Continue to check our website for further updates on when we will reopen. When the museum reopens, all visitors will need to make reservations at least a week in advance. Walk-in visits are no longer permitted.
Teen Newsletter: Concussions
August 2022
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each newsletter focuses on a different public health topic that CDC studies. Newsletter sections: Introduction, CDC’s Work, The Public Health Approach, and Out of the CDC Museum Collection.
A concussion is a type of traumatic brain injury—or TBI—caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement can cause the brain to bounce around or twist in the skull, creating chemical changes in the brain and sometimes stretching and damaging brain cells.
Medical providers may describe a concussion as a “mild” brain injury because concussions are usually not life-threatening. Even so, the effects of a concussion can be serious. Signs and symptoms generally show up soon after the injury. However, you might not know how serious the injury is at first and some symptoms may not show up for hours or days.
As symptoms improve, you may gradually return to regular activities. Recovery from a mild TBI or concussion means you can do your regular activities without experiencing symptoms. Recovery may be slower among:
- Older adults
- People who have had a concussion or other TBI in the past
- Teens
- Young children
Concussions can have a serious effect on a young, developing brain, causing short- and long-term problems affecting a child’s thinking, language, learning, behavior, and/or emotions. A successful recovery from a concussion starts with a correct response to the injury. Most children with a concussion feel better within a couple of weeks. However, for some, symptoms will last for a month or longer. Nevertheless, making short-term changes to a child’s daily activities can help him or her get back to a regular routine more quickly. It is important to take progressive steps towards normality, as each concussion and each child is unique.
Oftentimes, children recovering from concussions do not experience issues with schooling. Most kids and teens will only need help through informal, academic adjustments as they recover from a concussion. However, for kids and teens with ongoing symptoms, a variety of formal support services may be available to help them during their recovery such as Response to Intervention Protocol (RTI), 504 Plan, and Individualized Education Plan (IEP). The return to sports and activities is a gradual process that one must perform under the supervision of a health care provider.
There are many ways to help reduce the risk of a concussion or other serious brain injury both on and off the sports field, including using age- and size-appropriate car seats, wearing the right helmet, using gates at the top/bottom of stairs to prevent serious falls, and playing on soft surfaces such as mulch and sand. It is important to take proper precautions to prevent brain injuries.
CDC’s National Center for Injury Prevention and Control (NCIPC) is the center responsible for working on concussions. They lead innovative research and science-based programs to prevent injuries and violence and to reduce their consequences. NCIPC’s Division of Injury Prevention has three branches. The Applied Sciences Branch focuses on four public health topics, one being traumatic brain injury. If you recall from the Introduction section (hyperlink “Introduction section” via anchor tags), a concussion is a type of traumatic brain injury.
CDC Programs and Resources on Traumatic Brain Injury & Concussion:
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, as well as other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps.
For ease of explaining and understanding the public health approach for the public health problem of concussions, let’s focus on how rates of concussions among young athletes decreased over the years with guidance from CDC.
- Surveillance (What is the problem?). In public health, we identify the problem by using surveillance systems to monitor health events and behaviors occurring among a population.
The Youth Risk Behavior Surveillance System (YRBSS) monitors a variety of health-related behaviors that contribute to the leading causes of death and disability among youth, including how many high school students had a concussion from playing a sport or being physically active in the previous 12 months.
The Traumatic Brain Injury (TBI) Surveillance Report uses data collected from multiple sources (i.e., Healthcare Cost and Utilization Project’s National Inpatient Sample and National Vital Statistics System) to describe the national incidence estimates of TBI-related hospitalizations and deaths by age group, principal mechanism of injury, injury intent, and sex.
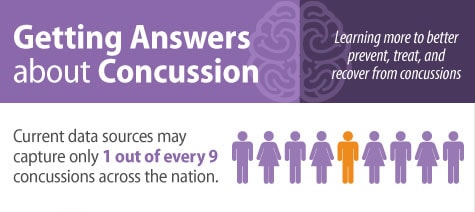
Want to learn more about concussion surveillance? Check out the National Concussion Surveillance System that is currently being tested.
