Malaria Diagnosis (United States)
Malaria must be recognized promptly in order to treat the patient in time and to prevent further spread of infection in the community via local mosquitoes.
Malaria should be considered a potential medical emergency and should be treated accordingly. Delay in diagnosis and treatment is a leading cause of death in malaria patients in the United States.
Malaria can be suspected based on the patient’s travel history, symptoms, and the physical findings at examination. However, for a definitive diagnosis to be made, laboratory tests must demonstrate the malaria parasites or their components.

A patient with fever who had recently traveled to a malaria-endemic country is being evaluated in the emergency room.
Diagnosis of malaria can be difficult:
- Where malaria is not endemic any more (such as in the United States), health-care providers may not be familiar with the disease. Clinicians seeing a malaria patient may forget to consider malaria among the potential diagnoses and not order the needed diagnostic tests. Laboratorians may lack experience with malaria and fail to detect parasites when examining blood smears under the microscope.
- In some malaria-endemic areas, malaria transmission is so intense that a large proportion of the population is infected but not made ill by the parasites. Such carriers have developed just enough immunity to protect them from malarial illness but not from malarial infection. In that situation, finding malaria parasites in an ill person does not necessarily mean that the illness is caused by the parasites.
Clinical diagnosis is based on the patient’s symptoms and on physical findings at examination.
The first symptoms of malaria (most often fever, chills, sweats, headaches, muscle pains, nausea and vomiting) are often not specific and are also found in other diseases (such as the “flu” and common viral infections). Likewise, the physical findings are often not specific (elevated temperature, perspiration, tiredness).
In severe malaria (primarily caused by Plasmodium falciparum), clinical findings (confusion, coma, neurologic focal signs, severe anemia, respiratory difficulties) are more striking and may increase the index of suspicion for malaria.
Clinical findings should always be confirmed by a laboratory test for malaria.
In addition to ordering the malaria specific diagnostic tests described below, the health-care provider should conduct an initial workup and request a complete blood count and a routine chemistry panel. In the event that the person does have a positive malaria test, these additional tests will be useful in determining whether the patient has uncomplicated or severe manifestations of the malaria infection. Specifically, these tests can detect severe anemia, hypoglycemia, renal failure, hyperbilirubinemia, and acid-base disturbances.
Malaria parasites can be identified by examining under the microscope a drop of the patient’s blood, spread out as a “blood smear” on a microscope slide. Prior to examination, the specimen is stained (most often with the Giemsa stain) to give the parasites a distinctive appearance. This technique remains the gold standard for laboratory confirmation of malaria. However, it depends on the quality of the reagents, of the microscope, and on the experience of the laboratorian.
More on: Diagnosis (Microscopy)
Various test kits are available to detect antigens derived from malaria parasites. Such immunologic (“immunochromatographic”) tests most often use a dipstick or cassette format, and provide results in 2-15 minutes. These “Rapid Diagnostic Tests” (RDTs) offer a useful alternative to microscopy in situations where reliable microscopic diagnosis is not available. Malaria RDTs are currently used in some clinical settings and programs. The World Health Organization is conducting comparative performance evaluations of many of the RDTs which are commercially available worldwide based on a panel of parasites derived from a global network of collection sites. Results of this testing is available at: http://www.wpro.who.int/sites/rdt/home.htm.
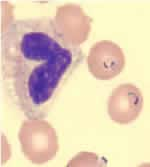
Blood smear stained with Giemsa, showing a white blood cell (on left side) and several red blood cells, two of which are infected with Plasmodium falciparum (on right side).
On June 13, 2007, the U.S. Food and Drug Administration (FDA) approved the first RDT for use in the United States. This RDT is approved for use by hospital and commercial laboratories, not by individual clinicians or by patients themselves. It is recommended that all RDTs are followed-up with microscopy to confirm the results and if positive, to confirm the species and quantify the proportion of red blood cells that are infected. The use of this RDT may decrease the amount of time that it takes to determine that a patient is infected with malaria.
More on: Diagnosis (Rapid Diagnostic Test)
Parasite nucleic acids are detected using polymerase chain reaction (PCR). Although this technique may be slightly more sensitive than smear microscopy, it is of limited utility for the diagnosis of acutely ill patients in the standard healthcare setting. PCR results are often not available quickly enough to be of value in establishing the diagnosis of malaria infection.
PCR is most useful for confirming the species of malarial parasite after the diagnosis has been established by either smear microscopy or RDT.
More on: Molecular Diagnosis of Malaria and Babesiosis
More on: Simian Malaria Species Confirmation Service (SMSCS)
Serology detects antibodies against malaria parasites, using either indirect immunofluorescence (IFA) or enzyme-linked immunosorbent assay (ELISA). Serology does not detect current infection but rather measures past exposure.
More on: Serology
Drug resistance tests must be performed in specialized laboratories to assess the susceptibility to antimalarial compounds of parasites collected from a specific patient. Two main laboratory methods are available:
In vitro tests: The parasites are grown in culture in the presence of increasing concentrations of drugs; the drug concentration that inhibits parasite growth is used as endpoint.
Molecular characterization: Molecular markers assessed by PCR or gene sequencing also allow the prediction, to some degree, of resistance to some drugs. CDC recommends that all cases of malaria diagnosed in the United States should be evaluated for evidence of drug resistance.
More on: Drug Resistance