Continue to check our website for further updates on when we will reopen. When the museum reopens, all visitors will need to make reservations at least a week in advance. Walk-in visits are no longer permitted.
Teen Newsletter: May 2021 – Fetal Alcohol Spectrum Disorders (FASDs)
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each month will focus on a different public health topic that CDC studies. Newsletter sections: Introduction, CDC’s Work, The Public Health Approach, Special Feature, Out of the CDC Museum Collection, and Activities.
Be sure to join our live Newsletter Zoom on May 25, 2021, at 8pm ET, and check out all the activities (digital scavenger hunt—Goosechase, Zoom, social media challenge, and Ask a CDCer) at the end of each newsletter. Join in on the fun and win some prizes! Also, be on the lookout for the recently added activity, a pre-Zoom game (Kahoot) that will be emailed the day of the Zoom.
Introduction – Fetal Alcohol Spectrum Disorders (FASDs)

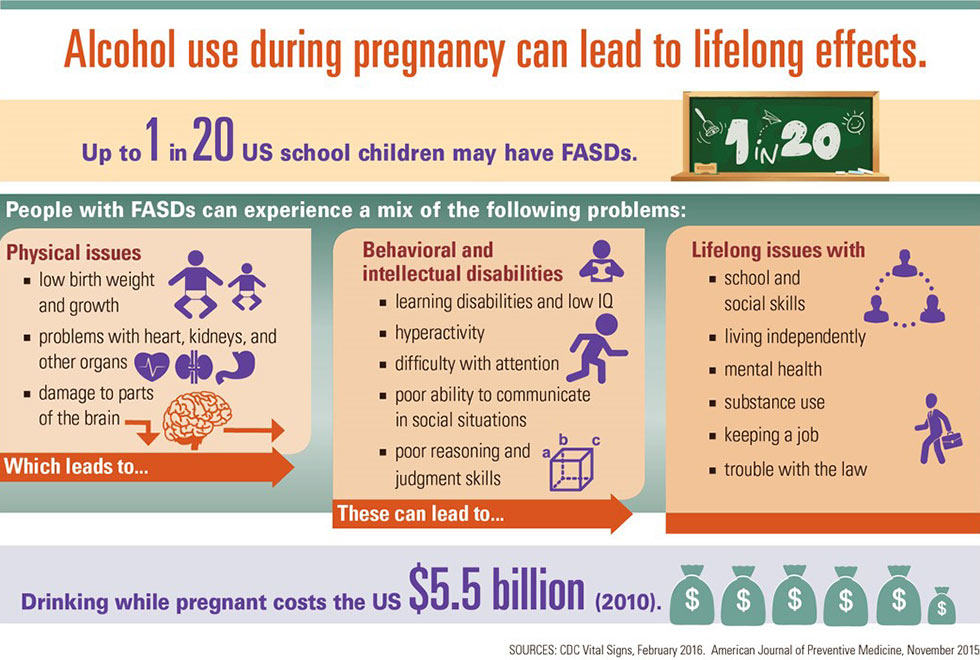
Fetal alcohol spectrum disorders (FASDs) are a group of conditions that can occur in a person who was exposed to alcohol before birth. These effects can include physical problems and problems with behavior and learning. Often, a person with an FASD has a mix of these problems.
A developing baby can be exposed to the same level of alcohol as the mother during pregnancy.