This state-of-the-art surveillance system will be able to accurately determine how many Americans (children and adults) get a concussion each year and determine the cause. In addition, the results of a national system would inform and equip leaders within communities and states across the U.S.
- Risk Factor Identification (What is the cause?). After we’ve identified the problem, the next question is, “What is the cause of the problem?” For example, are there factors that might make certain populations more susceptible to diseases, such as something in the environment or certain behaviors that people are practicing?
Traumatic brain injuries (TBIs), including concussions, are caused by an impact to the head or body. Physiologic factors (such as a child’s developing nervous system and thinner cranial bones) might place children at increased risk for TBIs. Developing brains of children/adolescents are more vulnerable to Mild Traumatic Brain Injuries (mTBI) because their axons are not well-myelinated, meaning cells in the brain are not well protected, and they are more susceptible to chemical and metabolic changes.
Overall, youth are among those at greatest risk for concussion: studies have demonstrated that 70% of emergency department visits for sports and recreation-related TBIs were among kids and teens. Activities associated with the highest number of emergency department visits for concussions are football, bicycling, basketball, playground activities, and soccer.
A CDC study published in Sports Health reports youth tackle football athletes ages 6 to 14 sustained 15 times more head impacts than flag football athletes during a practice or game and sustained 23 times more high-magnitude head impacts (hard head impacts).
- Intervention Evaluation (What works?). Once we’ve identified the risk factors related to the problem, we ask, “What intervention works to address the problem?” We look at what has worked in the past in addressing this same problem and if a proposed intervention makes sense with our affected population.
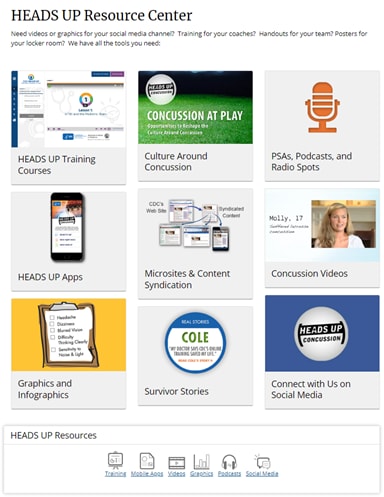
CDC’s HEADS UP initiative includes educational trainings and materials that were created to protect children and teens by raising awareness and informing action to improve prevention, recognition, and response to concussions and other serious brain injuries.
Specifically, CDC HEADS UP works to improve prevention, recognition, and response to concussions and other serious brain injuries through:
CDC collaborated with multiple organizations and leading experts to develop recommendations, guidelines, and tools for diagnosis and management of patients with concussions and Mild Traumatic Brain Injuries (mTBI). Below are a couple of examples:
- Six gradual steps to help safely return an athlete to play.
- Pediatric mTBI Guideline
Key recommendations from this guideline include:
- Do not routinely image patients to diagnose mTBI.
- Use validated, age-appropriate symptom scales to diagnose mTBI.
- Assess evidence-based risk factors for prolonged recovery.
- Provide patients with instructions on return to activity customized to their symptoms.
- Counsel patients to return gradually to non-sports activities after no more than 2-3 days of rest.
Baseline testing is another example of an intervention. It is used to assess an athlete’s balance and brain function as well as for the presence of any concussion symptoms. Results from baseline tests (or pre-injury tests) can be used and compared to a similar exam conducted by a health care professional during the season if an athlete has a suspected concussion. Comparing post-injury test results to baseline test results assists health care professionals in identifying the effects of the injury and making more informed return to school and play decisions.
- Implementation (How did we do it?). In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”.
