Opioid Overdose Prevention in Tribal Communities
In 2021, on average, over 290 Americans died every day from a drug overdose. The number of overdose deaths has increased over time, with a sharp rise during the COVID-19 pandemic, including among American Indian and Alaska Native people. (Source: NVSS – Drug Overdose Deaths). In 2021, 1,358 non-Hispanic AI/AN people died by overdose, which was the highest rate of any racial or ethnic group.
The Centers for Disease Control and Prevention’s (CDC) National Center for Injury Prevention and Control (NCIPC) is committed to comprehensive efforts to address the opioid crisis in tribal and urban Indian communities. For additional details about the broader NCIPC injury prevention work in American Indian and Alaska Native communities, click here.
Overdose Deaths Involving Opioids Among American Indian and Alaskan Natives, U.S. 2010-2021
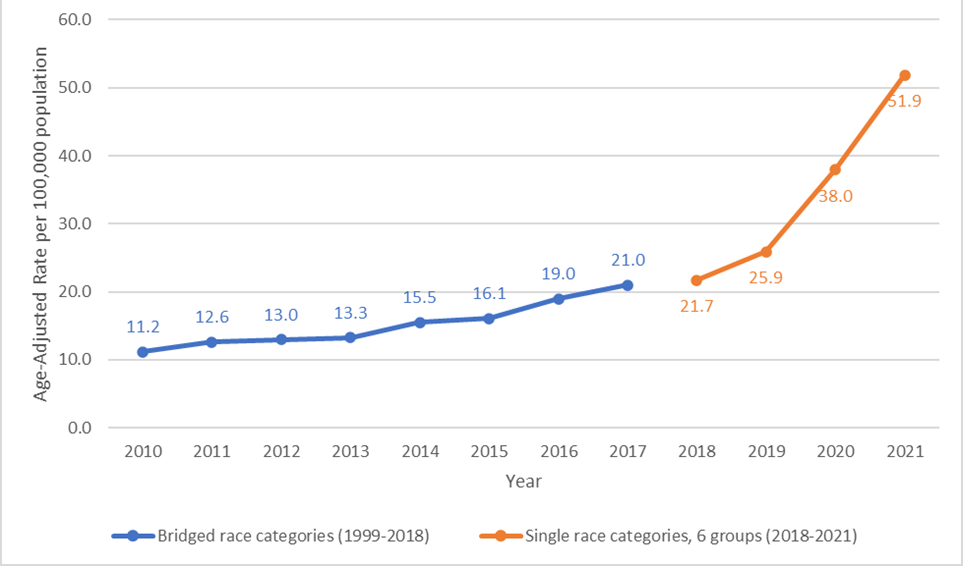
Source 2010-2017: Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 1999-2020 on CDC WONDER Online Database, released in 2021. Data are from the Multiple Cause of Death Files, 1999-2020, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/mcd-icd10.html on Jun 6, 2023
Source 2018-2021: Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 2018-2021 on CDC WONDER Online Database, released in 2023. Data are from the Multiple Cause of Death Files, 2018-2021, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/mcd-icd10-expanded.html on Jun 6, 2023
Note: Data from 2010-2017 uses the historical four Bridged-race categories (American Indian or Alaskan Native, Asian / Pacific Islander, Black or African American, White). To maintain consistency between the historical bridged race data and the single race data available beginning in 2018, age-adjusted mortality rate for 2018-2021 uses the six-category single race option.
Fiscal Year 22 Total Tribal Funding
$13,000,000
NCIPC’s funding strengthens partnerships among tribal public health and local, state, and federal entities. NCIPC-funded tribal partner projects are supported to improve opioid overdose surveillance and data infrastructure, as well as develop and implement culturally appropriate prevention strategies.
