Injury Center Snapshot
Many types of injury and violence are urgent and interrelated. NCIPC is focused on priorities including preventing adverse childhood experiences, overdose, and suicide. When we prevent any one of these issues, we decrease the risk of the others now and for the next generation.
Exposure to ACEs can change the way the brain develops and functions, contributing to increased risk of chronic diseases, substance use, suicide, and other types of injury and violence.
MoreEach year, tens of thousands of people in the United States die as a result of an overdose. And the numbers keep increasing. Losing a loved one to overdose also has a profound impact on friends, family members, and children.
MoreThe Injury Center has been at the forefront of addressing some of today’s most pressing public health challenges such as suicide, drug overdose, and ACEs. Our work is growing and evolving, and we are preparing for future injury and violence challenges that may arise.
The Injury Center is building on ACEs research to create a solid foundation for everyone’s health and wellbeing.
- NCIPC has been a leader in ACEs prevention and mitigation efforts for decades. We have a legacy of successful initiatives that have built the framework and infrastructure for our newest investments.
- Funded 12 states or tribal nations to build jurisdiction-wide ACEs monitoring and prevention
- Tracked ACEs and health outcomes through two national level surveys
- As of 2020, all states have data on ACEs among adults
- As of 2023, for the first time, there will be national data on ACEs among adolescents
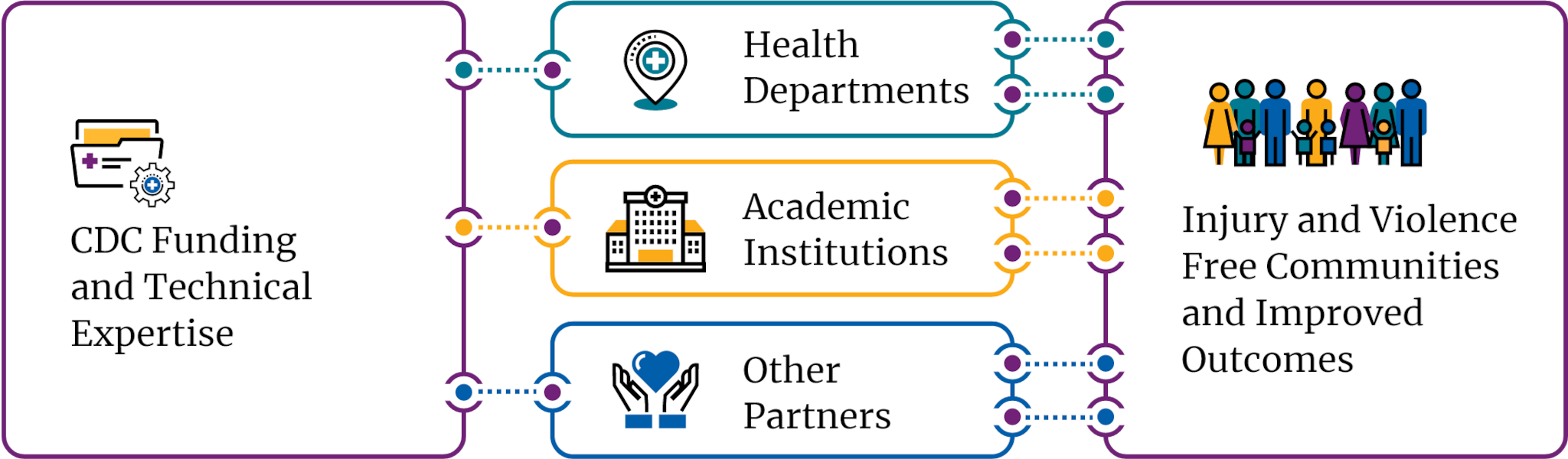
- Supported ACEs monitoring and research from more than 50 grantees in health departments and academic institutions
- Provided 23 states with funding to address the impact of COVID-19 on suicide and ACES.
- We drive data to action to create safe, stable, and nurturing environments for all children. Preventing ACEs could reduce a large number of health conditions including depression, heart disease, and obesity.9
The Injury Center applies its surveillance, research, prevention, and response approach to reduce drug overdose.
- In 2006, NCIPC scientists first published data on the growing epidemic of opioid overdose. Since then, NCIPC has been at the forefront of federal efforts to prevent overdoses and substance use–related harms.
- In 2021, we awarded $296 million to 66 jurisdictions—47 states and Washington, D.C., 16 localities, and 2 territories—to scale up overdose prevention and response efforts.
- We administer The Drug-Free Communities (DFC) Support Program — the nation’s leading effort to mobilize communities to prevent and reduce substance use among youth. More than 700 DFC coalitions are funded across the United States.
- In 2022, we released our updated Overdose Prevention Framework, which details CDC’s guiding principles and strategic priorities to address the evolving overdose crisis.
The Injury Center is dedicating new funding to address multiple forms of violence.
- In the United States, 124 people die from gun violence every day and even more sustain non-fatal injuries.8 As part of our work to address firearm safety as a public health issue, we
- awarded 18 research grants focusing on gun violence prevention and evaluating strategies that protect individuals, families, and communities
- funded 10 state health departments to provide surveillance data in near-real time on emergency visits for nonfatal firearm injuries
- released new data on firearm deaths showing a historic increase of 35% in the firearm homicide rate, the highest in more than 25 years.10
- Youth in the United States are at particular risk of violence, with homicide being the second leading cause of death for young people aged 10–24.11
- For more than 15 years, we have supported cities and local health departments working to prevent multiple forms of youth violence.