CDC is committed to finding answers for Americans concerned about concussions and other traumatic brain injuries (TBI). CDC partners with many organizations to get HEADS UP concussion materials into the hands of many people, such as parents, health care and school professionals, coaches, and athletes.
CDC recognizes that a strong focus on health and safety in sports can help keep young athletes safe. CDC created the “Concussion at Play: Opportunities to Reshape the Culture Around Concussion” report to provide a snapshot of current research on concussion knowledge, awareness, attitudes, and behaviors. The report includes potential strategies to help keep athletes safe by building a culture in sports to lower their chances of getting a concussion and recognize and report concussion symptoms so that they can seek care and take time to recover.
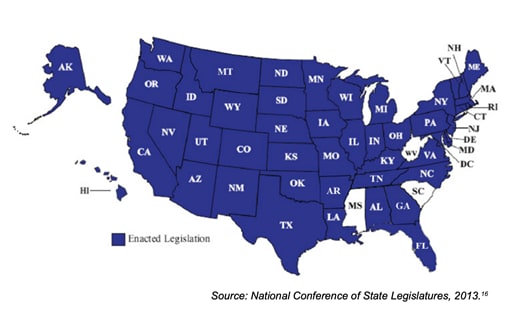
To limit the rising rate of concussions, many states, schools, and sports leagues and organizations have created policies or action plans on concussion in youth and high school sports.
In 2009, the state of Washington passed the first concussion in sports law, called the Zackery Lystedt Law. This law asserts that individuals who are suspected of having a concussion are not permitted to reenter play again until they are cleared by a healthcare provider. Similar to the Zackery Lystedt Law is Max’s Law, which establishes many guidelines a coach must follow if an athlete presents the symptoms of a concussion.
In total, between 2009 and 2012, 43 states and the District of Columbia passed laws on concussion in sports for youth and/or high school athletes, often called Return to Play Laws.
The requirements of Return to Play laws vary but typically include some combination of the following:
- Mandatory removal from play
- Mandatory bench times
- Required medical clearance
- Required training/education for coaches, parents, and athletes
- Informed consent of parents and athletes
Most concussion in sports laws include three action steps:
- Educate coaches, parents, and athletes: inform and educate coaches, athletes, and their parents and guardians about concussion through training and/or a concussion information sheet.
- Remove athlete from play: an athlete who is believed to have a concussion is to be removed from play right away.
- Obtain permission to return to play: an athlete can only return to play or practice after at least 24 hours and with permission from a healthcare professional.
Using The Public Health Approach helps public health professionals identify a problem, find out what is causing it, and determine what solutions/interventions work.
This month’s Out of CDC Museum Collection relates to the CDC’s Work section that highlights CDC HEADS UP. CDC works to get HEADS UP concussion materials into the hands of many people, such as parents, health care and school professionals, coaches, and athletes.
Below you will find two different posters designed to be displayed in places such as doctors’ offices and school gyms. These posters have played a monumental role in raising awareness and informing action to improve prevention, recognition, and response to concussions and other serious brain injuries.

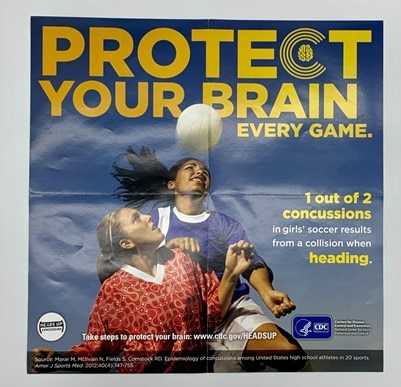
These posters mark a historical shift in concussion initiatives, moving from previously only informing healthcare workers to more recent HEADS UP initiatives also focusing on sports programs and schools as key places to share concussion information with coaches, parents, and school professionals.
HEADS UP posters are hung up at sports and recreation facilities in communities and at schools. Whether large or small, a difference can be made in educating communities about concussions and keeping young athletes safe through the HEADS UP effort.