Teen Newsletter: July 2021 – Hepatitis
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each month will focus on a different public health topic that CDC studies. Newsletter sections: Introduction, CDC’s Work, The Public Health Approach, Special Feature, Out of the CDC Museum Collection, and Activities.
Be sure to join our live Newsletter Zoom on July 27, 2021, at 8pm ET, and check out all the activities (digital scavenger hunt—Goosechase, Zoom, social media challenge, and Ask a CDCer) at the end of each newsletter. Join in on the fun and win some prizes! Also, be on the lookout for the recently added activity, a pre-Zoom game (Kahoot) that will be emailed the day of the Zoom.
Introduction – Hepatitis

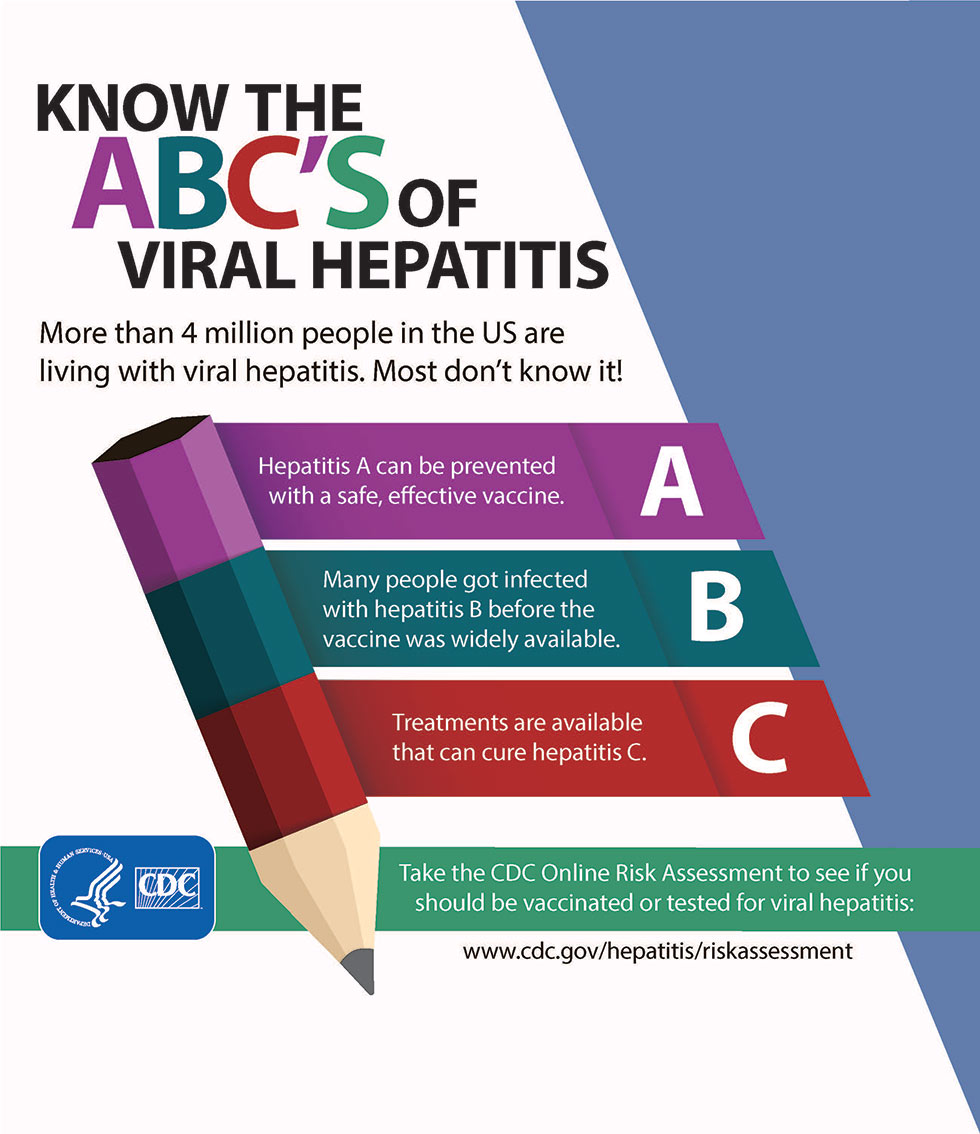
Hepatitis means inflammation of the liver. The liver is a vital organ that processes nutrients, filters the blood, and fights infections. When the liver is inflamed or damaged, its function can be affected. Heavy alcohol use, toxins, some medications, and certain medical conditions can cause hepatitis. However, hepatitis is often caused by a virus. Viral hepatitis — a group of infectious diseases known as hepatitis A, B, C, D, and E — affects millions of people worldwide, causing both acute (short-term) and chronic (long-term) liver disease. Viral hepatitis causes more than one million deaths each year. While deaths from tuberculosis and HIV have been declining, deaths from hepatitis are increasing. In the United States, the most common types of viral hepatitis are hepatitis A, hepatitis B, and hepatitis C.