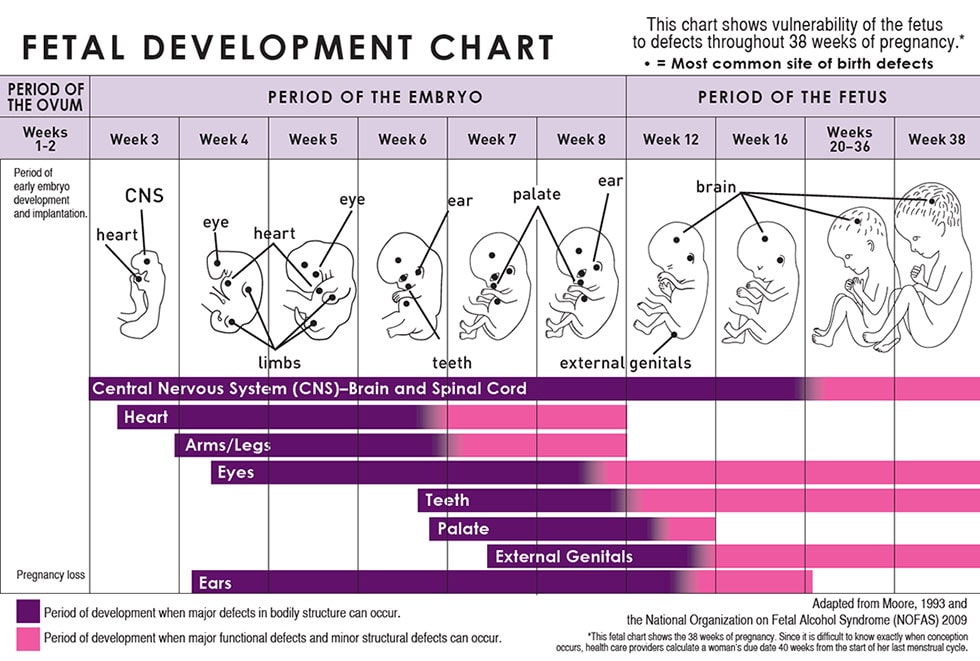
There is no known safe amount of alcohol during pregnancy or when trying to get pregnant. There is also no safe time to drink during pregnancy. Alcohol can cause problems for a developing baby throughout pregnancy, including before a woman knows she’s pregnant. All types of alcohol are equally harmful, including all wines and beer.
FASDs are preventable if a developing baby is not exposed to alcohol before birth.
If a woman is drinking alcohol during pregnancy, it is never too late to stop drinking. Because brain growth takes place throughout pregnancy, the sooner a woman stops drinking the better it will be for her and her baby. Resources are available.
FASDs can affect each person in different ways, and can range from mild to severe.
Diagnosing FASDs can be hard because there is no medical test, like a blood test, for these conditions. And other disorders, such as ADHD (attention-deficit/hyperactivity disorder) and Williams syndrome, have some symptoms like fetal alcohol syndrome.
Different FASD diagnoses are based on particular symptoms and include:
- Fetal Alcohol Syndrome (FAS): FAS represents the most involved end of the FASD spectrum. People with FAS have central nervous system (CNS) problems, abnormal facial features (such as a smooth ridge between the nose and upper lip – this ridge is called the philtrum), and growth problems. People with FAS can have problems with learning, memory, attention span, communication, vision, or hearing. They might have a mix of these problems. People with FAS often have a hard time in school and trouble getting along with others.
- Alcohol-Related Neurodevelopmental Disorder (ARND): People with ARND might have intellectual disabilities and problems with behavior and learning. They might do poorly in school and have difficulties with math, memory, attention, judgment, and poor impulse control.
- Alcohol-Related Birth Defects (ARBD): People with ARBD might have problems with the heart, kidneys, or bones or with hearing. They might have a mix of these.
- Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE): A child or youth with ND-PAE will have problems in three areas: (1) thinking and memory, where the child may have trouble planning or may forget material he or she has already learned, (2) behavior problems, such as severe tantrums, mood issues (for example, irritability), and difficulty shifting attention from one task to another, and (3) trouble with day-to-day living, which can include problems with bathing, dressing for the weather, and playing with other children. In addition, to be diagnosed with ND-PAE, the mother of the child must have consumed more than minimal levels of alcohol before the child’s birth, which APA defines as more than 13 alcoholic drinks per month of pregnancy (that is, any 30-day period of pregnancy) or more than 2 alcoholic drinks in one sitting.
FASDs last a lifetime. There is no cure for FASDs, but research shows that early intervention treatment services can improve a child’s development.
