Teen Newsletter: November 2020 – Mental Health
The David J. Sencer CDC Museum (CDCM) Public Health Academy Teen Newsletter was created to introduce teens to public health topics. Each month will focus on a different public health topic that CDC studies. Newsletter sections: Introduction, CDC’s Work, The Public Health Approach, Special Feature, Out of the CDC Museum Collection, and Activities.
Introduction – Mental Health
You voted during our October Newsletter Zoom for this month’s topic – you picked mental health! Be sure to join our live Newsletter Zoom to vote on the next public health topic, too. Check out all the activities (digital scavenger hunt—Goosechase, Zoom, social media challenge, and Ask a CDCer) at the end of each newsletter. Join in on the fun and win some prizes! Also, be on the lookout for the recently added pre-Zoom Kahoot that will be emailed out before the Zoom.

Mental Health

Mental health is an important part of overall health and well-being. Mental health includes our often used interchangeably, poor mental health and mental illness are not the same things. A person can experience poor mental health and not be diagnosed with a mental illness. Likewise, a person diagnosed with a mental illness can experience periods of physical, mental, and social well-being.
What is Mental Illness?

Mental illnesses are conditions that affect a person’s thinking, feeling, mood or behavior, such as depression, anxiety, bipolar disorder, or schizophrenia. Such conditions may be occasional or long-lasting (chronic) and affect someone’s ability to relate to others and function each day. There are more than 200 classified types of mental illness.
Why is Mental Health Important for Overall Health?

Mental and physical health are equally important components of overall health. Mental illness, especially depression, increases the risk for many types of physical health problems, particularly long-lasting conditions like stroke, type 2 diabetes, and heart disease. Similarly, the presence of chronic conditions can increase the risk for mental illness.
Can mental health change over time?

Yes, it’s important to remember that a person’s mental health can change over time, depending on many factors. When the demands placed on a person exceed their resources and coping abilities, their mental health could be impacted. For example, if someone is working long hours, caring for an ill relative, experiencing economic hardship, or living through an infectious disease outbreak/pandemic they may experience poor mental health.
The coronavirus disease 2019 (COVID-19) pandemic may be stressful for people. Fear and anxiety about a new disease and what could happen can be overwhelming and cause strong emotions in adults and children. Public health actions, such as social distancing, can make people feel isolated and lonely and can increase stress and anxiety. However, these actions are necessary to reduce the spread of COVID-19. Coping with stress in a healthy way will make you, the people you care about, and your community stronger.
How you respond to stress during the COVID-19 pandemic can depend on your background, your social support from family or friends, your financial situation, your health and emotional background, the community you live in, and many other factors.

The changes that can happen because of the COVID-19 pandemic and the ways we try to contain the spread of the virus can affect anyone, especially teens and young adults. Check out the Special Feature below to increase your ability to adapt and be resilient throughout the COVID-19 pandemic.
CDC’s Work – Mental Health
CDC is dedicated to helping all people live mentally healthier lives. We focus on preventing or reducing the impact of mental illness as a critical part of overall wellness, using the same approach that we use to prevent other health conditions such as heart disease or influenza, including early identification and intervention for those at risk, and providing science-based strategies to reduce the risk. CDC works in collaboration with federal and other partners to bridge the gap between research and delivery.
We all likely know someone who has experienced poor mental health or mental illness at some point in their lives.
Yet there are still many harmful attitudes and misunderstandings around mental health and mental illness, which make people ignore mental health, fuel stigma about mental illness, and make it harder to reach out for help. Take this quiz and see if you can separate the myths from the facts.
The Public Health Approach – Mental Health
Public health problems are diverse and can include infectious diseases, chronic diseases, emergencies, injuries, environmental health problems, as well as other health threats. Regardless of the topic, we take the same systematic, science-based approach to a public health problem by following four general steps. CDC works to prevent or reduce the impact of mental illness in the following ways:

1. Surveillance (What is the problem?)
In public health, we identify the problem by using surveillance systems to monitor health events and behaviors occurring among a population.
Mental illnesses are among the most common health conditions in the U.S.
- More than 50% will be diagnosed with a mental illness or disorder at some point in their lifetime.