United States Statistics
Hepatitis A
Hepatitis A
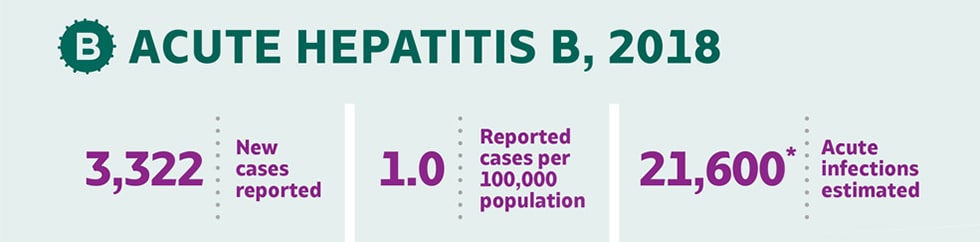
Hepatitis B
Hepatitis B
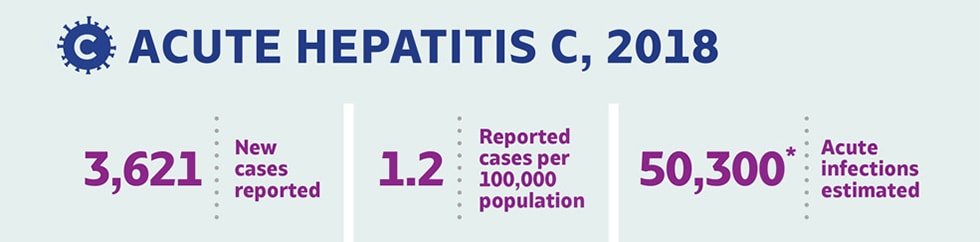
Hepatitis C
Hepatitis C
- About 12,500 new infections in 2018
- Estimated 39,900 people living with hepatitis A
- About 12,500 new infections in 2018
- Estimated 39,900 people living with hepatitis A
- About 22,600 new infections in 2018
- Estimated 862,000 people living with hepatitis B
- About 22,600 new infections in 2018
- Estimated 862,000 people living with hepatitis B
- About 50,300 new infections in 2018
- Estimated 2.4 million people living with hepatitis C
- About 50,300 new infections in 2018
- Estimated 2.4 million people living with hepatitis C
Symptoms:
Many people with hepatitis do not have symptoms and do not know they are infected. If symptoms occur with an acute infection, they can appear anytime from 2 weeks to 6 months after exposure. Symptoms of chronic viral hepatitis can take decades to develop. Symptoms of hepatitis can include: fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, light-colored stools, joint pain, and jaundice.
Hepatitis A
Hepatitis A
Hepatitis B
Hepatitis B
Hepatitis C
Hepatitis C
Can last from a few weeks to several months.
Can last from a few weeks to several months.
Can range from a mild illness, lasting a few weeks, to a serious, life-long (chronic) condition. More than 90% of unimmunized infants who get infected develop a chronic infection, but 6%–10% of older children and adults who get infected develop chronic hepatitis B.
Can range from a mild illness, lasting a few weeks, to a serious, life-long (chronic) condition. More than 90% of unimmunized infants who get infected develop a chronic infection, but 6%–10% of older children and adults who get infected develop chronic hepatitis B.
Can range from a mild illness, lasting a few weeks, to a serious, life-long (chronic) infection. Most people who get infected with the hepatitis C virus develop chronic hepatitis C.
Can range from a mild illness, lasting a few weeks, to a serious, life-long (chronic) infection. Most people who get infected with the hepatitis C virus develop chronic hepatitis C.
CDC’s Work – Hepatitis
The Division of Viral Hepatitis (DVH) is part of the National Center for HIV, Viral Hepatitis, STD, and TB Prevention at CDC. DVH consists of three branches that work collaboratively, 1) Epidemiology and Surveillance, 2) Prevention, and 3) Laboratory.
In collaboration with domestic and global partners, DVH provides the scientific and programmatic foundation and leadership for the prevention and control of hepatitis virus. DVH conducts research, surveillance, education and training, and evaluation to facilitate policy and design interventions to address the most common forms of viral hepatitis in the United States: hepatitis A virus (HAV), hepatitis B virus (HBV) and hepatitis C virus (HCV). These unrelated viruses are transmitted through different routes and require specific prevention strategies. CDC also conducts surveillance and investigation of other forms of viral hepatitis, particularly those common in other parts of the world, and serves as a WHO Collaborating Center for Reference and Research on Viral Hepatitis.
