Continue to check our website for further updates on when we will reopen. When the museum reopens, all visitors will need to make reservations at least a week in advance. Walk-in visits are no longer permitted.
Teen Newsletter: Smoking
January 2022
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each newsletter focuses on a different public health topic that CDC studies. Newsletter sections: Introduction, CDC’s Work, The Public Health Approach, Out of the CDC Museum Collection, and Teen Talk.
Watch the smoking Teen Talk.
Introduction – Smoking
Tobacco use remains the leading cause of preventable disease, disability, and death in the United States, mainly in the form of cigarettes and other combustible products. As of 2019, about 34 million U.S. adults smoke cigarettes. More than 16 million people live with at least one disease caused by smoking, and 58 million nonsmoking Americans are exposed to secondhand smoke. Smoking-related illness costs society more than $300 billion each year, including $170 billion in direct medical costs. Costs could be reduced if we prevent young people from starting to smoke and help people who smoke to quit.
34 million
U.S. adults smoke cigarettes.

3.6 million
U.S. middle and high school students use tobacco products.

58 million
nonsmoking Americans are exposed to secondhand smoke.

$170 billion
is spent each year to treat smoking-related diseases.
Nearly all tobacco product use begins in adolescence, and tobacco product use among U.S. youth is increasing. More than 1 in 4 high school students and about 1 in 14 middle school students in 2018 had used a tobacco product in the past 30 days. This was a considerable increase from 2017, which was driven by an increase in e-cigarette use. E-cigarette use increased from 11.7% to 20.8% among high school students and from 3.3% to 4.9% among middle school students from 2017 to 2018. No change was found in the use of other tobacco products, including cigarettes, during this time.
