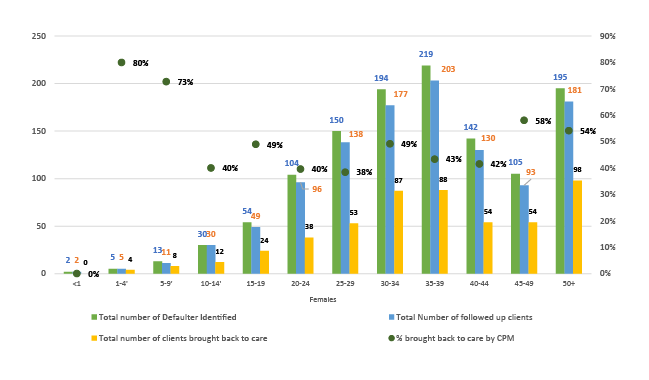
Figure 10b: CPMs in Defaulter Tracking Among Males