There are many types of treatment options, including medication to help with some symptoms, behavior and education therapy, parent training, and other alternative approaches. No one treatment is right for every child. Good treatment plans will include close monitoring, follow-ups, and changes as needed along the way.
Protective factors can help reduce the effects of FASDs and help people with these conditions reach their full potential.
Protective factors include:
- Diagnosis before 6 years of age
- Loving, nurturing, and stable home environment during the school years
- Absence of violence
- Involvement in special education and social services
CDC’s Work – Fetal Alcohol Spectrum Disorders (FASDs)
CDC’s National Center on Birth Defects and Developmental Disabilities (NCBDDD) works to address substance use (e.g., alcohol) during pregnancy. NCBDDD also works to improve care for affected individuals (e.g., people who have FASDs) and their families. More specifically, within NCBDDD is the Division of Birth Defects and Infant Disorders (DBDID) and within DBDID is the Infant Outcomes Monitoring, Research, and Prevention Branch. Work within this branch includes 1) monitoring alcohol use, 2) preventing alcohol use during pregnancy, and 3) educating families, professionals, and the public.
1. Monitoring Alcohol Use
CDC monitors alcohol use among women of childbearing age in the United States. These data are important to help reduce alcohol-exposed pregnancies by identifying groups of women at increased risk and designing prevention programs aimed at reducing risk behaviors and improving pregnancy outcomes.
2. Preventing Alcohol Use During Pregnancy
CDC works to prevent alcohol use during pregnancy by conducting research studies and implementing and disseminating evidence-based interventions for women at risk of an alcohol-exposed pregnancy. CDC also supports education and training activities for various audiences.
3. Educating Families, Professionals, and the Public
CDC educates families, professionals, and the public by supporting trainings for medical and allied health students and practitioners, promoting screening and intervention tools for women’s health care providers, promoting educational materials to various audiences, and responding to public inquiries.
The Public Health Approach – Fetal Alcohol Spectrum Disorders (FASDs)
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, as well as other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps.
1. Surveillance (What is the problem?)
In public health, we identify the problem by using surveillance systems to monitor health events and behaviors occurring among a population.
We unfortunately do not know exactly how many people have FASDs. Why is that, you ask? As you learned in the introduction, diagnosing FASDs can be hard because there is no medical test for these conditions; there are several diagnoses related to exposure of the baby to alcohol during pregnancy; and other non-alcohol disorders have similar symptoms.
Several different approaches have been used to estimate how many persons are living with FASDs in the population.
- Using medical and other records, CDC studies have identified 0.2 to 1.5 infants with FAS for every 1,000 live births in certain areas of the United States. The most recent CDC study analyzed medical and other records and found FAS in 0.3 out of 1,000 children from 7 to 9 years of age.
- Studies using in-person assessment of school-aged children in several U.S. communities report higher estimates of FAS: 6 to 9 out of 1,000 children.
- Few estimates for the full range of FASDs are available. Based on the National Institutes of Health-funded community studies using physical examinations, experts estimate that the full range of FASDs in the United States and some Western European countries might number as high as 1 to 5 per 100 school children (or 1% to 5% of the population).
CDC works with partners across the country to develop systems to monitor FASD exposures and outcomes. One way they monitor exposures is through existing national datasets to learn more about alcohol attitudes and drinking patterns among women of childbearing age, and alcohol screening and brief intervention (SBI) practices among healthcare providers. These data systems include Behavioral Risk Factor Surveillance System (BRFSS), National Survey of Family Growth (NSFG), National Ambulatory Medical Care Survey (NAMCS), and DocStyles.
The BRFSS is an ongoing, state-based, random-digit-dialed telephone survey. To determine the potential number of women at risk for an alcohol-exposed pregnancy, data from the BRFSS are analyzed for women aged 18–44 years in all 50 states. Women are asked about their use of alcohol during the 30 days before the survey.