Tobacco Product Use among High School Students – 2018
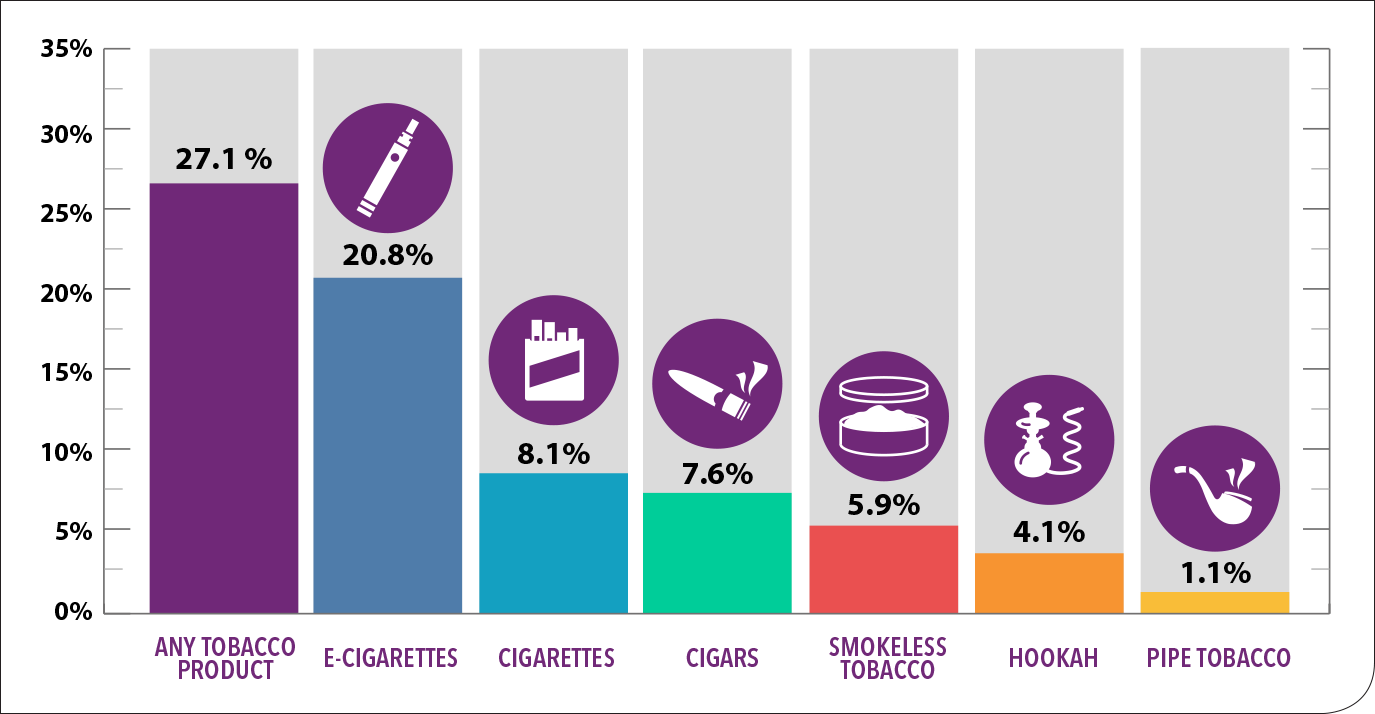
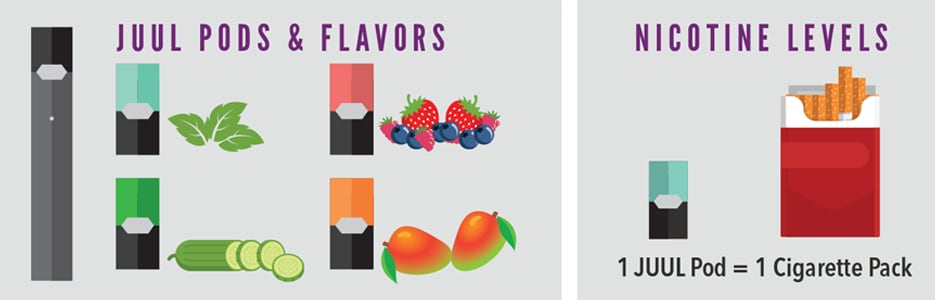
E-cigarettes are the main reason for the rise in tobacco use by youth. The increase in youth e-cigarette use happened at the same time as increased JUUL sales. JUUL is an e-cigarette shaped like a USB flash drive. It uses liquid nicotine refills called “pods,” which contain at least as much nicotine as a pack of cigarettes. Before the more recent FDA ban the available pod flavors were very appealing to youth (i.e., fruit and mint). Look for a Teen Newsletter on e-cigarette use in the coming months!
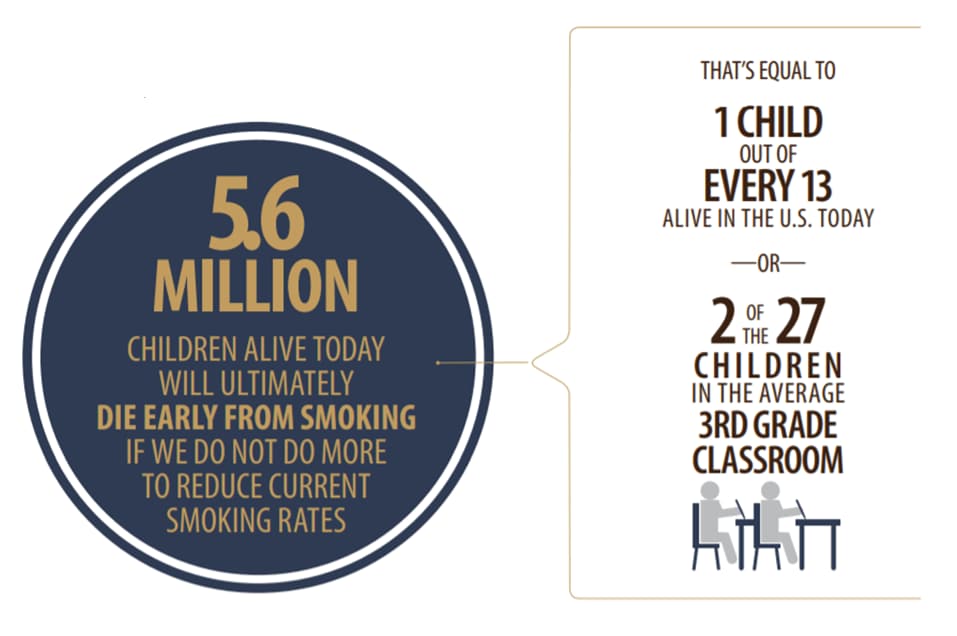
Use of any form of tobacco product by youths is unsafe. If smoking continues at current rates, 5.6 million – or 1 out of every 13 – of today’s children will ultimately die prematurely from a smoking-related illness.
What are the health consequences of smoking?
Cigarette smoking causes more than 480,000 deaths each year in the United States. This is nearly one in five deaths. Cigarette smoking has many health effects. It harms nearly every organ of the body, causes many diseases, and reduces the health of smokers in general.
Secondhand smoke is smoke from burning tobacco products, like cigarettes, cigars, hookahs, or pipes. Secondhand smoke also is smoke that has been exhaled (breathed out) by the person smoking. Exposure to secondhand smoke, even for a short time, can be harmful to both children and adults. Since 1964, about 2,500,000 people who never smoked have died from health problems caused by secondhand smoke exposure.