- Currently, we fund 8 recipients working to decrease high rates of violence in communities and address risk factors like limited educational or employment opportunities and racial inequity.
The Injury Center is working toward a vision of “no lives lost to suicide” by prioritizing data, science, action, and collaboration.
- People of any age, race, ethnicity, or sex can experience suicide risk, but certain groups have substantially higher rates of suicide.
- Our Comprehensive Suicide Prevention program aims to reduce suicide among higher risk groups like middle-age adults, youth and young adults, LGBTQ+ persons, veterans, and tribal communities.
- Timely data can save lives. We fund 10 states to collect near-real time data from emergency departments on suicidal thoughts and suicide attempts. These data have helped states respond to suicide clusters, track trends in suicidal behavior among adolescents, and monitor the impacts of COVID-19.
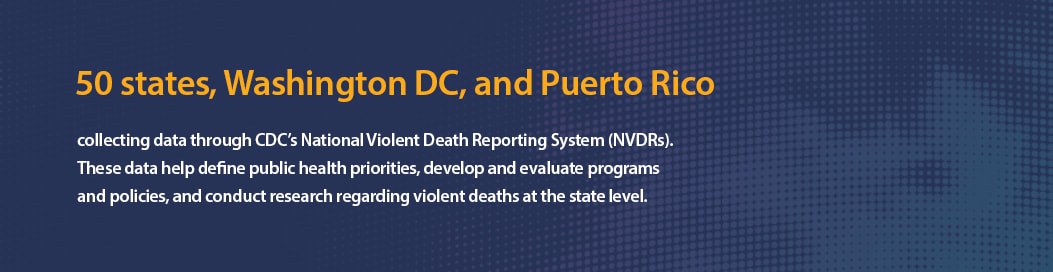
The Injury Center works with partners at other federal agencies, public health officials at the state and local level across the United States, researchers and research institutions, and communities to promote effective public health solutions to injury and violence and prevent harm in the first place. The Injury Center also provides information and tools to individuals and communities so they can support change at home.
- Swedo EA, Aslam MV, Dahlberg LL, et al. Prevalence of Adverse Childhood Experiences Among U.S. Adults — Behavioral Risk Factor Surveillance System, 2011–2020. MMWR Morb Mortal Wkly Rep 2023;72:707–715. DOI: http://dx.doi.org/10.15585/mmwr.mm7226a2
- O’Donnell J, Gladden RM, Mattson CL, Hunter CT, Davis NL. Vital Signs: Characteristics of Drug Overdose Deaths Involving Opioids and Stimulants — 24 States and the District of Columbia, January–June 2019. MMWR Morb Mortal Wkly Rep 2020;69:1189–1197. DOI: http://dx.doi.org/10.15585/mmwr.mm6935a1
- CDC WONDER: Underlying cause of death, 1999–2020. Atlanta, GA: US Department of Health and Human Services, CDC; 2022. https://wonder.cdc.gov/Deaths-by-Underlying-Cause.html
- Substance Abuse and Mental Health Services Administration. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/
- Centers for Disease Control and Prevention. Firearm deaths and rates per 100,000, United States, 2020. Web-based Injury Statistics Query and Reporting System (WISQARS), National Center for Injury Prevention and Control. [Online] Available from URL: http://www.cdc.gov/injury/wisqars/index.html.
- Centers for Disease Control and Prevention. Homicide injury deaths and rates per 100,000, United States, 2020. Web-based Injury Statistics Query and Reporting System (WISQARS), National Center for Injury Prevention and Control. [Online] Available from URL: http://www.cdc.gov/injury/wisqars/index.html.
- Guy GP Jr., Haegerich TM, Evans ME, Losby JL, Young R, Jones CM. Vital Signs: Pharmacy-Based Naloxone Dispensing — United States, 2012–2018. MMWR Morb Mortal Wkly Rep 2019;68:679–686. DOI: http://dx.doi.org/10.15585/mmwr.mm6831e1
- Centers for Disease Control and Prevention. Fatal injury data. Web-based Injury Statistics Query and Reporting System (WISQARS), National Center for Injury Prevention and Control. [Online] Available from URL: http://www.cdc.gov/injury/wisqars/index.html.
- Merrick MT, Ford DC, Ports KA, et al. Vital Signs: Estimated Proportion of Adult Health Problems Attributable toAdverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. MMWR Morb Mortal WklyRep 2019;68:999-1005. DOI: http://dx.doi.org/10.15585/mmwr.mm6844e1.
- Kegler SR, Simon TR, Zwald ML, et al. Vital Signs: Changes in Firearm Homicide and Suicide Rates — United States, 2019–2020. MMWR Morb Mortal Wkly Rep 2022;71:656–663. DOI: http://dx.doi.org/10.15585/mmwr.mm7119e1
- Centers for Disease Control and Prevention. Ten leading causes of death, United States, 2020. Web-based Injury Statistics Query and Reporting System (WISQARS), National Center for Injury Prevention and Control. [Online] Available from URL: http://www.cdc.gov/injury/wisqars/index.html.