The following patterns of alcohol drinking are examined
- Any alcohol use (one or more drinks)
- Binge drinking (4 or more drinks on any one occasion)
For example, let’s say we want to study alcohol use and binge drinking for pregnant women aged 18–44 years. This 2019 Morbidity and Mortality Weekly Report (MMWR) analyzed self-reported data from the 2015–2017 BRFSS for all 50 states and the District of Columbia.
From these data, you will find that approximately 11.5% of pregnant women reported current drinking, and among those, about one third reported binge drinking in the past 30 days.
Among pregnant women who binge drink, the average frequency of binge drinking in the past 30 days was 4.5 episodes, and the average intensity of binge drinking (the average largest number of drinks reported consumed on any occasion among binge drinkers) was 6.0 drinks.
2. Risk Factor Identification (What is the cause?)
After we’ve identified the problem, the next question is, “What is the cause of the problem?” For example, are there factors that might make certain populations more susceptible to disease, such as something in the environment or certain behaviors that people are practicing?
FASDs can occur when an individual is exposed to alcohol before birth. Alcohol in the mother’s blood passes to the baby through the umbilical cord. Alcohol can harm a baby at any time during pregnancy. FASDs are preventable if a developing baby is not exposed to alcohol before birth.
To link back to our example from the surveillance section above, let’s look at a 2013 study where researchers conducted 20 focus groups with 149 women of reproductive age. While women recognized the risks and consequences of drinking alcohol during pregnancy, many still held common misconceptions.
- Some women reported that certain kinds of alcohol are okay to drink during pregnancy and that drinking in the third trimester (last 3 months of pregnancy) did not harm the developing baby.
- Others thought that drinking small amounts of alcohol during pregnancy was acceptable and some said that their healthcare providers agreed that it was okay to drink small amounts.
- Some women continued to drink alcohol during pregnancy or said that they intended to continue drinking until it was confirmed that they were pregnant.
3. Intervention Evaluation (What works?)
Once we’ve identified the risk factors related to the problem, we ask, “What intervention works to address the problem?” We look at what has worked in the past in addressing this same problem and if a proposed intervention makes sense with our affected population.
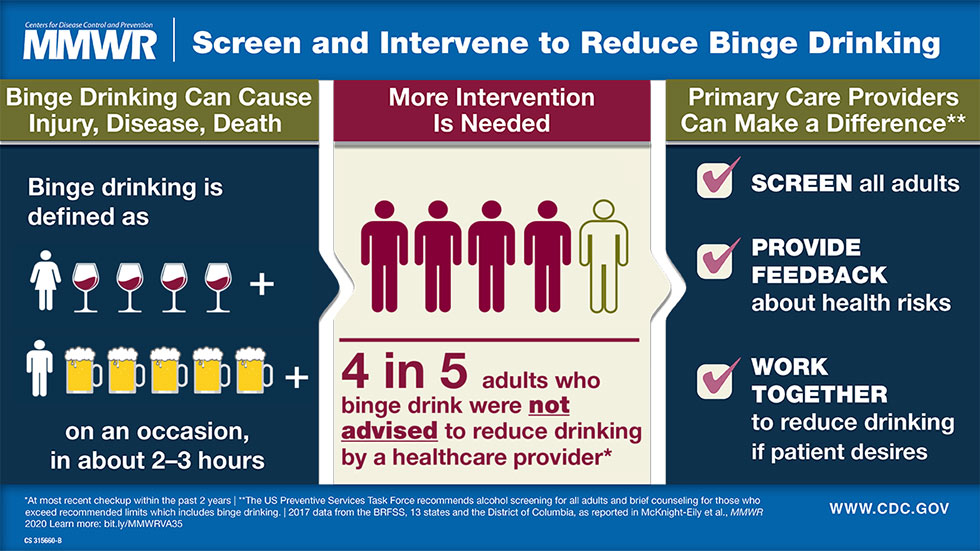
A woman’s partner, family, and friends influence her decisions whether or not to drink alcohol during pregnancy. Healthcare providers and the Internet act as important sources of health information for women, but do not always provide consistent information about the risks of alcohol use during pregnancy. Routine alcohol screening and brief counseling works and is cost-effective (good value for the amount of money that it costs).
