Issue Brief: Status Neutral HIV Care and Service Delivery
Eliminating Stigma and Reducing Health Disparities
Updated May 16, 2024
Today, powerful HIV prevention and treatment tools can keep people healthy and help end the HIV epidemic. Combining these tools in a status neutral approach can help people maintain their best health possible, while also improving outcomes in HIV prevention, diagnosis, care, and treatment. A status neutral approach to HIV-related service delivery aims to deliver high-quality, culturally affirming health care and services at every engagement, supporting optimal health for people with and without HIV. This approach is especially important now to reduce the unacceptably high number of annual HIV infections and help close the persistent gaps along the HIV prevention and care continuum, which indicate that not enough people are being engaged or retained in HIV prevention and treatment.
- HIV testing, treatment, and prevention services are often offered separately, can be challenging to navigate,
and further emphasizes a division between people with HIV and people who could benefit from prevention. - Separating HIV services from other routine healthcare misses opportunities to engage people in HIV testing, prevention, and treatment when they seek sexual health or other non-HIV-focused services.
- Providing critical support services—like housing, food, and transportation assistance—is essential to keeping someone in ongoing care, but these services are not necessarily offered alongside what are considered “traditional” HIV care and prevention services.
- Stigma embedded in the experience of many people seeking HIV treatment and prevention services can stop people from visiting health care providers labeled as “HIV” or “STD” clinics.
- Everyone has implicit biases that affect their perceptions of others. The HIV care or prevention services someone receives may be affected by healthcare and other service providers’ implicit biases on race/ethnicity, sexual orientation, gender identity, age, and other factors. These biases, in some cases, may be why a person does not return for care and services.
Many HIV prevention experts believe a status neutral approach can help improve care and service provision and eliminate structural stigma by meeting people where they are, offering a “whole person” approach to care, and putting the needs of the person ahead of their HIV status. The status neutral approach aims to advance health equity and drive down disparities by embedding HIV prevention and care into routine care. Integrating HIV prevention and care with strategies that address social determinants of health can help reduce barriers to accessing and remaining engaged in care.
The status neutral approach also aims to increase efficiency, since the clinical and social services that prevent or treat HIV are nearly identical and can be unified in a single service plan rather than different plans based on an individual’s HIV status. Adopting a status neutral approach is one way to help deliver better prevention and care and ultimately decrease new HIV infections and support the health and quality of life of people living with HIV in the United States.
The status neutral framework provides care for the whole person by offering a “one-door” approach: people with HIV and people seeking HIV prevention services can access treatment, prevention, and other critical services in the same place. Normalizing HIV treatment and prevention helps to destigmatize both. In a status neutral approach to care, a provider continually assesses and reassesses a person’s clinical and social needs. The goal is to optimize a person’s health through continuous engagement in treatment and prevention services without creating or deepening the divide between people with HIV and people who could benefit from prevention.
A status neutral approach is unique because both of the harmonized pathways promote continual assessment of each person’s needs and ongoing engagement in HIV prevention and care, including access to support services, for anyone who could benefit from them.
Status neutral HIV service delivery is:
- Healthcare that encompasses HIV testing, treatment, and prevention services.
- HIV treatment and prevention that is offered alongside other local medical healthcare services frequently used by the community—for example, sexual health, transgender and other LGBTQ-focused care, healthcare for people who use drugs, and general primary care.
- Service delivery that recognizes and includes broader social services that support the path to optimal HIV and other health outcomes—like housing, food, transportation, employment assistance, harm reduction services, and mental health and substance use disorder services—regardless of the HIV status of the people seeking care.
- Culturally affirming, stigma-free HIV treatment and prevention, delivered by supportive and accepting providers who have been trained to recognize and address implicit racial/ethnic, sexual orientation, and other biases (thoughts and feelings that providers are not consciously aware of), and provided in settings that consider and prioritize a positive experience for the person seeking services.