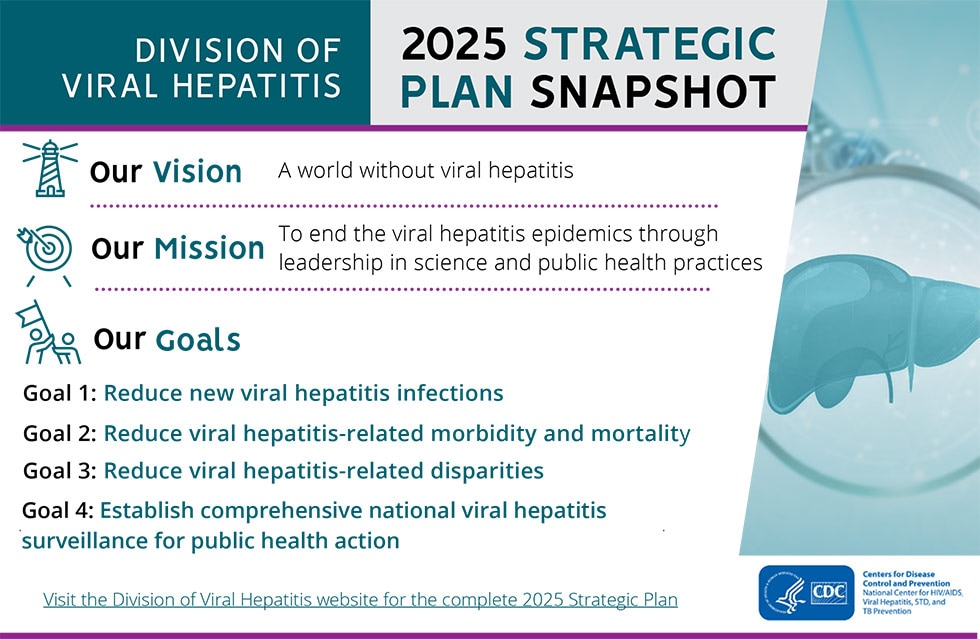
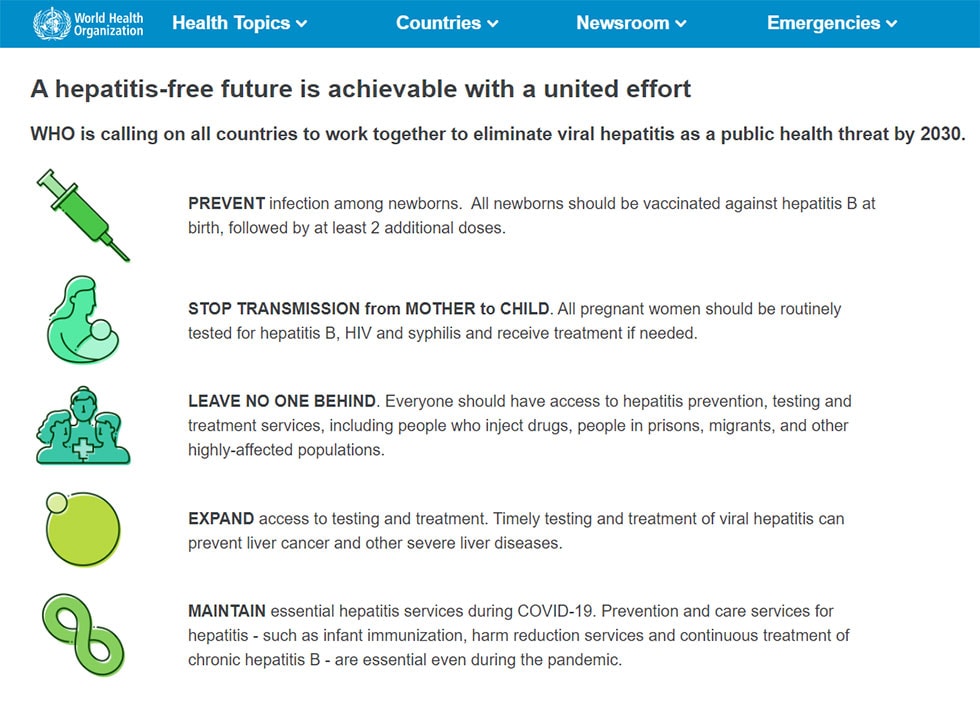
DVH’s 2025 Strategic Plan outlines goals, strategic approaches, objectives, and outcome measures for making measurable progress in reducing new viral hepatitis infections and viral hepatitis-associated illnesses, deaths, and disparities in the U.S. over the next five years. In developing 2025 outcome measures for this strategic plan, DVH was mindful of existing global goals to eliminate viral hepatitis as a public health threat by 2030.