What Can Be Done to Prevent Fetal Alcohol Spectrum Disorders?
Women can
- Talk with their healthcare providers about their plans for pregnancy, their alcohol use, and ways to prevent pregnancy if they are not planning to get pregnant.
- Stop drinking alcohol if they are trying to get pregnant or could get pregnant.
- Ask their respective partners, families, and friends to support their choice not to drink during pregnancy or while trying to get pregnant.
- Ask their healthcare providers or other trusted people about resources for help if they cannot stop drinking on their own.
Healthcare providers can
- Screen all adult patients for alcohol use at least yearly.
- Advise women not to drink at all if there is any chance they could be pregnant.
- Counsel, refer, and follow up with patients who need more help.
- Use the correct billing codes so that alcohol screening and counseling is reimbursable.
CDC has two strategies to reduce the number of alcohol-exposed pregnancies.
The first is Alcohol screening and brief intervention (SBI), which is an effective but underused preventive health service recommended by the U.S. Preventive Services Task Force and covered under the Affordable Care Act. Similar to hypertension or cholesterol screening, alcohol SBI can occur as part of a patient’s wellness visit. It involves
- A validated set of screening questions to identify a patient’s drinking patterns, which takes only a few minutes.
- A short conversation with patients who are drinking too much, and referral to specialized treatment as appropriate.
CDC has developed an Alcohol SBI Implementation Guide to help staff in primary care practices plan and implement alcohol SBI to reduce alcohol use. The guide also presents information on risky alcohol use and how it can be addressed through alcohol SBI.
The second it CHOICES, which is a counseling intervention program for non-pregnant women that helps them moderate their drinking, use contraception effectively, or both.
What if you think someone could have an FASD? They need a specialist (someone who knows about FASDs), such as a developmental pediatrician, child psychologist, or clinical geneticist. In some cities, there are clinics whose staff have special training in diagnosing and treating children with FASDs. For providers and clinics in your area, visit the National and State Resource Directory from the FASD United. It is very important to get help for FASDs as early as possible so that a child can reach his or her full potential!
4. Implementation (How did we do it?)
In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”
Education and awareness among women and health care professionals about the risks of alcohol use during pregnancy continue to be important to prevent alcohol-exposed pregnancies and FASDs.
Routine alcohol screening and brief counseling is recommended for all adults during routine clinic visits with their primary healthcare providers. Continued efforts are needed to increase adoption of alcohol screening and brief counseling by healthcare providers to reduce risky alcohol use among adults.
Considerations for messaging and educational materials related to alcohol use and pregnancy include providing clear and consistent messaging (especially from healthcare professionals), focusing on social support strategies, and utilizing electronic media.
As you can see, using The Public Health Approach helps public health professionals identify a problem, find out what is causing it, and determine what solutions/interventions work.
Special Feature – Fetal Alcohol Spectrum Disorders (FASDs)
Real Stories from People living with FASDs: Brenna’s Story

Heather and her husband Jason adopted Brenna and her three siblings from foster care. Weighing just 4 pounds and 13 ounces at birth, Brenna was so small that she came home wearing a doll’s clothes.
For years, Brenna’s parents struggled to get her accurately diagnosed. She had been slow to reach many milestones as an infant and participated in early childhood services for speech and physical therapy. She was small for her age throughout elementary school. Brenna also struggled academically. She had trouble staying on task, getting easily frustrated, and having outbursts and tantrums both in school and at home.
Brenna’s older sister was the first of the children to be diagnosed with an FASD; Brenna was diagnosed later at the age of 12 years. Deciding if a child has an FASD takes both a physical and developmental evaluation. Since there is no biological test to diagnose FASDs, clinicians must assess a child’s exposure history, behavioral and intellectual function as well as look for neurological and physical features. Also, many other disorders have similar symptoms which must be ruled out. Among several other tests, Brenna’s evaluation included an independent living/life skills test.
