Action in Health Care to Fight Antimicrobial Resistance
CDC invests in healthcare systems and infrastructure to make them safe places for patients to receive care. The most deadly, resistant healthcare-associated infections (HAIs) can spread from patient to patient and across healthcare facilities through patient transfer. When not stopped, these resistant healthcare-associated germs can spill over into communities, becoming much harder to control.
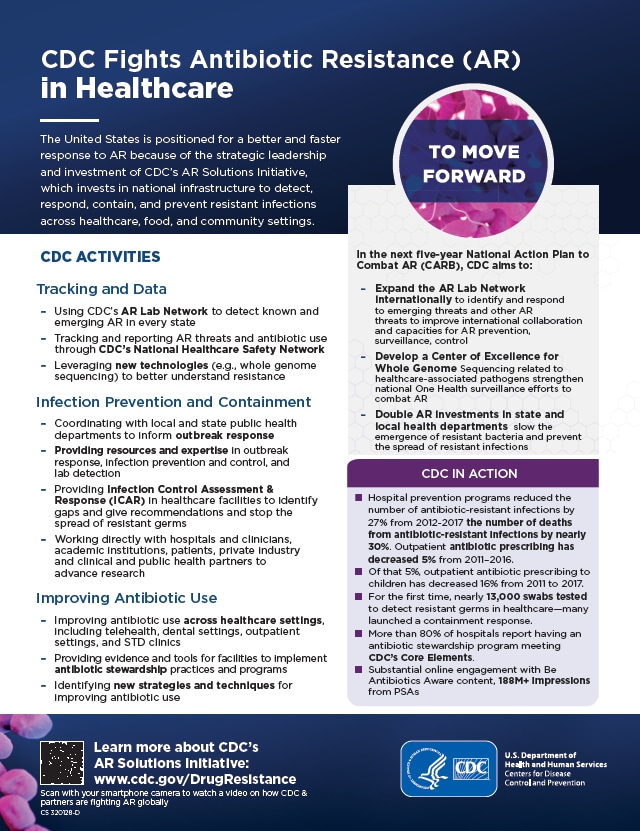
CDC expertise and resources have helped implement healthcare programs to prevent infections, including antimicrobial-resistant infections, and control the spread of germs. Hospital prevention programs have already seen successes. For example, CDC’s Containment Strategy—a series of aggressive detection and response activities—works to stop new or rare forms of antimicrobial resistance from spreading. For the “nightmare bacteria” CRE alone, aggressive containment responses could prevent 1,600 cases in just one state over three years.
Hospital prevention programs have already seen successes. From 2012 to 2017, the number of antimicrobial-resistant infections seen in hospitals dropped 27% and the number of deaths from antimicrobial-resistant infections fell nearly 30%. Nonetheless, without continued action and vigilance these gains will only be temporary. Learn more about how resistance can spread in healthcare facilities.
CDC implements activities outlined in the U.S. National Action Plan for Combating Antibiotic-Resistant Bacteria, released in 2015 and 2020. These activities are funded through CDC antimicrobial resistance investments, collectively known as CDC’s Antimicrobial Resistance (AR) Solutions Initiative. Through these investments, CDC is transforming how the nation combats antimicrobial resistance.
CDC Activities
Tracking and Data
- Using CDC’s AR Lab Networks to detect known and emerging resistance
- Using CDC’s National Healthcare Safety Network to track and report resistant threats and antibiotic/antifungal use across healthcare settings like hospitals and long-term care facilities
- Leveraging technologies to better understand resistance (e.g., whole genome sequencing)
Preventing Infections and Containment
- Supporting efforts to keep new or rare forms of antimicrobial resistance from spreading through CDC’s Containment Strategy
- Coordinating with local and state public health departments to inform outbreak response
- Providing resources and expertise for outbreak response, infection prevention and control, and laboratory detection of germs
- Providing Infection Control Assessment & Response in healthcare facilities to identify and address gaps in infection control that could lead to the spread of germs
- Working directly with hospitals and clinicians, academic institutions, patients, private industry, and clinical and public health partners to advance research and innovation
Improving Antibiotic and Antifungal Use
- Improving antibiotic and antifungal use across healthcare settings, including telehealth, dental settings, outpatient settings, and STD clinics
- Providing evidence and tools for facilities to implement antibiotic and antifungal stewardship practices and programs
- Identifying new strategies and techniques for improving antibiotic and antifungal use
Additional Work in Progress
- Developing a Center of Excellence for Whole Genome Sequencing, including healthcare-associated germs to help strengthen national One Health tracking efforts
- Doubling investments in state and local health departments to slow emerging antimicrobial resistance and prevent the spread of resistant germs
Examples of CDC Activities in Action
- A 27% reduction of antimicrobial-resistant infections and a 30% reduction in associated deaths from 2012-2017 through hospital infection prevention programs and other activities
- A 5% decrease in outpatient antibiotic prescribing for acute respiratory illnesses (ARIs) from 2011 to 2018
- CDC’s AR Lab Network performed more than 500,000 different tests to track antimicrobial resistance since 2016, and many of these results prompted a containment response
- As of 2019, more than 80% of hospitals reported having an antibiotic stewardship program that met CDC’s Core Elements of Hospital Antibiotic Stewardship
2022 Virtual Public Workshop Cosponsored by FDA & CDC
The Centers for Disease Control and Prevention (CDC) and Food and Drug Administration (FDA) co-sponsored a public virtual workshop on Tuesday, August 30, 2022. The title of the workshop was Drug Development Considerations for the Prevention of Healthcare-Associated Infections (HAIs). Discussions focused on the following topics/areas:
- The current state of development of pathogen-directed products used to prevent healthcare-associated infections
- Evidence supporting decolonization and pathogen reduction (in colonized patients) as a strategy to prevent infection and transmission of antimicrobial-resistant healthcare-associated pathogens
- Antimicrobial resistance threats as potential targets for decolonization and pathogen reduction
- Challenges and potential approaches to drug development and registration of products for the prevention of healthcare-associated infections
You can also view the transcript [PDF – 219 pages] of the workshop.