The Public Health Approach – Hepatitis
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, as well as other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps.
1. Surveillance (What is the problem?)
Information on cases of viral hepatitis reported nationally has been maintained at CDC in two surveillance systems
- National Notifiable Disease Surveillance System (NNDSS) – includes diagnosis, event dates (e.g., illness onset), and basic demographic data (e.g., state, county, age, race, ethnicity).
- Viral Hepatitis Surveillance Program (VHSP) – includes clinical features, serologic test results, and risk factors for infection. This information is needed to confirm the diagnosis, determine a source of infection, and identify others at risk of infection that would benefit from preventive intervention.
Surveillance for viral hepatitis is needed to direct and evaluate prevention and control activities. CDC recommends that all states and territories conduct surveillance for acute viral hepatitis, including hepatitis A, B, C, and non-ABC hepatitis. In addition, states and territories should consider establishing computerized databases of persons who test positive for hepatitis B surface antigen (HBsAg) or antibody to hepatitis C virus (anti-HCV) to facilitate the notification, counseling and management of persons with chronic hepatitis B virus (HBV) or hepatitis C virus (HCV) infections.
2. Risk Factor Identification (What is the cause?)
As you learned above in the introduction, heavy alcohol use, toxins, some medications, and certain medical conditions can cause hepatitis. However, hepatitis is often caused by a virus.
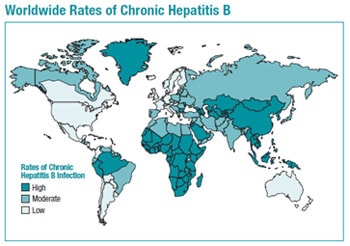
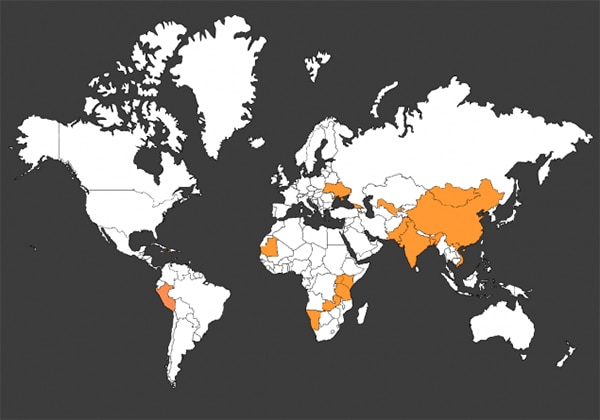
People Born Outside of the United States
Many countries in Asia, the Pacific Islands, and Africa have high or moderate prevalence of chronic hepatitis B (see map below). The overall prevalence of hepatitis B in the WHO Western Pacific Region is about 6.2%, and nearly 70% of Asian Americans were born outside of the United States. Asian Americans make up 6% of the total population in the United States, but account for 58% of the 862,000 Americans living with chronic hepatitis B.
Prevalence is also high among Pacific Islanders living in the United States. The overall prevalence of hepatitis B in the WHO African Region is 6.1%, although certain African countries are experiencing a much higher burden of infection (e.g., Somalia, Zimbabwe, Eritrea, Sudan, Nigeria, and Liberia). During the past 3 decades, migration from an African country of origin to the United States has increased from 200,000 to 1.7 million people. Of people living with chronic hepatitis B in the United States, 12% were born in Africa.
Drug Use and Viral Hepatitis
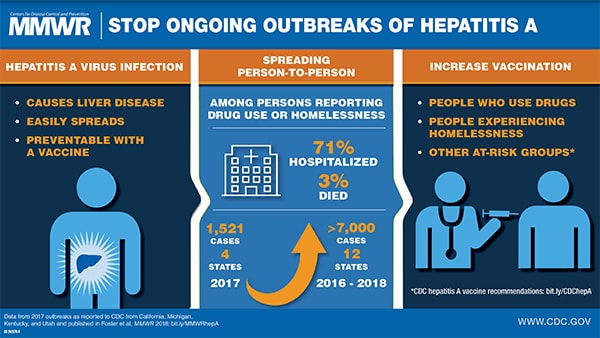
People Who Use or Inject Drugs (PWUD or PWID) and Hepatitis A
Current widespread outbreaks of hepatitis A are occurring across the country. Such outbreaks are believed to occur through both percutaneous and fecal-oral routes. Severe complications, high rates of hospitalization, and even deaths have occurred nationwide as a result of these outbreaks. While hepatitis A can affect anyone, in these outbreaks certain groups are at greater risk of being infected, including people who use or inject drugs. To help stop the outbreaks, CDC recommends the hepatitis A vaccine for PWUD and PWID.