Benefits of a Diagnosis
According to Brenna’s mother, Heather, “Getting the diagnosis helped understand where Brenna was coming from.” Heather said that it helped them reframe the challenges they faced. It wasn’t that Brenna was being defiant or wouldn’t do things they asked of her, but rather that Brenna couldn’t do it or lacked the skills and ability. They had to give Brenna the space and time to do it.
Heather also commented that, “It was helpful to get the diagnosis since it made available many resources in our area, including a support group. Being part of the support group has helped us learn more about FASDs. It is a relief to know there are other children with similar issues, who, for instance, must also be reminded of personal hygiene, even though they are almost in high school.” The diagnosis also helps explain why Brenna could be disruptive in school, as the classes might be too hard for her to follow.
In addition to the support group, the diagnosis helped Brenna get access to local services and ensured the school system had the information they needed to best support her.
Increasing Awareness in Her Community

Brave and cheerful, Brenna has been instrumental in increasing awareness about FASDs in her school. After her diagnosis, she proudly wore her FASD T-shirt depicting a strong woman and handed out buttons and flyers about this condition. Her mother says, “I was a bit worried, wondering if she would be able to handle the comments or teasing, but Brenna did great!”
Brenna is a kind and happy teen. She loves helping people and cares about her friends and is always checking up on them. She also calls and checks on her grandmother daily.
Brenna enjoys playing the piano and being in the choir. She also recently took up junior varsity color guard and is looking forward to the competitions.
CDC would like to give a special thanks to Brenna and her family and the FASD United for sharing this story with us.
Read other real stories from people living with FASDs.
Out of the CDC Museum Collection – Fetal Alcohol Spectrum Disorders (FASDs)
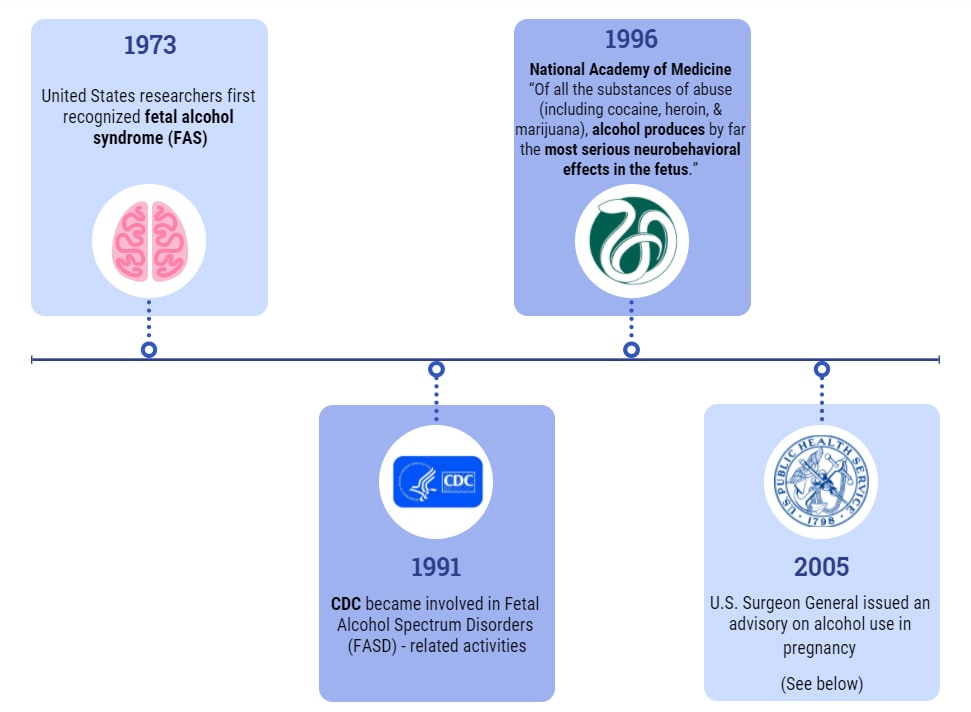
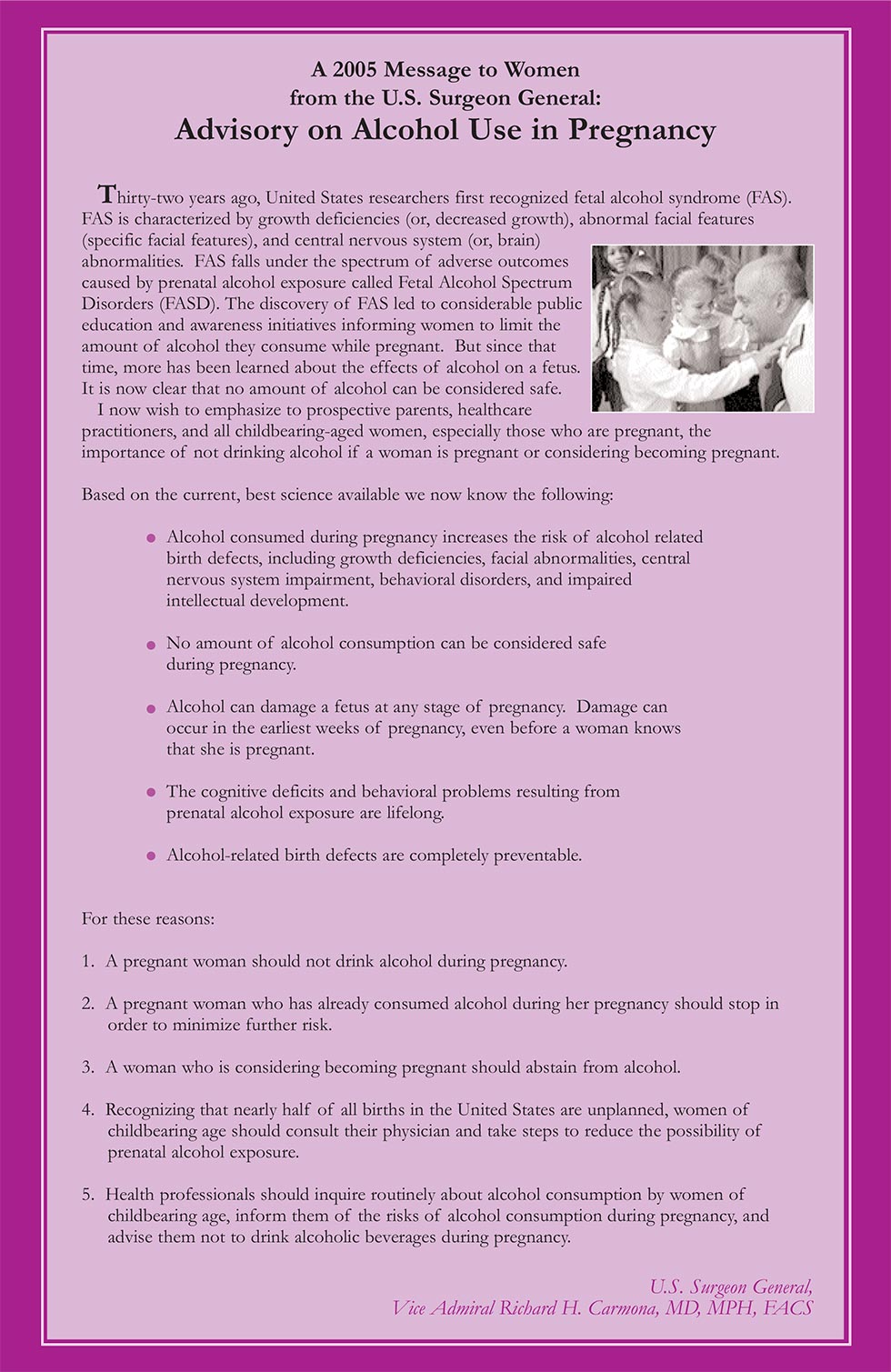
This month we are featuring an advisory on alcohol use in pregnancy message from the U.S. Surgeon General in 2005, Vice Admiral Richard H. Carmona, MD, MPH, FACS.
