Action in Communities to Fight Antimicrobial Resistance
Germs, including antimicrobial-resistant germs, spread within our community and sometimes make people sick. Depending on the germ, germs can spread to people through close contact, the air, contaminated water, contaminated surfaces, animals, and sexual contact.
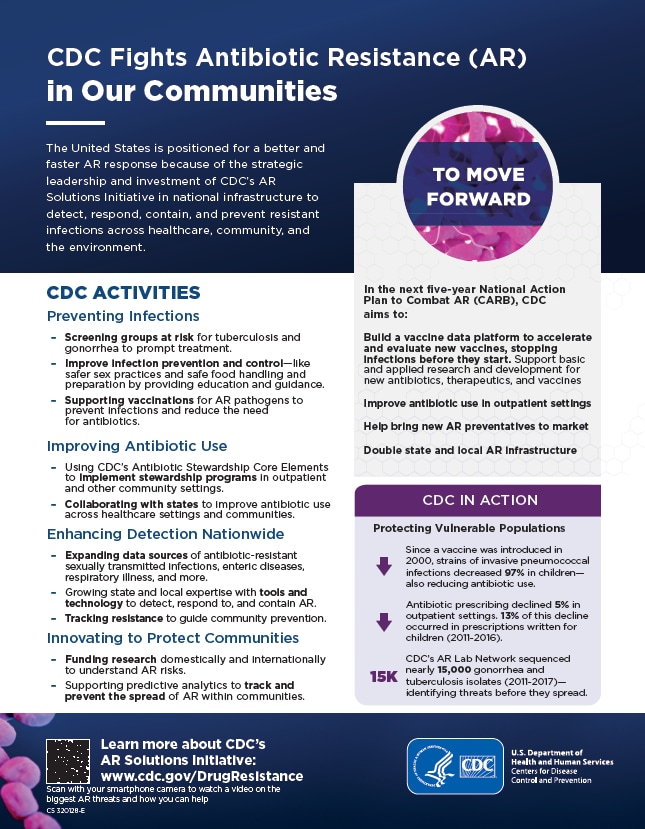
CDC invests in national infrastructure to detect, respond, contain, and prevent resistant infections in community settings to protect people and save lives. Learn more about how resistance can spread and why CDC is concerned about antimicrobial-resistant germs in the community.
CDC implements activities outlined in the U.S. National Action Plan for Combating Antibiotic-Resistant Bacteria, released in 2015 and 2020. These activities are funded through CDC antimicrobial resistance investments, collectively known as CDC’s Antimicrobial Resistance (AR) Solutions Initiative. Through these investments, CDC is transforming how the nation combats antimicrobial resistance.
CDC Activities
Preventing Infections
- Screening groups at risk for tuberculosis and gonorrhea to prompt treatment and prevent resistant infections
- Improving infection prevention and control by providing education and guidance for safer sex practices and safe food handling and preparation
- Supporting vaccinations for specific pathogens to prevent infections in the first place and reduce the need for antibiotics
Improving Antibiotic Use
- Using CDC’s Antibiotic Stewardship Core Elements to implement stewardship programs in outpatient and other community settings
- Collaborating with states to improve antibiotic and antifungal use across healthcare settings and communities
Enhancing Detection Nationwide
- Expanding data sources of antimicrobial-resistant sexually transmitted infections, enteric (gut) diseases, respiratory illness, and more
- Investing in state and local expertise with tools and technology to detect, respond to, and contain antimicrobial resistance
- Tracking resistance to guide community prevention
Innovating to Protect Communities
- Funding research domestically and internationally to understand antimicrobial resistance risks in the community like detecting drug-resistant gonorrhea directly from patient samples to better identify and treat the disease
- Supporting predictive analytics to track and prevent the spread of antimicrobial resistance within communities
Additional Work in Progress
- Supporting the science around alternatives to traditional drugs as another tool to address antimicrobial resistance in the community
- Increasing CDC’s investments in state and local infrastructure to address antimicrobial resistance locally
Examples of CDC Activities in Action
- Strains of invasive pneumococcal infections have decreased 97% in children since a vaccine was introduced in 2000 (achieving high vaccination coverage and encouraging appropriate antibiotic use will slow the spread of pneumococcal resistance)
- A 5% decrease in outpatient antibiotic prescribing for acute respiratory illnesses (ARIs) from 2011 to 2018
- Since 2011, CDC’s AR Lab Network sequenced nearly 38,000 gonorrhea and tuberculosis isolates (pure samples of a germ) providing a better understanding of the threats to help prevent spread