CDC Partners Estimate Healthcare Cost of Antibiotic-resistant Infections
Posted On: April 2021
- CDC teamed up with experts at the University of Utah School of Medicine to estimate that treating six antibiotic resistance threats contribute to more than $4.6 billion in health care costs annually.
- Partnerships like this help CDC gain a better understanding of the impact of antibiotic resistance in healthcare, help clinicians target infection control practices, and support healthcare decision makers to make informed choices that improve patient safety.
- Cost estimates can help guide actions needed to prevent resistant infections.
Each year, more than 35,000 people die because of antibiotic-resistant infections, with more than 2.8 million infections occurring in the United States, according to CDC’s Antibiotic Resistance Threats Report. Many of the germs that cause these infections are frequently found in healthcare settings, resulting in increased risks to patient safety and a burden on the healthcare system as these infections often require substantial healthcare resources to treat.
To better understand the financial burden these infections place on health care, CDC teamed up with experts at the University of Utah School of Medicine and released estimatesexternal icon that treating six alarming antibiotic resistance threats identified by CDC contribute to more than $4.6 billion in health care costs annually.
This is one of the largest studies on healthcare costs associated with treating multidrug-resistant infections to date, encompassing the total costs of medical personnel, equipment, and the space necessary to treat these patients. The estimates do not include other downstream healthcare costs that occur after the first hospitalization or economic impacts to the patients, indicating that the overall costs could be even higher.
Leveraging the existing partnership through CDC’s Prevention Epicenters Program—and resources from the Department of Veterans Affairs (VA) Medical Center and the VA Health Services Research and Development Service—the researchers used methods designed to overcome limitations of previous studies to generate more accurate healthcare costs from antibiotic resistance.
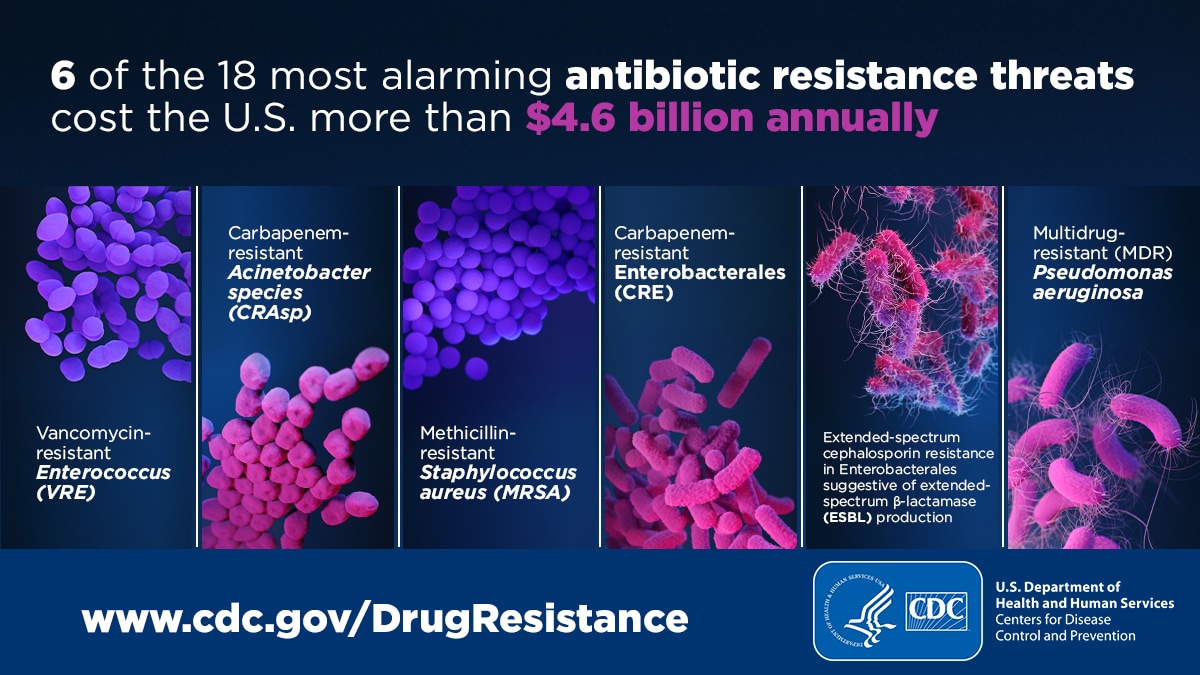
The image shows six of the 18 most alarming antibiotic resistance threats, which cost the U.S. more than $4.6 billion annually. These germs include: Vancomycin-resistant Enterococcus, Carbapenem-resistant Acinetobacter species, Methicillin-resistant Staphylococcus aureus, Carbapenem-resistant Enterobacterales, Extended-spectrum cephalosporin resistance in Enterobacterales suggestive of extended-spectrum β-lactamase (ESBL) production, and Multidrug-resistant Pseudomonas aeruginosa.
The large size of the VA datasets and the detailed information they contained allowed the researchers to isolate cost information specifically attributable to the antibiotic-resistant germs of interest while accounting for the location of the infection in the body and timing of infection while hospitalized. They then multiplied the pathogen-specific cost data by national infection case counts, previously published in the 2019 Antibiotic Resistance Threats Report and Multidrug-Resistant Bacterial Infections in U.S. Hospitalized Patients, 2012-2017external icon to find the estimated total healthcare costs to treat these infections.
Cost estimates like these can help the U.S. Government, healthcare facilities, and other organizations better understand the value of investments to prevent infections and slow the spread of germs. Estimates like these also underscore the healthcare costs associated with these infections and the economic benefits of preventing infections before they start.
CDC has proven that dedicated prevention and infection control efforts are working and are a best buy for public health. Between 2013-2019, investments in these areas have reduced deaths from antibiotic resistance by 18% overall and nearly 30% in hospitals alone.
The University of Utah School of Medicine has partnered with CDC through its Prevention Epicenters Program and Modeling Infectious Diseases in Healthcare (MInD)—innovative research programs with academic investigators to conduct infection control and prevention research—since 2015, collaborating with the VA and its medical centers to explore and implement new prevention strategies and reduce antibiotic resistance transmission (spread) in healthcare.
Partnerships like this one help CDC gain a better understanding of the impact of antibiotic resistance in healthcare, help clinicians target infection control practices, and support healthcare decision makers to make informed choices that improve patient safety.
Learn more about how CDC is collaborating on research pdf icon[PDF – 4 Pages] with partners, including the Prevention Epicenters Program and MInD, to help drive action to combat antibiotic resistance and save lives.