Newly Reported Gene, mcr-1, Threatens Last-Resort Antibiotics
Posted On: 2016
- Through CDC’s Antibiotic Resistance Solutions Initiative, the agency is transforming the nation’s capacity to further detect, respond, and prevent antibiotic resistant threats across healthcare settings and in communities to protect Americans and save lives.
- A new gene known as mcr -1—which can make bacteria resistant to colistin, a last-resort drug for some multidrug-resistant infections—was first reported in China in November 2015 and in the United States in May 2016.
- CDC, FDA, and USDA began searching for mcr -1 in bacterial samples from human, retail meat, and food animal sources. USDA discovered mcr -1 in bacteria from the intestines of two pigs in spring 2016.
- After DoD found that a Pennsylvania patient carried a bacteria with the gene, CDC and state and local health departments in Pennsylvania immediately launched a coordinated public health investigation to potentially prevent mcr -1 from becoming widespread in the United States.
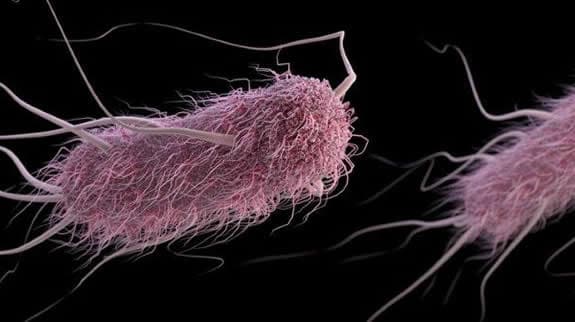
In November 2015, mcr -1—a gene that can make bacteria resistant to colistin, an old antibiotic that is the last-resort drug for some multidrug-resistant infections—was reported in China. The mcr -1 gene is on a plasmid, a small piece of DNA that is able to move from one bacterium to another. The gene has the potential to quickly spread to other bacteria and raises the possibility that bacteria already resistant to major antibiotics could become resistant to colistin as well.
Colistin is a crucial last-resort option. The drug is not frequently used in typical care because of its side effects. Colistin has recently been used, and increasingly, to treat patients with infections caused by multidrug-resistant bacteria against which colistin is still effective, despite its side effects. If colistin resistance spreads to bacteria that are already resistant to all other antibiotics, those bacteria could cause truly untreatable infections. We cannot keep bacteria from changing; bacteria will inevitably find ways of resisting the antibiotics developed by humans. This is why it is more important than ever to slow spread of resistance by following infection control measures for every patient, every time and to keep antibiotics working by improving how we use them.
Transformative Investments Help Us Slow Future Threats
CDC is making transformative improvements using resources provided by Congress in fiscal year 2016 to further identify and respond to new and known antibiotic resistance threats with activities like:
- Antibiotic Resistance (AR) Laboratory Network: Establish seven regional labs with nationwide testing capabilities to track new and emerging AR threats, like “nightmare bacteria” CRE; fill critical public health data gaps; and inform prevention and response in all states and five major cities/territories.
- State Healthcare-Associated Infection (HAI) and AR Prevention Programs: Expand state programs to better respond to outbreaks, improve antibiotic prescribing, and prevent antibiotic-resistant infections across all healthcare settings.
- Whole Genome Sequencing (WGS): Scale up WGS of foodborne pathogens to better understand foodborne resistance patterns and outbreaks, and find new ways to prevent foodborne infections in humans.
CDC Responds
With China’s report, CDC and federal partners began hunting for and tracking mcr -1 in the United States.
Using bacterial samples from human, retail meat, and food animal sources, the CDC, U.S. Food and Drug Administration (FDA), and U.S. Department of Agriculture (USDA) retrospectively screened nearly 55,000 bacterial isolates through the National Antimicrobial Resistance Monitoring System (NARMS) and collections of healthcare-associated bacteria. Screening was done using DNA sequencing and rapid laboratory testing methods. These isolates tested negative for the mcr -1 gene.
However, less than six months after the first identification of mcr -1 in China, the U.S. Department of Defense (DoD) and USDA identified the gene in bacteria cultured from a Pennsylvania patient and retrospectively from the intestinal samples of two pigs, one in South Carolina and the other in Illinois.
After a U.S. resident was found to have a bacterium that contained the mcr -1 gene, CDC and state and local health departments in Pennsylvania immediately launched a coordinated public health investigation.
The bacteria found in the Pennsylvania patient was not resistant to all antibiotics. However, with the gene’s ability to move to other bacteria, including the “nightmare bacteria” carbapenem-resistant Enterobacterales (CRE), CDC launched an urgent public health response to contain and slow any potential spread.
To prevent mcr -1 from becoming widespread in the United States and further threatening antibiotics of last resort:
- CDC, the Pennsylvania Department of Health, and local health departments began identifying and screening close contacts of the patient to determine whether they might carry bacteria with the mcr -1 gene. As of June 29, 2016, 105 contacts were screened; none carried bacteria with the gene.
- CDC issued an alert to notify states, hospitals, and clinical laboratories about the discovery of mcr -1 in the United States. The alert reiterated recommendations for infection prevention, environmental cleaning, laboratory testing, reporting to public health officials, and preparing food safely.
- CDC has also developed and will deploy a rapid laboratory test to help clinical labs find bacteria with the mcr -1 gene.
Preventing & Tracking New Threats
This discovery emphasized the importance of a coordinated public health response, not only to detect new threats like mcr -1, but also to track, slow, and respond to the emergence of antibiotic resistance.
- CDC is working with other federal partners to continue searching for the mcr -1 gene in existing bacterial isolate collections with sophisticated laboratory methods, such as whole genome sequencing, for some isolates.
- Beginning in fall 2016, CDC’s Antibiotic Resistance Laboratory Network will expand nationwide capabilities to combat AR with a network of seven regional labs fully equipped to detect resistance in human samples. State public health laboratories will also be able to detect new forms of antibiotic resistance, like mcr -1, and report these findings to CDC.
- CDC and FDA are curating a colistin-resistance isolate panel of test organisms for the AR Isolate Bank, to challenge and test new diagnostics and therapeutics that can rapidly detect and treat infections caused by resistant bacteria.
- As both government and non-government labs continue to aggressively search for the mcr -1 gene in human isolates, CDC anticipates additional reports of mcr -1 in humans. CDC will continue to work with state and local public health to investigate and respond to these findings to attempt to contain and slow spread of this gene in humans.
Although there is no immediate threat to the public, the discovery of mcr -1 vividly illustrates the many domestic and global challenges facing us as we work to slow the spread of antibiotic resistance and improve antibiotic use. New resistant bacteria continue to emerge with the potential to severely impact our ability to provide medical treatment. The timely investments in the AR Solutions Initiative empower CDC to rapidly detect, investigate, and respond to emerging threats, like mcr -1; prevent resistant infections from occurring and spreading across healthcare settings and the community; and innovate, supporting development of new diagnostics and drugs to test, treat, prevent infections, and save lives.