Pediatricians’ Personal Approach with Parents Increases COVID-19 Vaccinations at Worcester, MA Clinic

Image from the role-playing video for pediatric clinicians.
The Kaiser Family Foundation’s July 26, 2022 COVID-19 Vaccine Monitor reported that, “Vaccine uptake among children ages 5-11 slowed with four [out of] ten parents saying their child in that age group has gotten the vaccine. Nearly three [out of] ten parents of 12- to 17-year-olds and nearly four [out of] ten parents of 5- to 11-year-olds say they definitely will not get their child vaccinated for COVID-19.”
Seeing this COVID-19 vaccine hesitance and resistance among parents locally in Worcester, MA, the Prevention Research Center (PRC) at the University of Massachusetts (UMass) Chan Medical School, part of the Centers for Disease Control and Prevention’s Vaccine Confidence Network, developed a program focused on improving local pediatricians’ communication with parents. The program—CONFIDENCE: Clinicians for Effective COVID-19 Vaccine Conversations for Youth and Adolescents—was created to help clinicians have more effective conversations with parents about getting their children vaccinated for COVID-19. The program was rolled out with one clinic in spring 2022 to assess the feasibility of the program’s approach and determine whether to scale it up. After a couple months, preliminary research findings were positive—most notably, there was an 18% increase in vaccinations at children’s visits, based on data from parent exit surveys.*
*Preliminary Program Findings:
Pre/Post parent survey data (n=69)
- Provider discussion of COVID-19 increased – 87% to 98%
- Provider-shared personal vaccine experience increased – 60% to 72%
- Satisfaction with vaccine conversation increased – 73% to 84%
- Decision to vaccinate child at visit increased – 44% to 62%
What made the CONFIDENCE program so successful?
- The PRC listened to local Parents and Pediatricians’ concerns and needs by conducting pre- and post-program focus groups, interviews, and surveys. From the pre-program research findings, the PRC determined that:
- Pediatricians needed more guidance on how to have effective conversations with parents who were vaccine hesitant and resistant, and
- Parents wanted to talk with their children’s pediatrician about COVID-19 vaccination and to know if the pediatrician vaccinated their own children.
- To help pediatric providers with their conversations with parents, the PRC developed a webinar training and two role-playing videos that providers could access at their convenience.
- To help parents, they created tailored in-clinic COVID-19 vaccine fact sheets and posters that featured testimonials from the clinic’s doctors and nurses explaining why they vaccinated themselves, children, and family members.
Communication Training Webinar & Role-playing Videos
The hour-long communication for COVID-19 vaccination training webinar and role-playing videos provided pediatric clinicians with evidence-based strategies, such as those effectively used for human papillomavirus (HPV) vaccine conversations. The communication approach leads with a strong provider recommendation and integrates principles of motivational interviewing, empathy, and respect. Pediatricians were also given a CONFIDENCE one-pager for quick reference before or during patient visits.
CONFIDENCE Communication Approach:
- Strong recommendation
- Share personal story
- Assess hesitancy
- Empathize with hesitant parents – OR – Explore reasons for parents’ resistance
- Honor parents’ autonomy and discuss vaccination at every visit
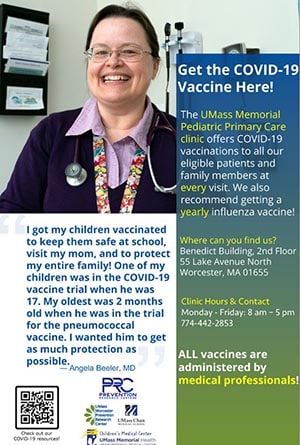
One of the posters displayed at the pediatric clinic.
The two short role-playing videos portrayed scenarios of pediatric clinicians talking with vaccine hesitant or resistant parents. The videos followed the CONFIDENCE communication approach presented in the webinar.
The PRC’s Grace Ryan, PhD, MPH, a Postdoctoral Fellow, stated, “There is a tendency to lump people into a single group of hesitancy, but there are nuances between parents who are hesitant versus resistant. Parents’ motivations for vaccinating or not vaccinating their children for COVID-19 seem to be more emotional than other vaccines and fueled by misinformation. Motivational interviewing brings empathy into the conversation and encourages clinicians to dig in to understand parents’ motivations and what’s preventing them from getting their children vaccinated.”
Posters with Vaccine Testimonials from the Clinicians
The PRC’s research showed that parents have deep trust in and respect for their children’s pediatricians, and they often want to know if and why their pediatrician got their own children vaccinated. In response, the PRC collected brief testimonials from pediatric clinicians and included them on posters with their photo and displayed them in the clinic.
A nurse who was featured in one of the clinic’s posters shared, “A patient’s parent told me that she made the decision to vaccinate her child because she saw me on the poster and that was something huge for her to see.”
The posters also included a QR code to access UMass Memorial Health’s COVID-19 resources and information on where and when to get vaccinated.
Tailored Educational Brochures for Parents
The PRC responded to local parents’ frequently asked questions collected from the pre-program research in an educational brochure given to parents during their child’s visit. The brochure was made available in nine languages predominantly spoken by community members.
COVID-19 Vaccination Strategies Applied by the PRC at UMass Chan Medical School:
With such strong preliminary findings, especially the positive feedback from the participating clinicians, the PRC has secured funding to implement the program more broadly to community-based partners across Central and Western, MA.
Dr. Ryan noted a few key takeaways from this effort:
- Draw from successful existing programs. “There are so many existing public health strategies that are effective. We recognized this and drew from what works for the pediatric population, and repurposed those strategies for this program, which saved us a lot of time.”
- Listen to and incorporate community voices. “This is true for all our work and what we’ve heard from community members and providers.”
- Research your population of focus. “Take the time to do formative and qualitative work to understand barriers among your population of interest and respond to those.”
This is an approach that requires a small amount of healthcare providers’ time yet yields productive results. The PRC team is hopeful that this approach could be effective for conversations about other vaccines, and plan to explore this more fully in the future.