Improving HIV and TB Service Delivery
As a key implementer of the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), CDC works with the Tanzanian government to build a sustainable, high-impact national HIV response to accelerate progress towards ending the HIV epidemic. CDC collaborates with the Ministry of Health in mainland Tanzania and Zanzibar to support HIV testing, prevention, and treatment services and to strengthen health systems. CDC supports more than 1400 health facilities in Tanzania, which is nearly half of all PEPFAR-supported facilities. These facilities provide comprehensive HIV/TB services. Current programmatic priorities include:
- Scaling up targeted testing strategies, such as index testing, and social network testing;
- Providing optimal treatment regimens for children and adults to expedite reaching and sustaining viral suppression;
- Limiting treatment interruption among people enrolled in antiretroviral therapy (ART);
- Reaching all people living with HIV (PLHIV) with TB preventive therapy (TPT);
- Eliminating mother-to-child transmission of HIV;
- Strengthening health information systems;
- Using data to inform decision-making;
- Ensuring health worker training, retention, and participation in outbreak response.

During the COVID-19 pandemic, CDC’s PEPFAR program had to quickly adapt to the challenging health landscape. CDC Tanzania prioritized efforts to continue routine HIV testing services for sexual children of PLHIV with HIV, and community activities that focus on identifying people at high-risk for new HIV diagnoses. Facility and community health workers were trained on infection prevention and control practices and scaled up remote approaches to monitoring and evaluation that reduce the spread of COVID-19 among this crucial population. CDC staff and partners worked to ensure the safety and well-being of PLHIV by training health workers on standard procedures to triage patients with possible COVID-19 at healthcare facilities and set up handwashing stations at the entry points to all facilities. Access to innovative models of care and treatment services for PLHIV, including community-based medication refills, were scaled up to reduce the time they spend in healthcare facilities. Through these innovative strategies, CDC’s HIV/TB programs continued to thrive and show impressive gains in its HIV and TB programs throughout the COVID-19 pandemic.


Maximizing HIV Testing Strategies
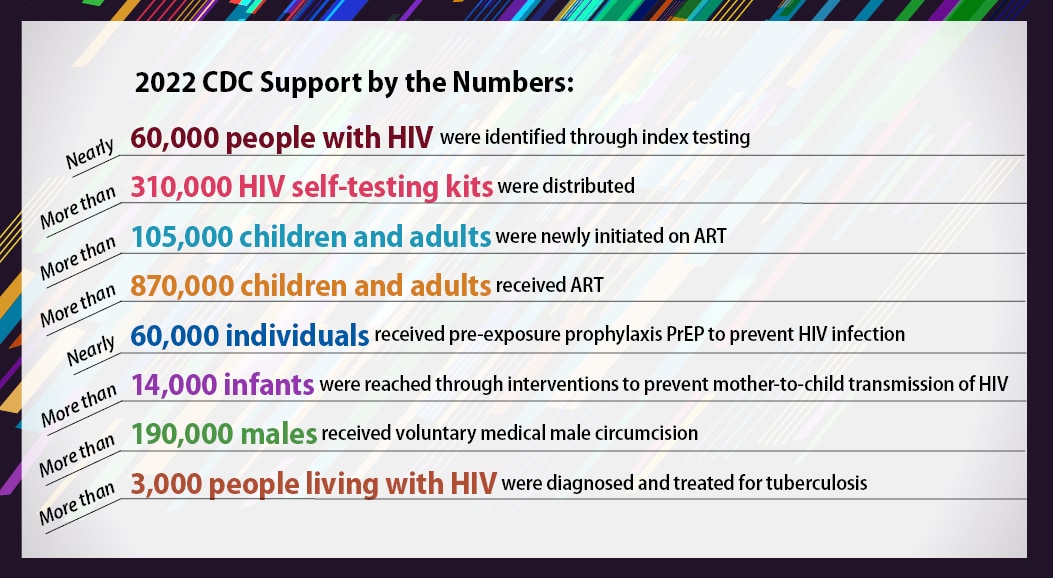
Index testing is an HIV case finding strategy that offers HIV testing to all sexual contacts of PLHIV. CDC actively monitors index testing across the cascade of service provision to ensuring the safe and ethical implementation of the strategy. Tanzania accelerated index testing in 2018 and saw an improvement in the proportion of PLHIV newly identified from 37% to 60% in FY22. CDC actively monitors index testing across the cascade of service provision to ensure the safe and ethical implementation of the strategy. In 2021, CDC began supporting social network strategies (SNS) which are peer-driven approaches to identify new HIV cases. SNS leverages an individual’s high-risk social network connections to refer them for HIV testing. HIV self testing implementation in Tanzania began in 2018. More than a year later, HIV self testing were made a legal part of routine services after the national assembly amended the law. CDC supports the Ministry of Health and regional authorities on the implementation of HIV self testing with over 500,000 kits distributed to clients through community and facility platforms to date. HIV self testing is integrated with other testing strategies to optimize the program ability to identify new HIV cases.
Scaling up Tuberculosis (TB) Prevention and Treatment
PLHIV are approximately 20 times more likely to develop TB than those without HIV. CDC supports HIV testing among TB patients, TB case finding and provision of TPT among PLHIV, and ART provision for HIV-positive TB patients. CDC supports successful models for integrating TB and HIV services, including prevention services. The proportion of PLHIV on ART who have completed or are currently on TPT is 90% as of September 2022.
Expanding Laboratory Accreditation and Certification
CDC supports Tanzania’s laboratory systems to strengthen detection capacities for HIV/TB, and other diseases of public health importance. Currently, 51 laboratories are accredited to international standards, and 131 laboratories are enrolled in CDC’s Strengthening Laboratory Management Towards Accreditation program. As of September 2022, more than 1,500 HIV testing sites were certified in the HIV rapid testing continuous quality improvement initiative, and more than 24,000 non-laboratory testers were trained of which, more than 10,000 were certified. Achieving viral suppression of HIV means that a person living with HIV has such low levels of HIV in their bodies that the chances are low that they will transmit HIV to others, which is a critical component to reaching epidemic control. By September 2022, 1,370,351 children and adults on ART had medical and/or laboratory records with documented viral load test results. Of these, 1,338,193 (98%) were virally suppressed (<1,000 copies/mL). Cumulatively, these results represent a crude estimate of viral load coverage of 92% and viral suppression of 98%.
Reaching Key and Vulnerable Populations
PLHIV are approximately 20 times more likely to develop TB than those without HIV. CDC supports HIV testing among TB patients, TB case finding and provision of TPT among PLHIV, and ART provision for HIV-positive TB patients. CDC supports successful models for integrating TB and HIV services, including prevention services. The proportion of PLHIV on ART who have completed or are currently on TPT is 90% as of September 2022.