Forty-eight years ago (1973), United States researchers first recognized fetal alcohol syndrome (FAS). As you learned above in the introduction, FAS is characterized by growth deficiencies (or, decreased growth), abnormal facial features (specific facial features), and central nervous system (or, brain) abnormalities. FAS falls under the spectrum of adverse outcomes caused by prenatal alcohol exposure called fetal alcohol spectrum disorders (FASDs). The discovery of FAS led to considerable public education and awareness initiatives informing women to limit the amount of alcohol they consume while pregnant. But since that time, more has been learned about the effects of alcohol on a fetus. It is now clear that no amount of alcohol can be considered safe during pregnancy.
Below are a couple of quick stops in history related to FASDs, including the advisory on alcohol use in pregnancy message from the U.S. Surgeon General in 2005. Explore other important public health moments in history on the CDC Timeline.
Newsletter Activities
All May 2021 Teen Newsletter winners will be announced 05/25/21 during the Zoom – see individual deadlines below, as applicable.
Don’t forget! The CDC Museum Public Health Academy Teen Newsletter has the newsletter activity prize category: Future CDCer
To qualify for Future CDCer, you must participate in all newsletter activities (scavenger hunt—Goosechase, Zoom, social media challenge, Ask a CDCer, and pre-Zoom game—Kahoot). All that qualify will be entered into a prize drawing for a CDC Museum Public Health Academy t-shirt.
*The following newsletter activities: Scavenger Hunt, Zoom, and Social Media Challenge are available for your participation anytime – even after deadlines. To be eligible for prizes you must complete activities by the deadline.
Want to do a fun digital scavenger hunt?
Time: ~20 min to complete
Complete all missions by 05/24/21 11pm ET, for prize drawing.
See below for more details.
Want to learn more from CDCers who work on FASD prevention, screening and interventions?
Join us for an exclusive Zoom on 05/25/21 at 8pm ET.
Advance registration required. All who register by or on 05/25/21 3pm ET will be entered into a prize drawing.
Watch the fetal alcohol spectrum disorders (FASDs) Teen Talk.
January is National Birth Defects Prevention Month and September is FASD Awareness Month. May is the halfway point between both, so a perfect time to promote preventing FASDs, which are a birth defect.
Pick your favorite fact sheet, poster, video, or other multimedia from CDC’s FASDs materials and post it on your social media using #CDCTeenNewsletter
Submit by 05/24/21 11pm ET to be entered into a prize drawing.
Click for instructions and to submit your post.
Do you have a question for a CDCer who works on FASD prevention, screening and interventions?
Submit your question for the FASD experts who will be joining the Zoom on 05/25/21 at 8pm ET.
If your question is selected, you will get a shout out on the live Zoom and a prize.
Please do not submit questions that are answered by reading this newsletter.
Click to submit your question(s) by 05/24/21 11pm ET.
CDCM PHA Teen Newsletter Scavenger Hunt May 2021
Step 1: Download the GooseChase iOS or Android app
Step 2: Choose to play as a guest
Step 3: Enter game code – GZLG74
Step 4: Enter password – CDC
Step 5: Enter your email as your player name (this is how we will contact you if you are the prize winner)
Step 6: Go to https://www.cdc.gov/fasd/ to complete your missions
Tips for Winning:
- All answers are found on the website, see Step 6.
- Open-ended answers and photo submissions are evaluated for accuracy.
- Complete all the missions by 05/25/21 11pm ET, to be entered into a drawing for a prize.
- Make sure to make your player name is your email.
Have fun!