1 in 5 Americans will experience a mental illness in a given year.
- 1 in 5 children, either currently or at some point during their life, have had a seriously debilitating mental illness.
- Half of all chronic mental illness begins by age 14 and three-quarters begin by age 24.
- 1 in 25 Americans lives with a serious mental illness, such as schizophrenia, bipolar disorder, or major depression.
CDC uses existing national public health surveys to assess the prevalence, severity, and economic impact of mental disorders in the U.S. and monitor trends and patterns over time.
- Behavioral Risk Factor Surveillance System (BRFSS) Questions include recent mentally unhealthy days, anxiety and depressive disorders, mental illness and stigma, and psychological distress.
- National Health and Nutrition Examination Survey (NHANES) Collects data covering a number of conditions, including depression and anxiety, symptoms of conditions, concerns associated with mental health and substance abuse, and mental health service use and need.
- National Health Interview Survey (NHIS) Questions include serious psychological distress, feelings of depression and anxiety, presence of attention deficit/hyperactivity disorder and autism spectrum disorder. The NHIS also examines mental health service use and whether individuals have unmet mental health needs.
- National Ambulatory Medical Care Survey Collects data on type of provider, medications, primary diagnoses and presence of long-lasting conditions.
- National Hospital Care Survey (NHCS) Examines care provided across treatment settings.
- National Study of Long-Term Care Providers (NSLTCP) Monitors mental illness, depression, and service use.
- National Survey of the Diagnosis and Treatment of ADHD and Tourette Syndrome (NS-DATA) Collects information about children 2 to 15 years old who had ever been diagnosed with attention-deficit/hyperactivity disorder (ADHD) and/or Tourette syndrome (TS) with the goal of better understanding diagnostic practices, level of impairment, and treatments for this group of children.
- National Violent Death Reporting System (NVDRS) Collects data from medical examiners, coroners, police, crime labs, and death certificates to understand the circumstances surrounding violent deaths, including suicide. NVDRS can also provide details on the circumstances that may have led to violent deaths, including mental illness and mental disorders.
- Pregnancy Risk Assessment Monitoring System (PRAMS) Collects data on maternal attitudes and experiences before, during, and after pregnancy; includes the prevalence of self-reported postpartum depression and anxiety symptoms.
- School Health Policies and Programs Study (SHPPS) Collects data on mental health and social service policies.
- WISQARS™ CDC’s WISQARS™ (Web-based Injury Statistics Query and Reporting System) is an interactive database system that provides customized reports of injury-related data, such as intentional self-harm including suicide.
- National Survey of Children’s Health (NSCH) Examines the health of children including those with special needs with an emphasis on well-being, collects information on the presence of a mental or behavioral problem.
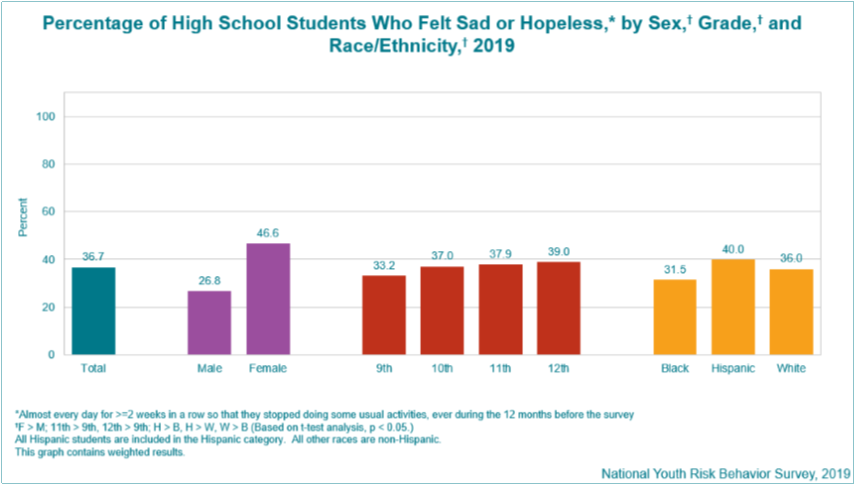
- Youth Risk Behavior Surveillance System (YRBSS) The YRBSS monitors health-risk behaviors including injuries and violence.
2. Risk Factor Identification (What is the cause?)
After we’ve identified the problem, the next question is, “What is the cause of the problem?” For example, are there factors that might make certain populations more susceptible, such as something in the environment or certain behaviors that people are practicing?
There is no single cause for mental illness. A number of factors can contribute to risk for mental illness, such as
-
- Early adverse life experiences, such as trauma or a history of abuse (for example, child abuse, sexual assault, witnessing violence)
- Experiences related to other ongoing (chronic) medical conditions, such as cancer or diabetes.
- Biological factors, such as genes or chemical imbalances in the brain
- Use of alcohol or recreational drugs
- Having few friends
- Having feelings of loneliness or isolation

3. Intervention Evaluation (What works?)
Once we’ve identified the risk factors related to the problem, we ask, “What intervention works to address the problem?” We look at what has worked in the past in addressing this same problem and if a proposed intervention makes sense with our affected population.