What are the health benefits of quitting smoking?
If nobody smoked, one of every three cancer deaths in the United States would not happen. Quitting smoking lowers your risk for smoking-related diseases and can add years to your life. While quitting earlier in life yields greater health benefits, quitting smoking is beneficial to health at any age. Even people who have smoked for many years or have smoked heavily will benefit from quitting.
CDC’s Work – Smoking
There are two programs at CDC that work together on smoking.
- National Center for Environmental Health (NCEH)
- The Tobacco Laboratory examines both individual and population exposures to the chemicals in tobacco products. This laboratory is unique because it measures toxic and addictive substances in tobacco products, in smoke and other emissions, and in people who use tobacco products or are exposed to secondhand smoke. No other laboratory in the federal government has these capabilities.
- National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP)
- Office on Smoking and Health (OSH) is the lead federal agency for comprehensive tobacco prevention and control. OSH saves lives and saves money by preventing and reducing tobacco use.
- OSH works to:
-
-
- Measure how tobacco use affects populations
- Study what works best to prevent tobacco use and help people quit tobacco use
- Provide information to the public about the dangers of tobacco use and secondhand smoke exposure
- Fund and guide states, territories, tribes, and nonprofit organizations to use evidence-based strategies
-
-
CDC’s National Tobacco Control Program (NTCP) is the only nationwide investment that supports all 50 states, the District of Columbia, 8 U.S. territories, and 27 tribal organizations for comprehensive tobacco control efforts and quitlines. States use OSH funds to prevent kids from using tobacco, reduce secondhand smoke exposure, help smokers quit, and reduce disparities in tobacco use.
The Public Health Approach – Smoking
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, and other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps.
For ease of explaining and understanding the public health approach for the public health problem of smoking and vaping, let’s focus on how West Virginia Division of Tobacco Prevention, with funding and technical support from CDC’s National Tobacco Control Program, helped people quit smoking in West Virginia.
- Surveillance (What is the problem?). In public health, we identify the problem by using surveillance systems to monitor health events and behaviors occurring among a population.
Cigarette smoking is the leading cause of preventable disease and death in the United States, accounting for about 480,000 deaths every year (about 1 in 5 deaths). Nationally, an estimated 14% of adults currently smoke cigarettes, and more than 16 million Americans live with a smoking-related disease.
CDC’s Office of Smoking and Health (OSH) conducts and supports national and international surveys on tobacco use, smoking cessation, secondhand smoke exposure, and other tobacco-related topics among youth, adults, and specific populations. One survey is the Behavior Risk Factor Surveillance System (BRFSS). BRFSS is the nation’s premier system of health-related telephone surveys that collects state data about U.S. residents regarding their health-related risk behaviors, chronic health conditions, and use of preventive services.
According to an analysis of the 2016 BRFSS, nearly 25% of West Virginia adults were cigarette smokers – the highest percentage of any state in the country. The West Virginia Division of Tobacco Prevention, part of the state’s Department of Health & Human Services, wanted to look for new ways to lower the number of West Virginia adults who smoke tobacco.
- Risk Factor Identification (What is the cause?). After we’ve identified the problem, the next question is, “What is the cause of the problem?” For example, are there factors that might make certain populations more susceptible to disease, such as something in the environment or certain behaviors that people are practicing?
Data from BRFSS showed that Cigarette smoking remains high among certain groups in the United States.
- Intervention Evaluation (What works?). Once we’ve identified the risk factors related to the problem, we ask, “What intervention works to address the problem?” We look at what has worked in the past in addressing this same problem and if a proposed intervention makes sense with our affected population.
Quitting smoking is one of the most important actions people can take to improve their health. This is true regardless of their age or how long they have been smoking.
The Tobacco Prevention program staff knew that pharmacists can play a key role in promoting health by counseling people on how to quit using tobacco products and by providing nicotine replacement therapies like patches or gum. Counseling and nicotine replacement therapies are proven, effective ways to help smokers quit.