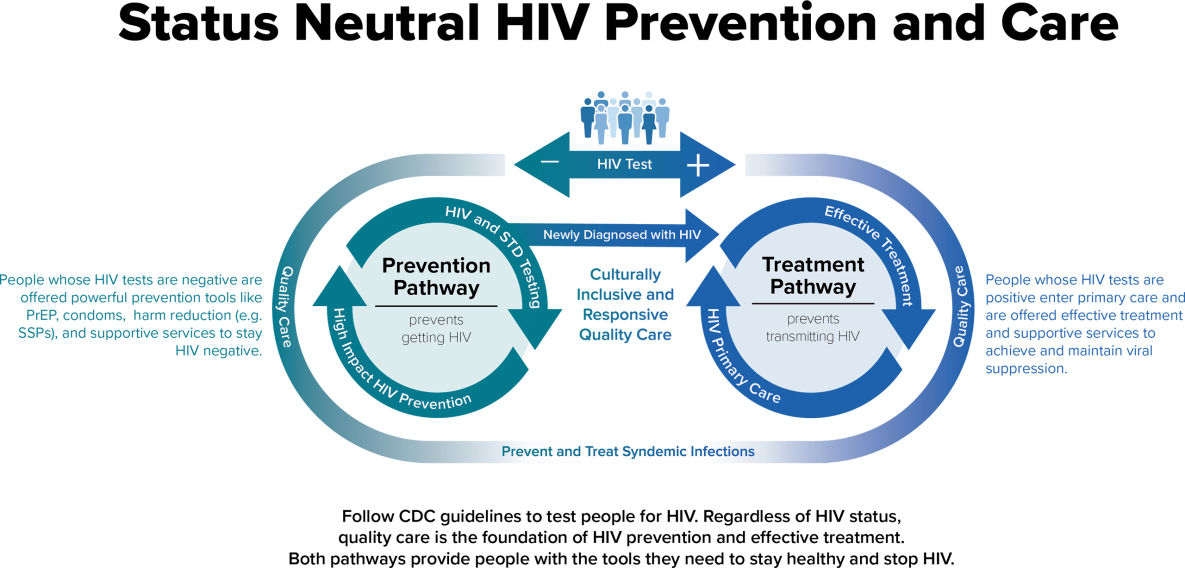
Status neutral service begins with an HIV test—the pathway to prevention and treatment. In a status neutral approach, an HIV test spurs action regardless of the result by recognizing the opportunity created by a negative or positive result for an individual to achieve better health:
- If a person receives a negative HIV test result, the provider engages the person in HIV prevention and offers powerful tools that prevent HIV, such as pre-exposure prophylaxis (PrEP). The prevention pathway emphasizes a consistent re-evaluation of the engaged person to match prevention and social support strategies to the individual’s needs. Being engaged in such preventive services also means expedited connection to HIV care in the event of a new positive HIV test result. Condoms and harm reduction services are also an important part of this prevention pathway, especially for people who are not ready or eligible for PrEP.
- If a person receives a positive HIV test result, the provider offers a prescription for effective treatment to help them become virally suppressed and maintain an undetectable viral load as well as other clinical and support services to help support general health and achieve a high quality of life. Studies have shown that people with an undetectable viral load do not transmit HIV to their sexual partners, this is often referred to as “U=U.”
HIV treatment and prevention services have not been fully used by all who need them: Only 66 percent of people with diagnosed HIV in the United States are virally suppressed. PrEP remains greatly underused—just 23 percent of the estimated one million Americans who could benefit are using the intervention. Stigma and structural barriers are major obstacles that deter people from seeking HIV prevention and care. People with HIV and people who could benefit from HIV prevention are not two distinct populations, but rather one group with similar medical and social service needs. Adopting a status neutral and “whole person” approach to people in need of prevention and care services can address these similar needs, along with HIV-related stigma.
Health departments implementing models of status neutral HIV care have reported benefits such as:
- Decreasing new HIV infections. A status neutral approach to care and service delivery means that regardless of HIV status, people have access and support to stay on highly effective public and personal health interventions like PrEP and HIV treatment. When people are supported to fully use these interventions, the outcome is the same—HIV infections and other infections are identified, prevented, and treated. For example, New York City’s status neutral approach to HIV prevention and care, first introduced in 2016, contributed to annual declines in new HIV diagnoses thereafter. New York City saw a 22% decrease in new HIV diagnoses from 2016 to 2019.
- Supporting and enabling optimal health through continual engagement in comprehensive, “whole person” care. By offering HIV services alongside other local health care and social support services used by the community, HIV prevention and treatment can become part of the fabric of holistic care designed to meet the needs of each person. As their needs evolve, a person can be seamlessly connected to new services. Potential outcomes include improved HIV care, as well as better overall health and social stability for every individual. For example, Chicago has created comprehensive status neutral health homes that offer the same services to people with HIV and people who could benefit from prevention services. Services include primary care, medications, care coordination, and behavioral health.
- Opportunities for more efficient service delivery. Parallel services and structures historically created for people with HIV or people who could benefit from prevention services can impede the most efficient use of resources. This can also inadvertently hinder connection to care by maintaining stigmatizing structures in health care. Identifying opportunities to resolve these divisions allows for more streamlined and integrated care. Washington, D.C. has seen increased capacity and improved outcomes and engagement at organizations using a status neutral approach. Using this approach has increased viral suppression rates 3% across all funded jurisdictions and increased linkage to preventive services like PrEP and harm reduction for people who tested negative for HIV.