People Who Inject Drugs and Hepatitis B and Hepatitis C
Both hepatitis B and hepatitis C are bloodborne diseases. PWID are at risk for hepatitis B virus (HBV) and hepatitis C virus (HCV) infection through the sharing of needles and any equipment used to prepare and inject drugs. In recent years, an emerging HCV epidemic has been occurring among young PWID, particularly in rural and suburban settings, underscoring the need for routine hepatitis C testing for people who continue to engage in high-risk behaviors.
Other populations with increased risk
- International travelers
- Men who have sex with men
- People with occupational risk for exposure
- People who anticipate close personal contact with an international adoptee
- People experiencing homelessness
- People with chronic liver disease, including hepatitis B and hepatitis C
- People with HIV
3. Intervention Evaluation (What works?)
Hepatitis A
There are two types of hepatitis A vaccine.
- The first type, the single-antigen hepatitis A vaccine, is given as two shots, 6 months apart, and both shots are needed for long-term protection against hepatitis A. Vaccination with the full, two-dose series of hepatitis A vaccine is the best way to prevent infection. Hepatitis A vaccine has been licensed in the U.S for use in people 1 year of age and older. Additional guidance is available in Recommendations of the ACIP.
- The other type is a combination vaccine that protects people against both hepatitis A and hepatitis B. The combination vaccine can be given to anyone 18 years of age and older and is given as three shots over 6 months. All three shots are needed for long-term protection for both hepatitis A and hepatitis B.
Immune globulin can provide short-term protection against hepatitis A, both pre- and postexposure. Immune globulin must be administered within 2 weeks after exposure for maximum protection. Additional guidance is available in MMWR: Updated Dosing Instructions for Immune Globulin (Human) GamaSTAN S/D for Hepatitis A Virus Prophylaxis. Given that the virus is transmitted through the fecal-oral route, good hand hygiene—including handwashing after using the bathroom, changing diapers, and before preparing or eating food—is integral to hepatitis A prevention.
Hepatitis B
The best way to prevent hepatitis B is by getting vaccinated. The hepatitis B vaccine is safe and effective. Completing the series of shots (2, 3, or 4 doses, depending on the manufacturer) is needed to be fully protected. Who is the vaccine recommended for?
- All infants
- All children and adolescents younger than 19 years of age who have not been vaccinated
- People at risk for infection by sexual exposure
- People at risk for infection by exposure to blood
Three single-antigen vaccines and two combination vaccines are currently licensed in the U.S. for Hepatitis B.
Single-antigen hepatitis B vaccines
- ENGERIX-B®
- RECOMBIVAX HB®
- HEPLISAV-B™
Combination vaccines
- PEDIARIX®: Combined hepatitis B, diphtheria, tetanus, acellular pertussis (DTaP), and inactivated poliovirus (IPV) vaccine. Cannot be administered before age 6 weeks or after age 7 years.
- TWINRIX®: Combined hepatitis A and hepatitis B vaccine. Recommended for people aged ≥18 years who are at increased risk for both HAV and HBV infections.
Hepatitis C
There is currently no vaccine for hepatitis C due to its higher variability than hepatitis A and B. That being said, there are still ways to prevent and treat hepatitis C.
- Universal hepatitis C screening:
- Hepatitis C screening at least once in a lifetime for all adults aged 18 years and older, except in settings where the prevalence of HCV infection (HCV RNA‑positivity) is less than 0.1%.
- Hepatitis C screening for all pregnant women during each pregnancy, except in settings where the prevalence of HCV infection (HCV RNA‑positivity) is less than 0.1%.
- One‑time hepatitis C testing regardless of age or setting prevalence among people with recognized conditions or exposures:
- People with HIV
- People who ever injected drugs and shared needles, syringes, or other drug preparation equipment, including those who injected once or a few times many years ago
- CDC recommends that people who are diagnosed with hepatitis C be provided
- medical evaluation (by either a primary-care clinician or specialist [e.g., in hepatology, gastroenterology, or infectious disease]) for chronic liver disease, including treatment and monitoring;
- hepatitis A and hepatitis B vaccination;
- screening and brief intervention for alcohol consumption; and
- HIV risk assessment and testing.
More information on recommendations for testing, management, and treating hepatitis C are available from CDC and the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America.