Funded Organizations
In partnership with other centers at CDC, NCIPC is providing $12 million in supplemental funds to 11 Tribal Epidemiology Centers and 15 tribes or tribal-serving organizations. These collaborations address issues of data quality, completeness, accuracy, and timeliness. Funding also supports regional strategic planning to address opioid overdose prevention so that strategies appropriate to tribal communities are developed and the strengths inherent to tribal organizations are built upon. NCIPC is also providing $1 million to national partners to provide training and technical assistance to tribes implementing overdose prevention initiatives and establish an overdose prevention track at a national conference.
Funding supports 11 Tribal Epidemiology Centers (TECs) to (1) strengthen epidemiologic surveillance and public health data infrastructure to address issues of data quality, completeness, accuracy, and timeliness, (2) support a multi-disciplinary, data-focused approach between TECs, tribal nations, and key partners to enhance data quality, and (3) implement prevention strategies that can be targeted to better address drug overdose in AIAN communities.
- Alaska Native Tribal Health Consortium (Alaska)
- Albuquerque Area Indian Health Board (New Mexico)
- California Rural Indian Health Board, Inc. (California )
- Great Lakes Inter-Tribal Council, Inc. (Wisconsin)
- Great Plains Tribal Chairmen’s Health Board (South Dakota)
- Inter-Tribal Council of Arizona, Inc. (Arizona)
- Northwest Portland Area Indian Health Board (Oregon)
- Rocky Mountain Tribal Leaders Council (Montana)
- Southern Plains Tribal Health Board Foundation (Oklahoma)
- United South and Eastern Tribes, Inc. (Tennessee)
- Urban Indian Health Institute (Alaska)
Partner tribes and tribal organizations receiving supplemental funding are working to address strategic plan priority areas: (1) epidemiologic surveillance and public health data infrastructure; (2) implementation of evidence-based health systems interventions; or (3) innovative community-based strategies.
- Alaska Native Tribal Health Consortium (Alaska)
- Bristol Bay Area Health Corporation (Alaska)
- California Rural Indian Health Board, Inc. (California)
- Cherokee Nation (Oklahoma)
- Chickasaw Nation (Oklahoma)
- Eastern Band of Cherokee Indians (North Carolina)
- Forest County Potawatomi Community (Wisconsin)
- Great Lakes Inter-Tribal Council, Inc. (Wisconsin)
- Lummi Nation (Washington)
- Northwest Portland Area Indian Health Board (Oregon)
- Rocky Mountain Tribal Leaders Council (Montana)
- Southern Plains Tribal Health Board Foundation (Oklahoma)
- United South and Eastern Tribes, Inc. (Tennessee)
- Wabanaki Health and Wellness (Maine)
- White Earth Band of Chippewa Indians (Minnesota)
NNPHI offers technical assistance and capacity building for tribes and tribal organizations for opioid overdose prevention, in collaboration with NCIPC. NNPHI works closely with Seven Directions, a member national public health institute dedicated to Indigenous health and wellness, to (1) strengthen public health systems infrastructure; (2) improve data and information systems; and (3) identify evidence-based programs and services. Involved organizations have established a tribal opioid overdose technical expert advisory group to assist with the development and implementation of a technical assistance and training plan.
CDC funds innovative community-based strategies in tribal communities that build upon the strengths of local tribal culture, tradition, and practices.
- The Northwest Portland Indian Health Board developed the 49 Days of Ceremony, an Indigenous health promotion framework that aims to connect people to Traditional Indigenous Knowledge (TIK) and cultural practices to address stigma towards individuals with a substance use disorder, reframe perceptions of health and wellbeing, and promote healing among Tribal community members.
- The Alaska Native Tribal Health Consortium is using technology to promote more informed uptake of medication assisted treatment and empower individuals with an opioid use disorder through an interactive learning experience. Individuals enter the augmented reality platform through a pair of HoloLens glasses and select learning topics ranging from the epidemiology of opioid use to brain functionality.
CDC’s Injury Center plays a critical role in addressing the drug overdose epidemic by driving progress in the five strategic priorities that guide CDC’s response framework for preventing overdoses.