- Improving health equity. The status neutral framework integrates HIV and prevention services to better address social determinants of health regardless of HIV status. The framework also encourages the delivery of culturally affirming care by ensuring providers recognize and address their implicit biases on issues like race, ethnicity, sexual orientation, or gender identity. These biases sometimes prevent people from returning for care and other services. Likewise, countering stigma is essential to ensure that people with HIV are not defined by their status, and that people seeking HIV prevention and care services are empowered to access these tools without facing judgment or being reduced to the result of a lab test. Addressing racial bias and stigma results in better care experiences for patients and increases the likelihood that they remain in care and stay healthy.
Here’s how some jurisdictions across the country are integrating a status neutral approach into their HIV care services:
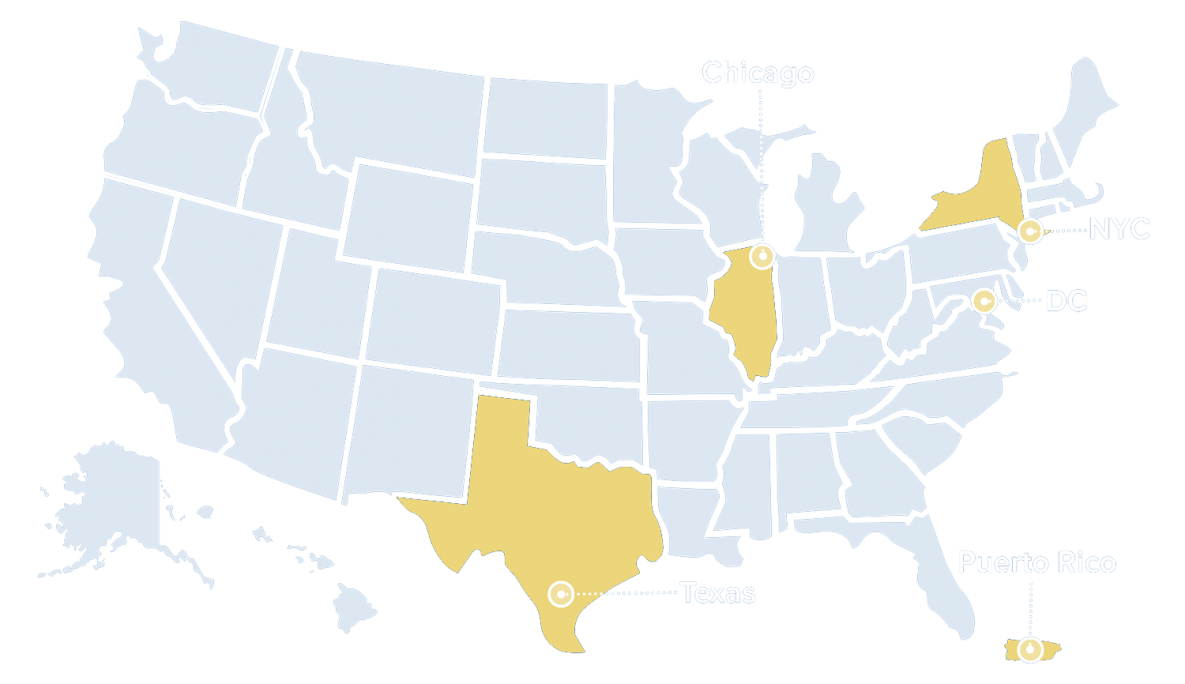
- Chicago: Integrating all HIV and sexually transmitted infection (STI) services. The Chicago Department of Public Health recently restructured its entire HIV services portfolio to adopt a status neutral approach. Based on feedback from its community members over a two-year community engagement process, the portfolio now integrates HIV and STI funding to deliver comprehensive care that links people to healthcare services like STI screening, substance use disorder treatment, mental health, housing, financial assistance, and psychosocial support in addition to HIV treatment and prevention. Anyone can access these services regardless of HIV status.
- New York City: Expanding sexual health and rebranding to reduce stigma. Stigma associated with HIV and STIs can prevent people from seeking care in STI clinics. To address this, the New York City Department of Health and Mental Hygiene rebranded its STI clinics as sexual health clinics and transformed services so that they fully meet clients’ sexual health needs. These changes have resulted in more diverse populations visiting the clinic for care.
- Puerto Rico: Delivering affirming, trauma-informed care for transgender people. Centro Ararat in Ponce, Puerto Rico delivers integrated, tailored sexual health and primary care to the transgender community. The center’s innovative clinic provides comprehensive, trauma-informed health services for transgender people alongside HIV and STI care. These services include hormone therapy and level testing, mental health services, support with name changes, and assistance finding trans-sensitive housing.