4. Implementation (How did we do it?)
In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”
For this last step, let’s focus on the Know Hepatitis B campaign. The Know Hepatitis B campaign seeks to increase awareness about the silent epidemic of hepatitis B and encourage people who may be chronically infected with hepatitis B to get tested so they can take care of themselves and protect their families.
Hepatitis B is common worldwide, especially in many parts of Asia and the Pacific Islands. As you learned above in step 2, Risk Factor Identification, in the U.S., hepatitis B disproportionately affects Asian Americans. While Asian Americans make up 6% of the U.S. population, they account for more than 58% of Americans living with hepatitis B. As many as 2 in 3 people living with hepatitis B do not know they are infected. Many people can live with the disease and not feel sick or have any symptoms. Testing identifies people living with hepatitis B and helps them take steps to protect their health, including starting treatment that can delay or reverse the effects of liver damage.
In 2013, the Division of Viral Hepatitis, along with its partner, Hep B United, launched Know Hepatitis B, a national communications campaign promoting hepatitis B testing among Asian Americans. This multilingual campaign has materials in English, Chinese, Korean, and Vietnamese, and messages are delivered through a variety of multi-media channels. Community-level outreach, in partnership with Hep B United and its local affiliates, also incorporated campaign messages and materials that facilitate education and communication about hepatitis B among health care providers, local partners, and patients.
As you can see, using The Public Health Approach helps public health professionals identify a problem, find out what is causing it, and determine what solutions/interventions work.
World Hepatitis Day is recognized annually on July 28th, the birthday of Dr. Baruch Blumberg (1925–2011). Dr. Blumberg discovered the hepatitis B virus in 1967, and 2 years later he developed the first hepatitis B vaccine. These achievements culminated in Dr. Blumberg winning the Nobel Prize. Organizations around the world, including WHO and CDC, commemorate World Hepatitis Day to raise awareness of the problem of viral hepatitis, which impacts more than 325 million people worldwide. It creates an opportunity to educate people about the burden of these infections, CDC’s efforts to combat viral hepatitis around the world, and actions people can take to prevent these infections.
What can you do for World Hepatitis Day?
Learn more about CDC’s global efforts and collaborations
Check out CDC’s Division of Viral Hepatitis global homepage to learn about the progress being made worldwide towards viral hepatitis prevention and control, the room for improvement in prevention and treatment, how CDC’s Division of Viral Hepatitis collaborates with others globally, and efforts towards elimination.