Tools – CDC translates research into evidence-based interventions that can be used by health care providers and communities to prevent adverse outcomes associated with mental illness.
Resources – CDC shares effective interventions and implements a coordinated approach among all groups that provide mental health services.
One group that is well known for leading public health efforts to advance the behavioral health of the nation is CDC’s sister agency, the Substance Abuse and Mental Health Services Administration (SAMHSA).
SAMHSA is within the U.S. Department of Health and Human Services, just like CDC. Its mission is to reduce the impact of substance abuse and mental illness on America’s communities.
It provides one-stop access to U.S. government information on mental health and mental health problems. It aims to educate and guide:
-
The general public
- Health and emergency preparedness professionals
- Policy makers
- Government and business leaders
- School systems
- Local communities
Content for SAMHSA is provided by:
4. Implementation (How can we do it?)
In the last step, we ask, “How can we implement the intervention? Given the resources we have and what we know about the affected population, will this work?”
CDC monitors and evaluates services and treatments of mental disorders to identify, improve, and scale what works.
As you can see, using The Public Health Approach helps public health professionals identify a problem, find out what is causing it, and determine what solutions/interventions work.
Special Feature – Mental Health
This month we are featuring a new initiative
(How Right Now) that aims to increase people’s ability to adapt and be resilient throughout the COVID-19 pandemic.
Millions of Americans are continuing to adjust to many emotional issues caused by the pandemic, such as the isolation that comes with social distancing during COVID-19—and that includes teens. Many of us may be struggling with overwhelming feelings as well as personal and family crises related to the pandemic.
To address this, How Right Now, provides information and tools to help reduce stress and manage challenging emotions. How Right Now is available in both English and Spanish.
Resources include an inspirational video showcasing individual challenges and hope during COVID-19, mental health expert videos, and celebrity PSAs.
The How Right Now website and resources can help you manage stress and anxiety, and can provide ways to cope right now. The initiative will continue to develop and post new content in the coming months, so be sure to check back for additional resources. The interactive website provides inspiration, areas to start conversation, and is a safe place to express how you truly feel.
As you have learned, mental health includes our emotional and social well-being. It affects how we think, feel, and act. It also helps determine how we handle stress, relate to others, and make healthy choices. Because the COVID-19 pandemic has produced new stresses on all of us, it’s important that we take care of our mental health in these challenging times.
How Right Now is made possible with support from the CDC Foundation.
Out of the CDC Museum Collection
Mental health is important for everyone, including professionals working a public health emergency response. Learn how CDC helped responders cope with stress and build resilience during a past epidemic.

On March 23, 2014, the WHO reported cases of Ebola Virus Disease (EVD) in the forested rural region of southeastern Guinea. The identification of these cases marked the beginning of the West Africa Ebola epidemic, the largest in history.
Take a look at the history of Ebola in West Africa (2014-2016) through the digital exhibition EBOLA: People + Public Health + Political Will. Learn how CDC, global partners, governments, organizations, and individuals came together to stop an epidemic.
Hear from Commander Jennifer Bornemann, LCSW describe her work as a behavioral health/resilience officer in the Monrovia Medical Unit (MMU). The MMU was an Ebola treatment unit in Liberia staffed by United States Public Health Service commissioned officers that treated healthcare workers during the 2014 Ebola epidemic (Fast Fact— they were the only U.S. federal entity to directly treat anyone with Ebola). “We were seen as a sense of hope, which was quite a privilege” – CDR Bornemann.
Does the name Commander Jennifer Bornemann sound familiar? It should, she was a guest speaker on our July 2020 Newsletter Zoom.
Below you can see the U.S. Flag made with Handprints of Hope.

Commander Jennifer Bornemann received this flag while at the MMU. It was made by kindergarten students from Mrs. Julie O’Malley’s kindergarten class at St. Mary’s Elementary School in Annapolis, MD. The flag was sent to encourage the officers and boost morale. It hung with great pride at the MMU and it was displayed for all visitors to see. “It was a reminder of home that we saw daily,” said one of the United States Public Health Service commissioned officers stationed at the MMU. The MMU has since been decommissioned, the flag has been returned to the U.S. and it is now part of the CDC Museum collection.
As you know, CDC is also responding to the COVID-19 pandemic. Part of the response is helping healthcare personnel and first responders cope with stress and build resilience during the pandemic.
Want to learn more about mental health and do a fun digital scavenger hunt?
Time: ~20 min to complete
See below for more details.
Want to learn more from a CDCer who works in mental health?
Watch the mental health Teen Talk.
Positive mental health refers to the presence of positive emotions and good functioning.
Post a positive mental health image, infographic or quote on your social media to promote positive metal health.
Use the hashtag #CDCTeenNewsletter and submit a screenshot of your post here.
For live Zoom only.
CDCM PHA Teen Newsletter Scavenger Hunt
November 2020
Step 1: Download the GooseChase iOS or Android app
Step 2: Choose to play as a guest
Step 3: Enter game code – 5D1GQG
Step 4: Enter password – CDC
Step 5: Enter your email as your player name
Step 6: Go to https://www.cdc.gov/mental-health/ to complete your missions
Tips for Winning:
- All answers are found on the website, see Step 6.
- Open-ended answers and photo submissions are evaluated for accuracy.
Have fun!