- Texas: Improving access to social services for all people. Achieving Together is the community plan to end the HIV epidemic in Texas. It lays out a vision for status neutral HIV care that supports all people in accessing services that meet their priority needs. This approach addresses social determinants of health, including housing, transportation, and food assistance, helps with insurance navigation, and increases access to mental health and substance use disorder treatment.
- Washington, D.C.: Eliminating HIV prevention and treatment barriers early. DC Health developed a status neutral approach through its regional early intervention services initiative, which supports engaging people early in HIV care and prevention services throughout the DC metropolitan area. The initiative has made strides in integrating prevention and treatment services, which previously operated independently, and consists of five pillars to promote equity and whole person health spanning HIV outreach, education, testing, and linkage to and retention in care.
CDC is providing funding, conducting implementation science to improve programs, and partnering with organizations across the U.S. to support integrated, status neutral approaches to HIV care:
- Encouraging grantees to deliver integrated services. Several of CDC’s major funding programs provide flexible resources for health department and community-based organization (CBO) partners to deliver integrated HIV prevention services. Additionally, CDC encourages health departments that receive funding through CDC’s flagship prevention and surveillance program to use these resources to support programs that adopt status neutral approaches to HIV prevention and treatment.
- Ending the HIV Epidemic initiative implementation: In July 2021, CDC awarded the second major round of EHE funding — approximately $117 million — to health departments representing 57 prioritized jurisdictions to scale up focused, local efforts designed to address the unique barriers to HIV prevention in each community. CDC encourages grantees to coordinate with STD and viral hepatitis programs, LGBTQ health centers, criminal justice and correctional facilities, and other providers to deliver HIV services. In addition, the new program provides funding to a subset of jurisdictions to strengthen HIV testing, prevention, and treatment services at dedicated STD clinics.
- High-impact HIV prevention through CBOs and health departments: CDC funded more than 90 CBOs to develop high-impact HIV prevention programs and partnerships, beginning in 2021. These CBOs are required to create HIV programs with the greatest potential to address social and structural determinants of health. CBOs can use CDC funding to help clients navigate essential support services. The program will also support integrated screening for STIs, viral hepatitis, and TB, and referrals for subsequent treatment.
- Conducting implementation science. CDC is conducting a pilot program to evaluate a project designed to deliver status neutral HIV services to transgender people. The pilot will support transgender healthcare providers and CBOs in integrating HIV, STI, viral hepatitis, and harm reduction services alongside transgender-specific healthcare. The pilot aims to establish best practices for creating a “one-door” approach for testing and other interventions that can improve the health of transgender people.
- Building partnerships. CDC is working with other federal agencies and organizations focused on issues that intersect with HIV and affect health outcomes, like sexual health, mental health, housing, incarceration, employment, and substance use disorder to advance status neutral approaches to HIV prevention and care. For example, the HIV National Strategic Plan incorporates the statusneutral framework, creating opportunities to improve systems so they support the provision of status neutral services in the national HIV response. These partnerships will enable the sharing of knowledge and best practices that translates to better implementation science, programs, and services. These partnerships can also support better integration of programmatic efforts in communities.
It will take time for a status neutral approach to be adopted across the country. Federal agencies, state and local health departments, healthcare providers, and CBOs can take steps now to begin promoting and integrating this approach into their programs and service delivery models if appropriate for their organization or jurisdiction and supported by their community:
- Federal health agencies can provide training, support, and technical assistance to state and local health departments, healthcare providers, and CBOs looking to implement status neutral HIV care. They should prioritize strategies that support front-line providers in more easily creating and implementing status neutral programs. They should also promote cross-agency collaboration to integrate HIV treatment and prevention services over time with other primary care, behavioral health, and social services.
- State and local health departments can review their current funding and care delivery models to further integrate HIV into STI and primary care settings, especially community health centers, sexual health clinics, and health access points for people who use drugs. They should also identify ways to braid funding from multiple sources, and work with CBOs and other providers to gather and share best practices and lessons learned in implementing status neutral HIV care.
- Healthcare providers and CBOs can offer dynamic, supportive care that integrates culturally affirming messages and prioritizes each patients’ individual needs. They can consider providing non-HIV services that can improve patients’ overall health, such as STI and viral hepatitis screening, mental health care, and substance use counselling, as well as linkage to social services. They can also participate in regular trainings on recognizing and addressing implicit racial/ethnic and other biases.
- Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2019. HIV Surveillance Supplemental Report 2021;26(No. 2). https://www.cdc.gov/hiv-data/archive. Published May 2021. Accessed June 2, 2021.
- Walcott M, Kempf MC, Merlin JS, Turan JM. Structural community factors and sub-optimal engagement in HIV care among low-income women in the Deep South of the USA. Cult Health Sex. 2016;18(6):682-94.
- Eaton LA, Driffin DD, Kegler C, et al. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health. 2015;105(2):e75-e82.