Listen to the World Hepatitis Day Podcast
This podcast features Dr. Robert Brown of Weill Cornell Medical Center in New York City interviewing CDC’s Dr. Carolyn Wester, as they discuss new and important guidelines developed to enhance the health of viral hepatitis patients. The podcast took place live on 7/28.

Use “World Hepatitis Day” Image
Please feel free to right-mouse-click on this image link and save to use on your own webpage or in your email signature block.

Join us on Social Media
Follow @cdchep on Twitter for information about all types of viral hepatitis. Use #WorldHepatitisDay to join the conversation and spread the word.
Choose from sample social media posts below to support World Hepatitis Day.
For #WorldHepatitisDay on 7/28, learn more about the different types of viral #hepatitis – A through E – and the impact each has across the world. https://go.usa.gov/xyd5s
For World Hepatitis Day on 7/28, learn more about the different types of viral hepatitis that impact millions worldwide and what is being done by CDC to help eliminate hepatitis globally. https://go.usa.gov/xyd5s
Out of the CDC Museum Collection – Hepatitis
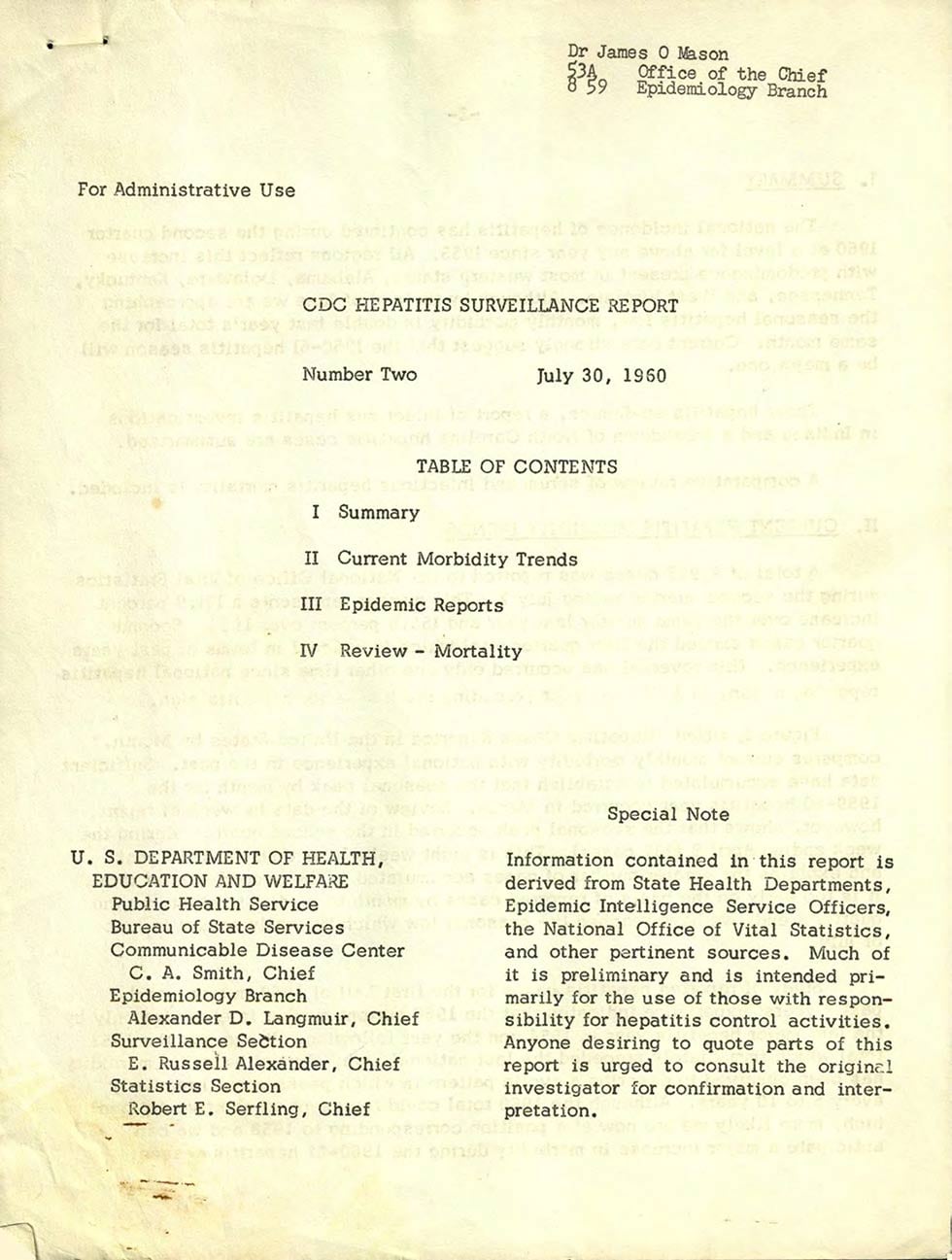
This month’s Out of the CDC Museum Collection features an archival item from July 30, 1960; the CDC Hepatitis Surveillance Report.
The history of the discovery of causative viruses is a very fascinating scientific adventure. Did you know that individualization of several types of hepatitis only emerged after World War II? National hepatitis reporting began in 1953. According to A Brief History of Hepatitis Milestones, their identification has been associated with milestones which revolutionized medicine and public health. The discovery of hepatitis B virus (HBV) brought the first ever vaccine not prepared by tissue culture, but initially directly from plasma and soon the first vaccine produced by genetic engineering. The HBV vaccine proved to be the first “anti-cancer” vaccine by preventing hepatocellular carcinoma and practically eradicating it from childhood in Taiwan. Pretty cool right? Successful vaccines have since become available for hepatitis A virus, and more recently hepatitis E virus. The discovery of hepatitis C virus in 1989 opened a new era since it was the first virus to be identified by a direct molecular approach.
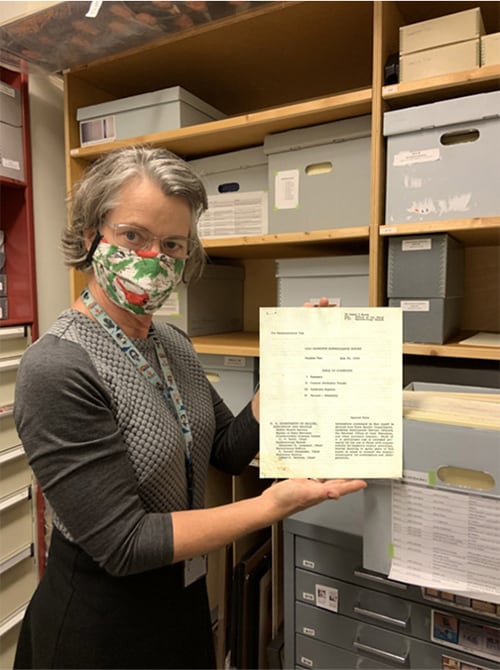
The CDC Museum Collections Manager Mary Hilpertshauser (contractor, Chickasaw Management, Inc.) shares her favorite quote from the 1960’s report –
“Samples from this well submitted to the Tennessee Department of Public Health Laboratory contained coliform organisms with remarkable consistency, indicating rather constant fecal contamination. This well, inadequately protected, was less than fifty feet from a pit privy and less than one hundred feet from a sinkhole into which drained a septic tank and a pig pen.
