Alaska Public Health Professionals Join Forces to get COVID-19 Vaccine to Communities
In Alaska, where isolation is already a big part of life, the COVID-19 pandemic has presented more barriers to getting vaccinated against the disease than in other areas of the United States. Public health officials in Alaska have worked to break down vaccination barriers through public education and changes in scheduling strategy since August 2020.
Public health officials from the Alaska Department of Health and Social Services (AKDHSS) began vaccination planning in August 2020. Much of their planning had to address challenges of weather and the long distances between many communities. They did not want to leave anyone out or any part of the state.
“The target audience throughout this process was all Alaskans,” said Tessa Walker-Linderman, the Alaska Vaccine Task Force co-lead. “We wanted to reach everyone. But in terms of our Alaska Native partners, many live in more remote communities and villages, so we wanted to ensure that we were also getting vaccine out to those remote areas.”
Bringing vaccine to the people

Kenneth Frank shares a message in Neets’aii Gwich’in as part of the AKPIRG/NPACF Language Panel project.
Alaska Immunization Program Manager Matthew Bobo said a lot of the work at AKDHSS was to strengthen the state vaccine distribution systems, especially in rural areas. They also worked to educate the public about how and where vaccinations are available across the state.
This is paying off so far, as 48% of residents were fully vaccinated as of early June 2021.
According to Regina McConkey, the communications and education co-lead for the Alaska Vaccine Task Force, the first steps the team took was making sure scheduling and informational websites were user friendly and very quickly creating a call center. They also held forums in different communities around the state to share information and answer questions about COVID-19 vaccines and how to get vaccinated.
Kelsey Pistotnik, an AKDHSS public health advisor, said the agency has been working with partners and providers to bring the vaccines to people and make getting them as easy as possible.
Originally, vaccination appointments throughout the state were made online. But when online appointment scheduling started to slow down, they switched to walk-in appointments. They also extended appointments until 10 p.m. to make vaccination more accessible to restaurant workers and others who work late.
Planning for rural vaccination
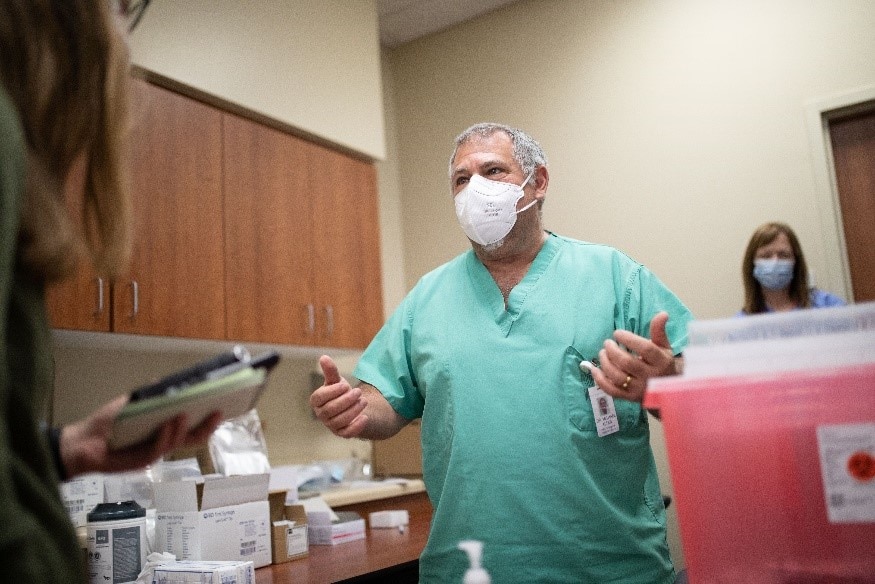
Dr. Michael Alter at Mat-Su Regional Hospital Palmer, Alaska administering the vaccine to hospital workers.
Rural vaccination was a planning priority for AKDHSS. While they were able to build on existing vaccination distribution infrastructure and relationships to reach rural communities, they had to build new systems for storing and transporting vaccine to address the unique storage and handling needs of the COVID-19 vaccines.
One of the biggest issues to overcome was distributing the correct number of vaccines to rural areas that range widely in size. The initial minimum order size for COVID-19 vaccines was 975 doses (1,170 doses as of the beginning of June), so AKDHSS had to create depots where vaccines could be stored and then redistributed in smaller quantities to rural areas.
Partners such as the Alaska Sea Life Center in Seward and CDC Arctic Investigations Program in Anchorage made redistribution possible. Along with the state public health laboratory, their partners allowed AKDHSS to use their ultra-cold freezers to help store vaccine when they distributed doses to rural areas.
“We really felt like we needed to be partnered together to be really efficient in our distribution of vaccine, so that’s how the taskforce came together. For every lead position, there’s two people: one from the state and one from ANTHC,” she said.
The team also reached out to tribal health partners in the Alaska Native Tribal Health Consortium (ANTHC) and asked them to co-lead this effort. Walker-Linderman said tribal health is a huge part of Alaska’s healthcare system, and the AKDHSS immunization program works closely with ANTHC for routine vaccinations as well.
Helping people come together again

Dr. Anne Zink, Chief Medical Officer for the State of Alaska administering the first vaccination shot to Dr. Kim Jensen, an ER physician.
For routine immunizations, tribal health organizations distribute vaccines to their villages. AKDHSS wanted to continue using that model with COVID-19 vaccines to make sure that vaccines got out to rural communities.
Bobo said many Alaska Natives “still have historic trauma” from the 1918 influenza pandemic.
“It decimated small villages, and lots of Alaska Natives died,” he said. As a result, “I was very much on high alert from the perspective of wanting to protect those villages and make sure that those communities are safe. We wanted to make sure that they’re rolling out that vaccine into these villages and communities, so they felt protected.”
The team says vaccination helped Alaskans fight isolation in communities like northern rural Alaskan villages, allowing community activities like high school sports to return.
“Especially in rural Alaska, just those kinds of stories, like being able to get back to the things that we love to do, are the kinds of things I really hold on to. It shows exactly what’s happening,” Pistotnik said. “People were able to come together again, and I think that is so meaningful in these different areas.”
What are you, your health department, or your organization doing to support COVID-19 vaccination in your community? Share your story with communityfeatures@cdc.gov and you could see it on our COVID-19 Vaccine Community Features page.