Anthrax
What is anthrax?
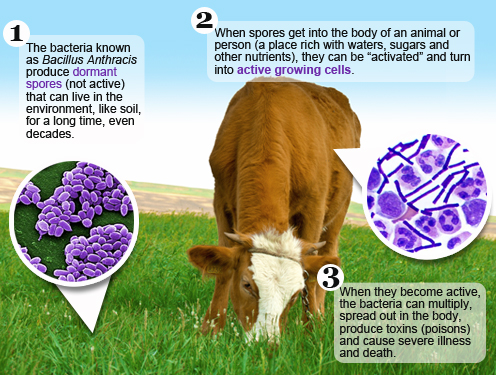
Anthrax is a serious disease caused by a bacterial organism known as Bacillus anthracis. This bacterium forms spores, a resistant form that lies dormant until the right conditions exist for them to germinate and produce vegetative cells. The type of illness a person develops depends on how anthrax enters the body. Typically, anthrax gets into the body through the skin, lungs, or gastrointestinal system. All types of anthrax can eventually spread throughout the body and cause death if they are not treated with antibiotics.
How is anthrax spread?
Anthrax is most commonly spread when humans handle products from infected animals, breathe in anthrax spores from infected animal products, or eat undercooked meat from infected animals. Anthrax has also been used as a bioweapon, when in 2001, a powder containing anthrax spores was sent to targeted individuals through the U.S. Postal System.
In very rare cases, person-to-person transmission has been reported for cutaneous anthrax. This is because discharges from skin lesions might be infectious until the patient has been on antimicrobials for a day or so. Therefore, cutaneous anthrax lesions should be kept covered for at least one day after the start of antibiotic therapy.
Is it safe for a mother to continue breastfeeding if she has been exposed to anthrax?
Usually. Clinical management of women who deliver neonates while receiving prophylaxis or treatment for anthrax does not require mother-infant separation. Because there is no evidence for anthrax transmission through human breast milk, anthrax exposure is not considered a contraindication to initiating or continuing breastfeeding or providing expressed human milk. Women with active cutaneous anthrax lesions on the breast should avoid infant contact and not breastfeed from the affected breast until after 48 hours of appropriate antimicrobial drug therapy. B. anthracis has not been isolated from cutaneous lesions 48 hours after the initiation of appropriate antimicrobial drugs; therefore, breastfeeding can resume from the affected breast after these criteria are met.
Some antibiotics are safer than others while breastfeeding. Ciprofloxacin is recommended as the first-line antimicrobial agent of choice for post-exposure prophylaxis (PEP) for asymptomatic lactating women because of the severity of inhalation anthrax. The American Academy of Pediatrics considers ciprofloxacin and tetracyclines (which include doxycycline) to be compatible with breastfeeding because infants absorb only a small amount of these drugs. Physicians may instead prescribe amoxicillin if the strain of anthrax is susceptible to penicillin and no other contraindications to the mother are present. Amoxicillin is among those drugs categorized as safe for use with infants. Health care providers should always weigh the risks and benefits when prescribing medications to breastfeeding mothers.
Learn more about antimicrobial considerations for breastfeeding women and safe prescription medication use while breastfeeding.
Is the Anthrax vaccine safe for breastfeeding mothers and their infants?
Yes. Anthrax vaccines are administered as a component of a PEP regimen, or to persons in occupations placing them at risk for exposure. There is no biologic reason to suggest that breastfeeding women or breastfed infants have an increased risk for adverse events after vaccination with anthrax vaccine absorbed (AVA) or PEP. Therefore, breastfeeding is neither a precaution nor a contraindication to vaccination in a pre- or post–anthrax event setting.
- Special Considerations for Prophylaxis for and Treatment of anthrax in Pregnant and Postpartum Women – CDC
- Pediatric Anthrax Clinical Management – American Academy of Pediatrics
- Use of Anthrax Vaccine in the United States: Recommendation of the Advisory Committee on Immunization Practices (ACIP), 2009 – CDC