A four-year-old girl who was diagnosed by her physician in October as a case of infectious hepatitis frequently visited her grandmother, whose privy was, as above noted, close to the incriminated well. If this girl had been a convalescent carrier of the infectious hepatitis virus in early December or late November, she could have infected the well.”
Bonus – 75 Years of CDC!
The CDC turned 75 this month! We are kicking off a year of celebration with this bonus section, which highlights stops in CDC’s history.
In this July newsletter, our bonus will focus on important events before CDC became established in 1946. Here’s a timeline of some important events:
- In 1798, the nation’s first public health agency, the Marine Hospital Service (MHS), was formed.
- In 1902, the Marine Hospital Service changed its name to Public Health and Marine Hospital Service.
- In 1912, the Public Health and Marine Hospital Service was renamed to the United States Public Health Service (USPHS).
- In 1942, Malaria Control in War Areas (MCWA), a USPHS program, was created. MCWA was CDC’s predecessor.
- On July 1, 1946, the Communicable Disease Center (CDC) was established.

At its founding, CDC had around 400 employees, most of whom formerly worked in the MCWA. The CDC office, pictured here, was in the former MCWA headquarters, the eight-story “Volunteer Building” on the corner of Peachtree Street and 7th Street. CDC occupied two floors in this building and was present at a few other sites throughout the Atlanta area, including Chamblee and Lawrenceville.
Did you know
- CDC’s budget started with only $10 million dollars and now has a budget of around $11 billion.
- CDC started with fewer than 400 employees and now has more 14,000 employees.
- The initial primary mission of CDC was to prevent malaria from spreading across the nation.
Newsletter Activities
All July 2021 Teen Newsletter winners will be announced 07/27/21 during the Zoom – see individual deadlines below, as applicable.
Don’t forget! The CDC Museum Public Health Academy Teen Newsletter has the newsletter activity prize category: Future CDCer.
To qualify for Future CDCer, you must participate in all newsletter activities (scavenger hunt—Goosechase, Zoom, social media challenge, Ask a CDCer, and pre-Zoom game—Kahoot). All that qualify will be entered into a prize drawing for a CDC Museum Public Health Academy t-shirt.
*The following newsletter activities: Scavenger Hunt, Zoom, and Social Media Challenge are available for your participation anytime – even after deadlines. To be eligible for prizes you must complete activities by the deadline.
Want to do a fun digital scavenger hunt?
Time: ~20 min to complete
Complete all missions by 07/26/21 11pm ET, for prize drawing.
See below for more details.
Want to learn more from CDCers who work on hepatitis?
Join us for an exclusive Zoom on 07/27/21 at 8pm ET.
Advance registration required. All who register by or on 07/27/21 3pm will be entered into a prize drawing.
Watch the hepatitis Teen Talk.
Help us promote the NEW CDC Museum Instagram account!
Follow the page and like/share our content.
Submit a screenshot of you sharing one of our posts by 07/26/21 11pm ET to be entered into a prize drawing.
Do you have a question for a CDCer who works on hepatitis?
Submit your question for the hepatitis experts who will be joining the Zoom on 07/27/21 at 8pm ET.
If your question is selected, you will get a shout out on the live Zoom and a prize.
Please do not submit questions that are answered by reading this newsletter.
Click to submit your question(s) by 07/26/21 11pm ET.
CDCM PHA Teen Newsletter Scavenger Hunt
July 2021
Step 1: Download the GooseChase iOS or Android app
Step 2: Choose to play as a guest
Step 3: Enter game code – XDQ4XP
Step 4: Enter password – CDC
Step 5: Enter your email as your player name (this is how we will contact you if you are the prize winner)
Step 6: Go to https://www.cdc.gov/hepatitis/index.htm to complete your missions
Tips for Winning:
- All answers are found on the website, see Step 6.
- Open-ended answers and photo submissions are evaluated for accuracy.
- Complete all the missions by 07/26/21 11pm ET, to be entered into a drawing for a prize.
- Make sure to make your player name is your email.
Have fun!