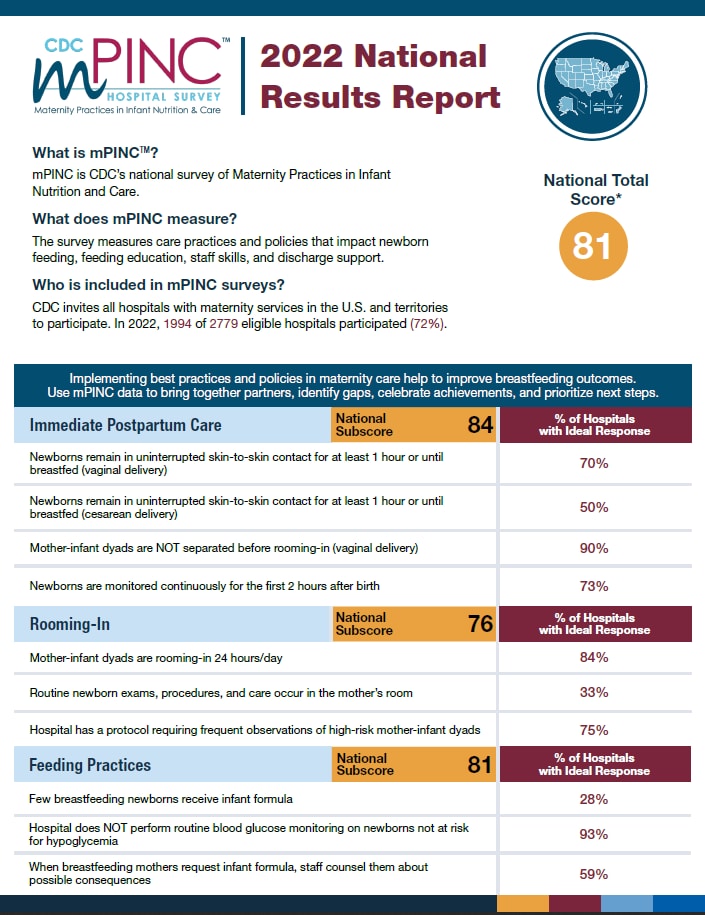
mPINC 2022 National Results Report
What is mPINC?
mPINC is CDC’s national survey of Maternity Practices in Infant Nutrition and Care.
What does mPINC measure?
The survey measures care practices and policies that impact newborn feeding, feeding education, staff skills, and discharge support.
Who is included in mPINC surveys?
CDC invites all hospitals with maternity services in the U.S. and territories to participate. In 2022, 1994 of 2779 eligible hospitals participated (72%).
National Total Score* 81
Implementing best practices and policies in maternity care help to improve breastfeeding outcomes. Use mPINC data to bring together partners, identify gaps, celebrate achievements, and prioritize next steps.
| Immediate Postpartum Care | National Subscore: 84 | % of Hospitals with Ideal Response |
|---|---|---|
| Newborns remain in uninterrupted skin-to-skin contact for at least 1 hour or until breastfed (vaginal delivery) | 70% | |
| Newborns remain in uninterrupted skin-to-skin contact for at least 1 hour or until breastfed (cesarean delivery) | 50% | |
| Mother-infant dyads are NOT separated before rooming-in (vaginal delivery) | 90% | |
| Newborns are monitored continuously for the first 2 hours after birth | 73% | |
| Rooming-In | National Subscore: 76 | % of Hospitals with Ideal Response |
| Mother-infant dyads are rooming-in 24 hours/day | 84% | |
| Routine newborn exams, procedures, and care occur in the mother’s room | 33% | |
| Hospital has a protocol requiring frequent observations of high-risk mother-infant dyads | 75% | |
| Feeding Practices | National Subscore: 81 | % of Hospitals with Ideal Response |
| Few breastfeeding newborns receive infant formula | 28% | |
| Hospital does NOT perform routine blood glucose monitoring on newborns not at risk for hypoglycemia | 93% | |
| When breastfeeding mothers request infant formula, staff counsel them about possible consequences | 59% | |
| Feeding Education & Support | National Subscore: 94 | % of Hospitals with Ideal Response |
| Mothers whose newborns are fed formula are taught feeding techniques and how to safely prepare/feed formula | 78% | |
| Breastfeeding mothers are taught/shown how to recognize/respond to feeding cues, to breastfeed on-demand, and to understand the risks of artificial nipples/pacifiers | 76% | |
| Breastfeeding mothers are taught/shown how to position and latch their newborn, assess effective breastfeeding, and hand express milk | 74% | |
| Discharge Support | National Subscore: 78 | % of Hospitals with Ideal Response |
| Discharge criteria for breastfeeding newborns requires direct observation of at least 1 effective feeding at the breast within 8 hours of discharge | 68% | |
| Discharge criteria for breastfeeding newborns requires scheduling of the first follow-up with a health care provider | 89% | |
| Hospital’s discharge support to breastfeeding mothers includes in-person follow-up visits/appointments, personalized phone calls, or formalized, coordinated referrals to lactation providers | 89% | |
| Hospital does NOT give mothers any of these items as gifts or free samples: infant formula; feeding bottles/nipples, nipple shields, or pacifiers; coupons, discounts, or educational materials from companies that make/sell infant formula/feeding products | 66% | |
| Institutional Management | National Subscore: 76 | % of Hospitals with Ideal Response |
| Nurses are required to demonstrate competency in assessing breastfeeding (milk transfer & maternal pain), assisting with breastfeeding (positioning & latch), teaching hand expression & safe formula preparation/feeding, and demonstrating safe skin-to-skin practices§ | 73% | |
| Hospital requires nurses to be formally assessed for clinical competency in breastfeeding support/lactation management | 75% | |
| Hospital records/tracks exclusive breastfeeding throughout the entire hospitalization | 92% | |
| Hospital pays a fair market price for infant formula | 54% | |
| Hospital has 100% of written policy elements§ | 32% | |
*Scores range from 0 to 100, with 100 being the best possible score. The “Total Score” is an average of the subscores for the 6 subdomains.
§See the scoring algorithm for specific items on CDC’s Maternity Care Practices scoring web page.
NOTE: The mPINC survey was redesigned in 2018. Results from the mPINC surveys 2018 and later cannot be compared with results from 2007—2015 mPINC surveys.
Questions about the mPINC survey? Visit: Maternity Practices in Infant Nutrition and Care (mPINC) Survey to learn more.
Suggested Citation: Centers for Disease Control and Prevention. 2022 National Results Report, CDC Survey of Maternity Care Practices in Infant Nutrition and Care. Atlanta, GA. 2023.