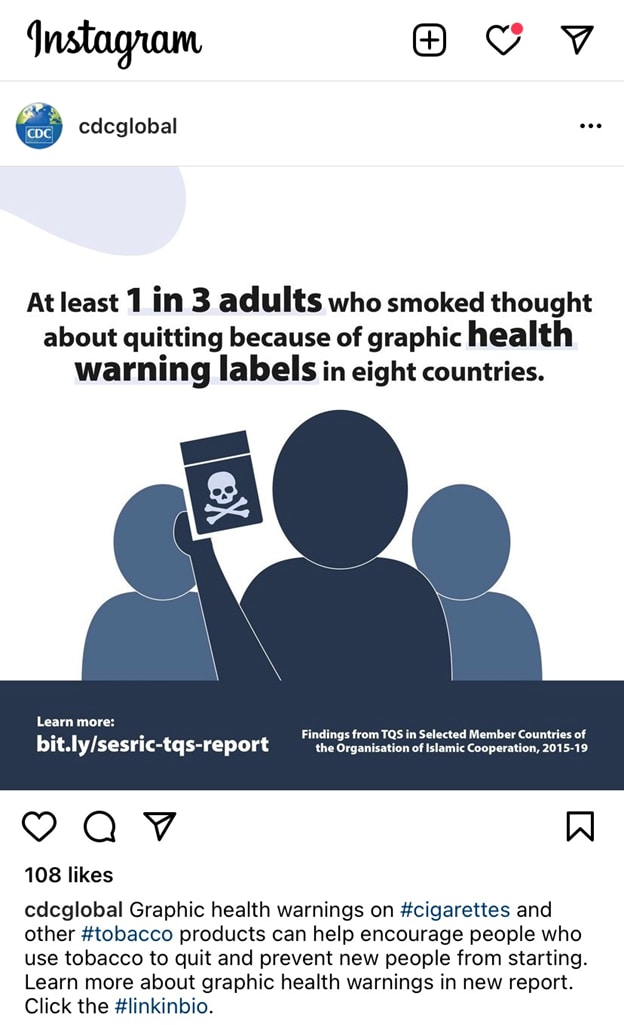
While not specific to the West Virginia case study, here is another great example that was shared last month on Instagram. Research shows that graphic health warning labels work too.
- Implementation (How do we do it?). In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”
The Tobacco Prevention program staff decided to work more closely with small pharmacies in rural counties to reduce tobacco use among West Virginians. Creative Pharmacist (now known as STRAND Clinical Technologies) now works with pharmacists in more than 1,000 independent pharmacies to help patients manage their chronic health conditions. Creative Pharmacist shows CDC’s Tips From Former Smokers® (Tips®) ads on TVs in these pharmacies—reaching more than 2 million customers in 2 years—to motivate smokers to consider quitting and ask a pharmacist for advice.
The Tobacco Prevention program and Creative Pharmacist created a pilot program to help people quit smoking. The program focused on small pharmacies in 5 rural counties with high smoking rates. As part of the program, pharmacists:
- Talked to people who smoked about trying to quit smoking.
- Hosted counseling and group support sessions.
- Taught people who smoked about the benefits of nicotine replacement therapy— like patches or gum.
- Used Tips® ads and other materials to educate people.
- Sent text messages about quitting.
- Told people who smoked about services offered by the West Virginia Tobacco Quitline, including free phone counseling and 8 weeks of free nicotine replacement therapy.
The pilot program created by this public-private partnership between the Tobacco Prevention program and pharmacies has helped West Virginians quit smoking. Fifty adults who smoked cigarettes enrolled in the program. Within 10 weeks of launching the program, 40% of the enrolled clients had quit smoking, and one-third of the 40% remained quit at 24 weeks. The program was expanded, with an additional 8 rural pharmacies enrolling 110 clients, 30 of whom had quit cigarette smoking within 12 weeks. The program continues to be evaluated and enhanced.
The partnership between Tobacco Prevention staff, Creative Pharmacist, and pharmacists in rural counties helped place Tips® television ads and other materials related to quitting in rural pharmacies. When people who smoke see the messages, they can turn to their local pharmacists for advice on how to quit smoking. As a result of this program, pharmacists have built stronger relationships with West Virginians who smoke and are seen as trusted counselors who are willing and able to help people quit smoking. Tobacco Prevention staff, who are supported with CDC funding and received technical assistance from CDC for this project, are finding new ways to reduce tobacco use in West Virginia.
Using the Public Health Approach helps public health professionals identify a problem, find out what is causing it, and determine what solutions/interventions work.
Out of the CDC Museum Collection – Smoking
This month’s Out of the CDC Museum Collection relates to the CDC’s Work section above. Remember learning about the CDC Tobacco Laboratory? Below is an image of a smoking machine that was used in the Tobacco Lab for almost eight years, pretty cool right? It was added to the museum collection in 2013.

Harmonized 8 Channel Smoking Machine (1994) that was used by the CDC Tobacco Laboratory till the early 2000s.
Want to see a smoking machine in action? Watch the short video clip below to see a CDC laboratory scientist prepare and use a smoking machine for cigarette analysis. The smoking machine captures smoke particulate on a pad which provides information on exposures to harmful chemicals in tobacco smoke.